INTRODUCTION
Bile duct stones treatment is usually performed by ERCP (endoscopic retrograde cholangiopancreatography) with balloon or basket extraction 1,2. However, in 10-15% of cases, bile duct stones cannot be extracted using conventional methods 3. This condition is known as dificult biliary stones (DBS). In our hospital, 1,446 ERCPs were performed between 2015 and 2021 and 10.1% corresponded to DBS.
Different types of specialized therapeutic procedures are available for DBS 1. Although the success rates of these procedures in Latin America have been reported 4,5, local Colombian reports are scarce 6. DBS treatment requires expensive technology and highly specialized personnel. Therefore, local studies are required to optimize the resource allocation.
In this study, we describe the clinical characteristics, laboratory findings, ERCP findings, treatments, outcomes, and subsequent treatments performed in patients with DBS treated at a reference hospital in Colombia.
METHODS
A descriptive observational study was conducted including patients with DBS diagnosed at the Hospital Universitario San Ignacio between January 2015 and November 2021. The inclusion criteria were patients older than 18 years, with DBS diagnosis defined as: 1) unsuccessful bile duct clearance by ERCP plus sphincterotomy (associated with a balloon or basket extraction attempt), or 2) disproportion between the size of the distal bile duct and the stone (DBDS), with a difference greater than 2 mm6. The exclusion criteria were pregnancy, altered coagulation or platelet function without an active infectious process, cholecystostomy prior to ERCP, and referral to another hospital. Ethical approval was granted by the Institutional Review board (FM-CIE-0006-22).
Sociodemographic data were collected systematically during patient care. Variables regarding comorbidities, laboratories, ERCP findings, adverse events, Intensive Care Unit requirement, in- hospital mortality, hospitalization length stay and unscheduled readmission in the following 30 days were obtained from electronic medical records. Mortality rate at 6 months was evaluated using the National ADRES database (acronym in Spanish, which translates General Social Security Health System Resources Administrator), a public database which reports mortality date(https://aplicaciones.adres.gov.co/bdua_internet/Pages/ConsultarAfiliadoWeb.aspx).
DBS treatment success was defined as bile duct clearance because of the therapeutic procedure. Procedures available for DBS treatment were Endoscopic Sphincterotomy Plus Large Balloon Dilation (ESLBD) (Boston Scientific CRETM balloon, Massachusetts, United States), Mechanical lithotripsy (ML), (Lithotriptor GF500, G-FLEX, Belgium), Temporary Stent (TS) (FleximaTM, Boston Scientific, Massachusetts, United States), Cholangioscopy-guided laser lithotripsy (CGLL) (Spyglass, Boston Scientific, Massachusetts, United States), or surgery. These procedures were performed according to international guidelines recommendations1. Patients with unsuccessful bile duct clearance after the first ERCP with balloon or basket extraction could be treated with a therapeutic procedure for DBS in the same ERCP time or scheduled at a later visit to receive another therapeutic procedure. The therapeutic procedure selection was decided by the endoscopist.
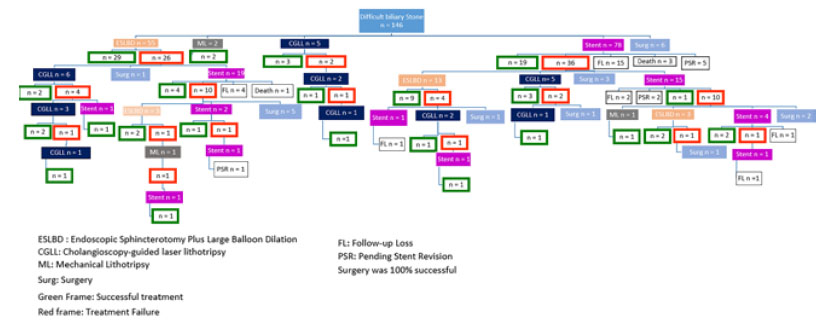
Patients with pending DBS resolution (PDBSR) were defined as patients with DBS who required a new therapeutic procedure but were within the six-month window after the last procedure. Follow-up losses were dened as patients with DBS who required a new therapeutic procedure but did not consult within the next six-month windows after the last procedure. Where possible, telephone follow-up was done to find out if lost patients had been treated at another hospital. Patients who reported extra-institutional DBS treatment were asked to share their clinical record information to determine treatment success. Patients who could not provide extra-institutional clinical records were considered as follow-up losses.
STATISTICAL ANALYSIS
To describe qualitative variables, absolute and relative frequencies were reported. The central tendency and dispersion measures were calculated for quantitative variables. Mean and standard deviation for variables with normal distribution, and median and interquartile range for variables with non-normal distribution. The Kolmogorov-Smirnov test at a significance level of 5% (p<0.05) was used to assess the normal distribution. A descriptive analysis of patients treated with CGLL and comparison between groups with or without complete follow-up was done (Supplementary Table 1. A t-test, Mann Whitney U test, or chi-squared test was used to compare groups according to variable characteristics. Statistical analysis was performed using STATA (Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC).
RESULTS
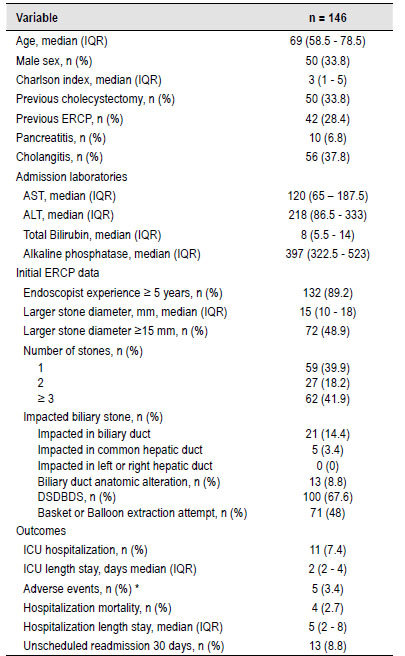
A total 146 patients with DBS were included in this study (Table 1). The median age was 69 years (interquartile range 58.5 - 78.5). Fifty patients (33.8%) were male. The median comorbidity Charlson Index score was 3 (IQR 1 - 5). 42 patients (28.4%) had a previous ERCP and 56 (37.8%) had cholangitis at admission. The median largest stone diameter was 15 mm (IQR, 10 - 18 mm), 72 (48.9%) were ≥15 mm. Of the patients, 39.9% had one stone, 18.2% had two stones, and 41.9% had ≥3 stones. DSDBDS was observed in 100 (67.6 %) patients. Four (2.7%) patients died during hospitalization and 13 (8.8%) had an unscheduled readmission within 30 days.
Table 1 Clinical data, initial ERCP findings, and outcomes in patients with dificult biliary stones.
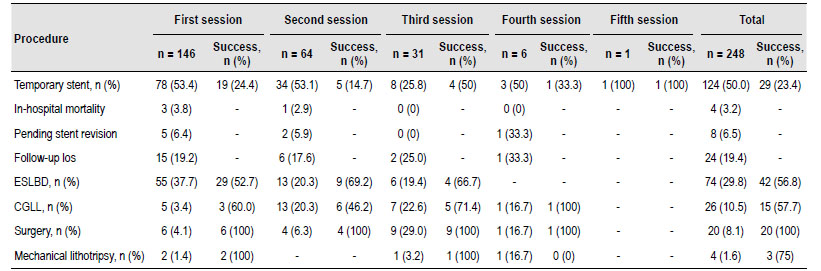
The most commonly used procedures as the first therapeutic option were ST (53.4%) and ESBLD (37.7%). 82 patients (56.2%) had successful DBS extraction in the first therapeutic procedure (after unsuccessful ERCP associated with balloon or basket extraction). 33 (22.6%) patients were successful in the second procedure, 25 (17.1%) in the third, 3 (2.1%) in the fourth, and 1 (0.7%) in the fth procedure. Four (2.7%) patients died during the follow-up period. Eight patients treated with TS (6.5%) were classied as having PDBSR and 24 (19.4%) were lost to follow-up. Supplementary Figure 1 shows a fowchart of the treatments received by patients. Table 2 reports the success rates according to the therapeutic procedures performed. The overall success rates were 56.8% for ESLBD, 75% for ML, 23.4% for TS, 57.7% for CGLL and 100% for surgery procedures (Table 2).
Table 2 Success extraction rate in dificult biliary Stone according to procedure and treatment session.
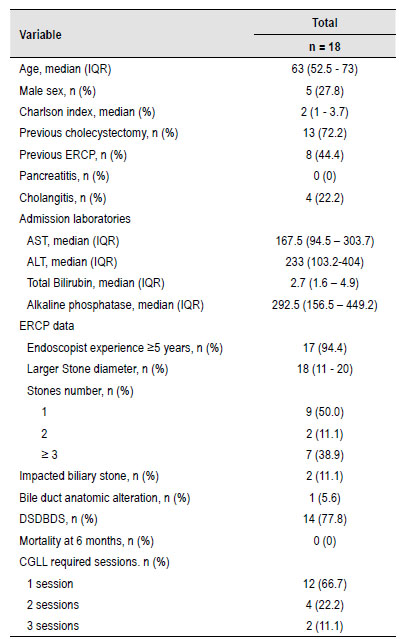
Patients who required at least one session of CGLL had a higher prevalence of previous ERCP (44.4%) and larger stones (18 mm). After successful CGLL, fragments were retrieved with a Dormia Basket (GF1615, G-FLEX, Belgium). The characteristics and outcomes of patients treated with Cholagioscopy Guided Laser Lithotripsy are presented in Table 3).
Table 3 Clinical, sociodemographic, ERCP findings and treatment success rate in patients with dificult biliary stones treated with Cholangioscopy Guided Laser Lithotripsy.
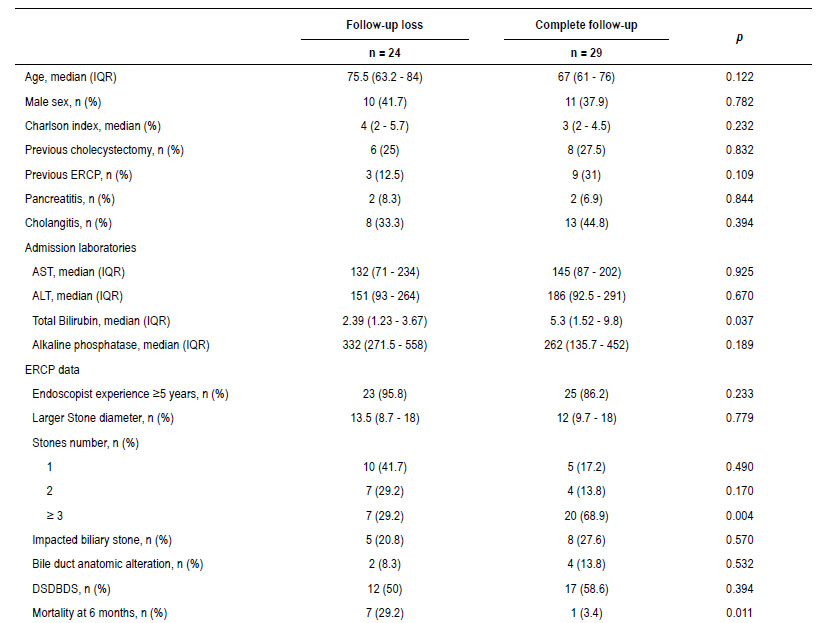
Considering the high frequency of loss to follow-up in the TS group, we compared patients with or without complete follow-up. The group loss to follow-up presented a trend toward older age (75.5 vs 67.0 years, p: 0.122), higher comorbidity (median Charlson index score 4 vs 3, p=0.232) and higher mortality at 6 months (7 vs 1, p=0.011) (Supplementary Table 1).
DISCUSSION
This study describes the clinical characteristics, laboratory findings, ERCP findings, outcomes, and subsequent management in patients with DBS in a reference hospital in Colombia. Our results suggest: 1) >50% of DBS patients had ≥2 common duct bile stones 2) A moderate (50-70%) success rate is expected in the first therapeutic DBS procedure (after failed ERCP), with nearly 50% of patients requiring ≥2 sessions. 3) A moderate success rate of several endoscopic procedures is expected in the next sessions.
We found a moderate success rate in DBS patients treated with ESLBD. Additionally, ESLBD success rate was consistent in different session times (between 52.7 and 69.2%). A 2019 meta-analysis7EMBASE, and the Cochrane Library database to identify relevant available articles until July 19, 2018. Complete common bile duct stone (CBDS reported variable success rates, in a range between 66.7-97.7% in the initial intervention and 29-92% in the following sessions. Success rate variability depended on stones characteristics (mean number of stones between 2 and 4, stone diameter between 10 mm and 16.5 mm) with a lower success rate for stones ≥15 mm 8. Our relatively lower ESLBD success rates could be associated with our larger median stone size (15 mm).
In our study, ML had a 75% DBS success rate. However, only four patients were treated with this procedure. ML has been reported as a therapeutic option for DBS patients. A study reported success rates near to 70% in a single session and 90% in subsequent sessions for stone size diameter ≥15 mm 9. That study reported that unsuccessful ML procedures were associated with a stone diameter of ≥21.9 mm. Other studies reported unsuccessful ML procedures associated to impacted biliary stones, stone size >30 mm or DSDBDS 10. Besides, ML is associated with major complications (basket entrapment or basket fracture). These technical complications can occur in 3.5% of procedures in the bile duct 11. Therefore, in our hospital we prefer ESLBD as a therapeutic option. In conclusion, ML has a moderate success rate and is a good therapeutic option in reference centers with specialized personnel.
Half of our DBS patients were initially treated with TS. The European Society of Gastrointestinal Endoscopy (ESGE) guideline recommends TS as a temporal treatment to relieve biliary obstruction and before a subsequent attempt to stone extraction 1. Evidence suggests that TS exerts a shearing force 12, reducing the volume and number of stones in the common bile duct 13 facilitating next extraction attempts. TS is frequently performed as the first option in our setting because it is readily available and other specialized DBS therapeutic procedures require prior insurance authorization. However, our results showed a low overall TS success rate (23.4%). Prospective studies have reported a TS success rate between 55% 14 and 75% 15, which is higher than our results. Our results may differ because nearly 25% of our patients were PDBSR or follow-up losses. Second, DBS fragile patients could have died o could have been unt for another ERCP 16. That hypothesis is supported by our results: Our lost to follow-up group had a trend toward older age, higher comorbidity, and a higher 6-month mortality rate.
Patients with DBS treated with CGLL presented a moderate success rate, which was consistent across different session times. Maydeo et al. reported a DBS success rate of 77.5% in the first CGLL procedure 17. They also reported a 90% success rate in DBS diameter size between 16 - 30 mm and 65% success rate for stones ≥ 30 mm. Additionally, unsuccessful CGLL procedures were associated with large stones, multiple stones, and patients with a history of previous unsuccessful ERCP. In our study, CGLL was performed in 18 patients in one or more sessions (Table 3 and Supplementary Figure 1). A total of 44.4% of the patients had a history of previous ERCP. The median stone size was 18 mm and half of the patients had ≥2 stones. These factors are related to unsuccessful extraction and may explain our lower success rate. Therefore, CGLL is a useful therapeutic procedure for DBS patients with a stone diameter ≥ 15 mm, multiple stones, or a history of previous ERCP. However, one third of patients will require more than one CGLL session.
In our study, surgery for DBS patients was always successful. Previous studies have reported no mortality or morbidity differences between endoscopic and surgical treatment 18. However, there is a tendency to carry out an endoscopic treatment in choledocholithiasis 19. Therefore, surgery is usually performed in selected patients or after multiple unsuccessful therapeutic procedures. This study reported that only 20 patients required surgery for DBS within 6 years, 70% after unsuccessful endoscopic procedures and 30% as the first therapeutic alternative. Those patients had multiple stones associated with a severe DSDBDS. A medical board, including the surgical team and an experienced endoscopist, made surgical decisions on a case-by-case basis. In conclusion, different endoscopic therapeutic procedures are effective for DBS management. However, surgery may be an option considering the local experience and available resources.
This study describes clinical, sociodemographic and ERCP characteristics and success rates of different therapeutic procedures in a large local DBS cohort. Our data refect the decision-making process faced by an endoscopist in everyday practice. Some limitations, need to be considered: 1) Guidelines have reported different DBS diagnostic criteria based on stone size and bile duct characteristics 1,2 , and different definitions make it difficult to compare the results of different groups. We decided to use a denition that has been used in other studies 17,20 and carefully described the biliary stones and bile duct characteristics to facilitate the comparison of our results with those of other studies 2) Treatment allocation depended on endoscopist criteria. However, there was no difference in the eficacy between the different therapeutic procedures. Therefore, our results represent real world evidence about DBS treatment decisions and could present data to improve subsequent studies.
Our methodology presents a descriptive and retrospective design; therefore, our data should be interpreted as a hypothesis generator and does not demonstrate any therapeutic procedure superiority in DBS patients. Clinical trials are required to compare different treatment options and to assess the best sequential approach. Additionally, TS presented a significant follow-up loss which difficult the success outcome evaluation. Although telephone contact was attempted in these patients, there was a high prevalence of loss to follow-up. Therefore, TS therapeutic procedure data must be carefully considered.
In conclusion, our results suggest a moderate DBS success rate with different alternative therapeutic procedures. However, several treatment sessions are usually required in DBS patients.