INTRODUCTION
Acute pancreatitis (AP) is the most common gastrointestinal hospital admission with an incidence of 4.6-100 per 100,000 cases in Europe. 1 Recurrent episodes of acute pancreatitis (RAP) can occur in patients who survive their first admission. Although numerous studies have investigated AP, little research has been performed on the risk of recurrent episodes of AP and the reasons for readmissions after a first AP attack. 2,3,4 Repeated admissions for AP increase hospitalizations and costs; furthermore, RAP is the most important risk factor for progression to chronic pancreatitis with loss of exocrine and endocrine pancreatic functions and, ultimately, pancreatic cancer. 5
Moreover, patients who suffer from several bouts of AP have significantly impaired their health-related quality of life 6 as it has been assessed in quality of life (QOL) scales for RAP patients. 7 Consequently, investigate the course and risk factors for RAP would certainly reduce readmissions, decrease costs, and improve patient’s quality of life.
Data available on the incidence of RAP and predictive factors are scarce and heterogeneous due to differences in study design, variability in follow-up, and no clear consensus in the definition of relapsing. 8-11 In 2018, the American Pancreatic Association published an agreement document for definition and diagnosis of RAP 12 which, undoubtedly, will help researches to contrast their investigations and allow data comparison among centers. The aim of the study is to assess, in our Institution, the rate of RAP and the clinical outcomes in a cohort of RAP patients. We also want to investigate the risk factors of readmissions after a sentinel attack of AP.
PATIENTS AND METHODS
Study subjects
Retrospective single-center study obtained from a prospectively maintained database on AP patients admitted to the Gastroenterology Department of the Hospital Clínico Universitario (Valladolid, Spain). Our hospital is a tertiary, academic center, which serves a population of around 250.000 inhabitants. Patients studied were admitted to hospital between March 2014 and December 2020 and they were followed up until May 2021. For our purpose, patients were assigned into two groups: patients with more than one AP admission (RAP) and patients with a single episode of acute pancreatitis (SAP). Time, reason, number of readmissions, clinical outcomes and severity of the episodes were registered for the patients with RAP.
Definitions
The diagnosis and severity of AP (mild, moderately severe and severe) was carried out according to the revised Atlanta Classification by the International Consensus of 2012. 13
RAP was defined following the International State-of-the-Science Conference Guidelines: a syndrome of multiple distinct acute inflammatory responses originating within the pancreas in individuals with genetic, environmental, traumatic, morphologic, metabolic, biologic, and/or other risk factors, who experienced 2 or more episodes of documented AP, separated by at least 3 months. 12
Exclusion criteria
The exclusion criteria were the following: 1.- Patients who did not sign the informed consent to be included in our database. 2.- Patient admission more than 5 days after the pain onset or patients referred from another hospital. 3.- Patients who could not be followed up. 4.- Patients who died in their first admission. 5.- Patients who suffered from chronic pancreatitis or pancreatic cancer.
Data collection
Clinical, demographic, analytical and radiologic data were recorded which included age sex, body mass index (BMI), Charlson Comorbidity Index, and smoking and alcoholic status on admission. High blood pressure (HBP), diabetes mellitus (DM), and dyslipidemia were also registered. Local pancreatic or peripancreatic complications (fluid or necrotic collections, pseudocyst and walled-off necrosis) were identified. The presence of single of multiple organ failure (respiratory, cardiovascular and renal) was registered according to the modified Marshall score system 14 and was defined as a score of 2 or more for one of those three organs. The etiology of the episode of SAP/RAP was attributed to : 1.- Gallstones (cholelithiasis or choledocholithiasis, or both, found by either transabdominal or endoscopic ultrasound, computer tomography CT, endoscope retrograde cholangiopancreatography ERCP, or magnetic resonance cholangiopancreatograpy MRCP), 2.- Alcohol (alcohol consumption of more than 80 g/d over the previous 5 years) 3.- Post-endoscopic retrograde cholangiopancreatography 4.- Other etiologies (hypertriglyceridemia, pancreatic cancer, chronic pancreatitis, drug-induced…) 5.- Idiopathic (no causative factor was identified).
Statistical analysis
Quantitative variables are presented with mean and standard deviation and qualitative variables according to their frequency distribution. The Kolmogorov-Smirnov test was used to check normality. Pearson’s Chi-square test was used to analyze the association of qualitative variables. In cases where the number of cells with expected values less than 5 was greater than 20%, Fisher’s exact test or the Likelihood Ratio test were used for variables with more than two categories. Comparisons of quantitative values were performed using Student’s t-test for independent samples. Data were analyzed with IBM SPSS Statistics version 24.0 for Windows. Values of p<0.05 were considered statistically significant.
RESULTS
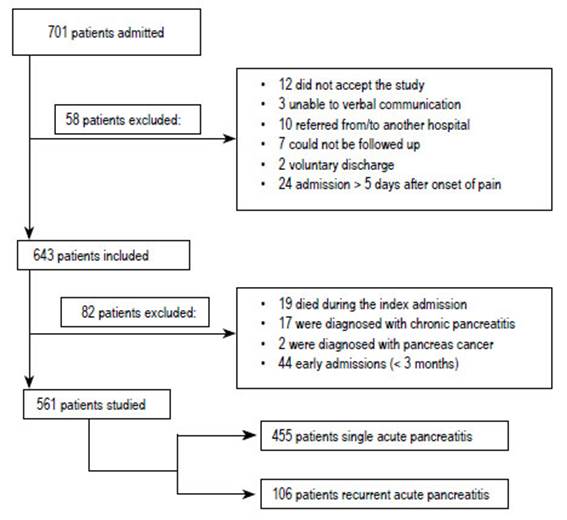
Over the time period considered, 701 admissions for AP were registered in our department. 561 patients were eventually enrolled in the study (Figure 1). 455 of them suffered from a single acute pancreatic event and 106 patients were admitted for two or more episodes of acute pancreatitis (18.9%). Table 1 shows data and outcome parameters of both cohorts.
A total of 154 episodes of RAP were registered. Patients with RAP were 57% females and 43% males, aged 64 ± 20 years. Mean follow-up was 67.63 months (95% IC 65.3-69.95). Most patients suffered from only one episode of RAP (93%); nine patients had 2 relapses, three patients suffered from 3 AP readmissions and four patients experienced 4 bouts of AP. The mean time for the first AP readmission was 10.25 months (95%IC 8.5-11.9), the shortest duration for recurrency was 3.5 months and the longest was 49 months. The etiology of AP did not differ among both cohorts; it was mainly biliary (67% SAP and 57.5% RAP), followed by unknown etiology (18.9% SAP and 25.5% RAP) (Figure 2). Length of hospital stay was similar in both cohorts. Severity, according to modified Atlanta classification, was mild in most of patients who developed SAP and RAP (80,4% and 82%) (Table 1). Of the 154 bouts of RAP, only 15 episodes (9%) were classified as moderately severe/severe in comparison to 108 episodes (19%) in the index attack. 19 patients died in their first AP episode, while only 1 RAP patient died.
Univariate analysis showed that younger age (p 0.004), absence of HBP (p 0.013) and no development of SIRS in the first AP attack (p 0.022) were associated with recurrence of AP. No differences were seen in terms of gender, alcohol and smoking status, BMI, comorbidities, diabetes and dislipemia. There were no statistical differences in relation to outcome measures such as organ failure, ICU admission or drainage of fluid collection and necrosectomy between both cohorts. We found that patients with local complications in their first bout of AP had a tendency to develop RAP (p 0.088) (Table 1). On multivariate analysis younger age was the only single factor related to recurrent episodes of acute pancreatitis (OR 1.015 95% IC 1.00-1.029)
Focusing on the most frequent etiology of RAP which in our series was gallstones (63/106 patients) we analyzed how these patients were managed after their first hospitalization for AP. Forty-four (69,8%) patients did not have a cholecystectomy performed after their first gallstone AP admission. Eight (12%) patients had received a cholecystectomy, one patient ERCP and three patients had cholecystectomy plus biliary sphincterotomy performed at the end of the follow-up period or before recurrence. Five patients did not accept surgical intervention, and two patients were disregarded for surgery due to comorbidities. Table 2 shows management of acute biliary pancreatitis.
When we performed a comparison between both cohorts (SAP and RAP of biliary etiology) including demographic, clinical, analytical and outcome parameters, univariate analysis showed that older age (p 0.017), previous cholecystectomy ( p <0.0001) or cholecystectomy plus biliary sphincterotomy performed ( p <0.0001) were statistically associated with absent of recurrent biliary pancreatitis which were confirmed on multivariate analysis: age OR 0.964 (95%IC 0.946-0.983), cholecystectomy OR 0.075 (95%IC 0.189-0.030) and ERCP+ cholecystectomy OR 0.190 (95%IC 0.219-0.055)
DISCUSSION
In our research, clinical, demographic, etiology and outcome parameters in patients with RAP were studied, and figures were compared with SAP patients.
The term "recurrent acute pancreatitis" was first described in medical literature in 1948, 16 and was accepted during the Marseille symposium in 1963. 17 However, in clinical practice, there has been much ambiguity over the years on the definition of RAP. It was not until 2018, when the International State-of-the-Science Conference established uniform diagnostic, management and definition of RAP by consensus. RAP was therefore considered as 2 or more well-documented separate attacks of AP, with complete resolution for more than 3 months between attacks 12. It is regarded that abdominal pain or elevation of pancreatic enzymes within three months can be attributed to a complication of the first AP episode, rather than a new bout of AP.
There is a lack of research on RAP in literature; however, it deserves especial dedication. Repeated attacks of AP lead to pancreatic fibrosis, chronic pancreatitis and, in the long run, can derive in the development of pancreatic cancer.(5 Moreover, the impact of recurrent bouts of AP, even in the absence of overt chronic pancreatitis, reduces physical and mental quality of life. 7 Change in dietary habits, helplessness, anxiety and fear to suffer another attack, are frequent feelings in these patients. 6
Figures published on RAP are conflicting, with frequencies ranging from 10% to 30% 4,11,19,20. In contrast to our research, some of the previous studies do not clearly defined the diagnostic criteria for RAP 8-10 or do not followed the international consensus guidelines(5,11,18,20 (Table 3). Our rate of RAP, according to the standard definition was 18,9%, like data from the publications(3,19 that also follow the American Pancreatic Association recommendations 12. More than half of our RAP were of biliary etiology (57.5%), resembling data reported from Zhang et. al. 18 and Mallick et al. 20
Unlike some other studies (5, 8), alcohol etiology did not represent a great proportion of RAP in our series (9%); it may be because patients diagnosed with chronic pancreatitis, where alcohol is the main culprit, were excluded from the follow-up. According to several previous research 5,8,19,20 our data also show that younger age is a risk factor of readmission (OR 1.015 95%IC 1.00-1.029) both in global RAP and in biliary RAP. Vipperla et al. 11 in USA, and Gullo et al. 8 in a multicenter European study evidenced a male predominance in RAP patients which was not observed in our cohort. In terms of the outcome measures, we found a slight tendency to have RAP when local complications were developed at the first AP episode (p 0,088); nevertheless, there were no differences in terms of length of hospitalization, UCI admission, organ failure, drainage of collections/necrosectomy, and severity. In contrast, Vipperla et al. 11 noticed that readmission was higher in patients who developed local complications and more severe course at index admission; however, their study included patients readmitted less than one month after discharge. In such a short period of time, a new admission could be considered the same attack, rather than a second episode. Bertilsson et al. 10 also mention that an increased first attack severity was associated with an increased frequency of RAP in all etiology groups; however, a clear definition of RAP is not referred in their text.
An issue of great concern is whether RAP episodes have a worse prognosis than the index attack. In the study by Lee et al. 21 specially designed for this purpose, it was clearly demonstrated that severe outcomes are less frequent in RAP bouts. The researchers claim that a former AP episode is protective against organ failure, intensive care admission, and mortality in the second episode. The authors state that previous acinar necrosis produces a decrease in pancreatic cells with less auto digestion, necrosis and inflammatory response in subsequent attacks. Our results are alike, RAP bouts had milder disease course and less mortality when compared to the index episode of AP. In contrast to some other studies 4,10 where alcohol intake and smoking status were related to RAP episodes, in our series, this association was not found. Currently, there are little research on blood pressure in relation to AP and RAP. Yu et al. 4 did not find association between hypertension and RAP, as could be expected. In our cohort, on univariate analysis hypertension was a protective factor against RAP which could not be found on multivariate analyses.
Special attention must be given to biliary pancreatitis which accounts for more than half of our RAP cases. Gallstones are the leading cause of AP, and cholecystectomy must be performed after the first AP episode. In our series, cholecystectomy alone and/or cholecystectomy plus ERCP were associated with a reduced risk of pancreatitis recurrence (Figure 2). Several societies, including American Gastroenterology Association (AGA) guidelines, strongly recommend cholecystectomy during the index admission(22 or at least within 2-4 weeks after discharge for mild acute pancreatitis 23. It is well established that non-adherence to the guidelines results in subsequent AP readmissions 24. Despite the recommendations, in our clinical setting, as in some other reports 2, we observed a low adherence to guidelines in routine clinical practice; almost 70% of our cohort did not had an early cholecystectomy performed.
The strengths of our study are several: Firstly, we defined RAP according to the state-of-art conference recommendations and early readmissions were excluded; secondly, we presented a large cohort of patients followed over a long period of time, and, finally, patients diagnosed with chronic pancreatitis, with different natural course of the disease, were excluded. However, limitations warrant mention: our database is a prospective one. We performed a retrospective design, which could have led to bias in follow-up. RAP patients admitted at another institution or patients attending only at emergency room without hospitalization, were not considered. Finally, we did not have genetic analysis or performed Oddi sphincter dysfunction tests or microscopic bile crystals detection to better classify idiopathic RAP (25% in our cohort)
In conclusion, our study demonstrates that RAP is a common clinical issue. Younger age was the strongest risk factor for RAP development in our research. Fortunately, repeated episodes of AP have a lower mortality rate and do not follow a more severe course than the index episode. In our series, gallstone accounts for more than half of our RAP. Management of acute biliary pancreatitis in our hospital merits a special mention, as consensus guidelines on early cholecystectomy are not particularly followed. Therefore, we have an important area of improvement in our clinical practice. Adherence to clinical guidelines must be implemented and the results in terms of improving our RAP data should be hence reassessed.