INTRODUCTION
Pancreatic cancer (PC) is the eleventh most common cancer in the world, accounting for 4.5% of cancer deaths 1). In Uruguay, the incidence of PC is 10/100,000 inhabitants 2). Its presentation is more frequent in men than in women, with an incidence of 5.5 vs. 4 per 100,000 inhabitants, respectively 1). The standardized mortality rate of PC in Uruguay is 10.44 per 100,000 inhabitants 3).
Eighty percent of cases manifest between the ages of 60 and 80, with presentation before the age of 40 being rare 4,5). However, men present with PC at younger ages and with more advanced stages than women 4).
Ninety percent of pancreatic neoplasms correspond to adenocarcinomas (ADC), while the rest correspond to cystic tumors, neuroendocrine tumors, lymphomas and metastases from other neoplasms 1,6). Regarding its topography, 70% are located at the cephalic level, while 30% at the corporal-caudal level 6). The latter manifest with more advanced stages, liver metastases and peritoneal carcinomatosis 6,3).
Clinically, PC manifests, in order of frequency, with abdominal pain, weight loss, jaundice, anorexia, diabetes mellitus, and steatorrhea. Less frequent is its presentation as migratory thrombophlebitis and gastrointestinal bleeding (HD) (6-8). Colon infiltration by PC is not uncommon and occurs in up to 17%. Clinically, they manifest as intestinal obstruction in 13%, HD in 1.6% of cases, and intestinal perforation, with only 4 case reports 9-11).
HD as a form of presentation of ADC of the pancreas is rare and this complication is associated with a poor prognosis 10). Digestive endoscopy is a useful tool in the diagnosis of HD, since it allows the cause to be identified by taking biopsies 10). According to the reported cases, HD due to PC presents as enterorrhagia and/or melena in 51.1%, hematemesis in 23.4%, drop in hemoglobin (Hb) in 22.3%, and hypotension in 3.2%(10). The main cause of HD due to PC is locoregional involvement of pancreatic head cancer at the gastroduodenal level, manifested as enterorrhagia and melena.
Regarding the prognosis and specic management of HD in this context, data are limited. However, when the bleeding surface is large, especially in cases of tumor invasion, endoscopic hemostasis is generally ineffective 10). Hemostatic radiotherapy may be a therapeutic option in HD due to gastroduodenal tumor invasion, although its efficacy has been poorly described in this context 10).
Computed tomography (CT) with double contrast (intravenous and oral) is the imaging study of choice to confirm the presence of the tumor, evaluate its extension and relationship with the peripancreatic vessels, as well as the detection of metastatic disease 12,13). Although surgery is the only curative treatment for PC, only 10 to 20% of them are resectable 1,2). Most of the distal PCs are unresectable at the time of diagnosis 1,2,14). They usually have an asymptomatic course and easily infiltrate organs and/or blood vessels and generate distant metastases 14). Surgery for palliative purposes it is a therapeutic option in these cases 7,9).
CLINICAL CASE
The case of a 61-year-old man from Montevideo is described. He had a personal history of smoking with a pack-year index of 50 and high blood pressure treated with enalapril 20 mg., every 12 hours. He was admitted to the emergency room due to pain in the flank and left hypochondrium of 2 weeks’ duration, intensity 6/10 (visual analogue pain scale), with irradiation to the back, with a nocturnal component that did not calm down with non-steroidal anti-inflammatory drugs. Concomitantly, loss of 5% of total body weight in 2 months, early fullness, without selective disgust. He presented an episode of enterorrhagia with clots, without hemodynamic repercussion, 72 hours prior to consultation. He had no other clinically evident bleeding.
On physical examination, the patient was awake, hemodynamically stable (blood pressure 140/70 mmHg and heart rate 64 bpm), with no signs of heart failure. Intense pain on palpation of the flank and left hypochondrium, without defense or elements of peritoneal irritation. To assess severity and repercussion of the bleeding, a complete blood count and blood crasis were performed, which highlighted mild normocytic and hypochromic anemia (Hb 10.1 g/dL), without coagulation alterations. Renal function was preserved, so bleeding was classified as minor.
Given the presence of intense abdominal pain with organic characteristics, a CT scan of the abdomen and pelvis was requested, which revealed the presence of a hypodense mass measuring 90 x 67 x 69 mm (L, T and AP) at the level of the tail of the pancreas (Figure 1). In the lower sector and behind it was in close relationship with the anterior pararenal fascia and with the splenic angle of the colon, observing air bubbles at that level, which suggested continuity with the colonic lumen (Figure 2). Hepatic lesions and a left adrenal mass were identified as elements of distant dissemination. The evaluation of the focal hepatic lesions was complemented with nuclear magnetic resonance (NMR), which confirmed their secondary nature.
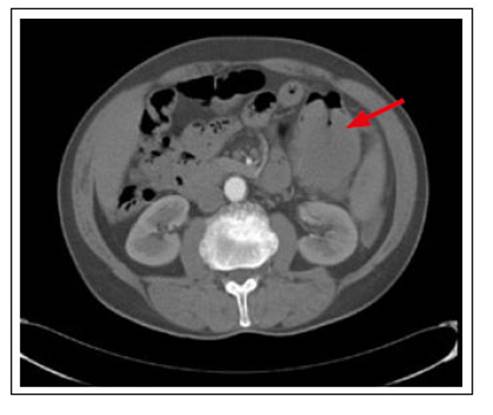
Figure 1 CT of abdomen and pelvis. Neoplasm of the tail of the pancreas in close relationship with the left angle of the colon (red arrow).
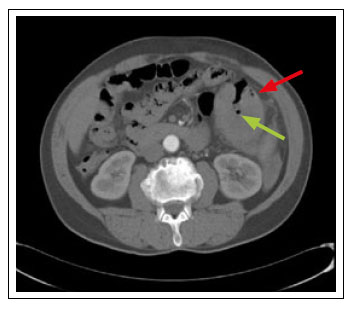
Figure 2 CT of abdomen and pelvis. Neoplasm of the tail of the pancreas with air bubbles inside (green arrow) and infiltration at the level of the splenic exure of the colon (red arrow).
Given the colonic compromise due to the lesion described in the abdominal CT, the assessment was started with video colonoscopy (VCC). At 35 cm from the anal margin, there was evidence of circumferential mucosal involvement with intense edema, erythema, friability, and spontaneous bleeding. It presented sectors of violaceous-black mucosa as usually seen in ischemic involvement (Figure 3). Biopsies were taken for histological study and were not continued proximally due to the risk of iatrogenesis. Pathological anatomy revealed colonic mucosa infiltrated by poorly differentiated solid pancreatic neoplasia. The histological subtype corresponded to ductal type ADC with cellular pleomorphism, cordonal solid architecture with few tubules (Figure 4 and 5).
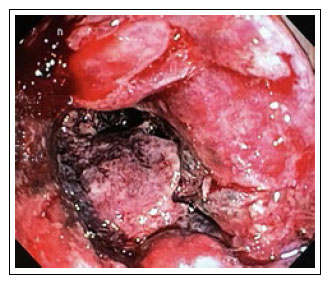
Figure 3 Colonoscopy. At splenic flexure of the colon, mucosa with great edema, erythema and spontaneous bleeding. Mucosa of blackish-violet appearance.
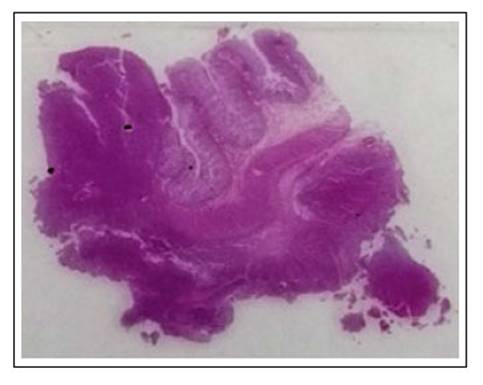
Figure 4 H&E histological slide. Resected colonic segment showing tumor infiltration from the serosa to the mucosa of the organ.
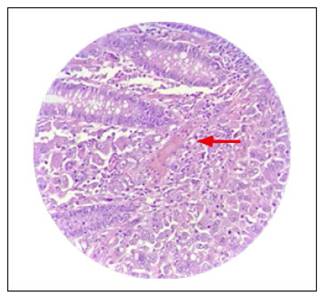
Figure 5 H&E 40X. Poorly differentiated adenocarcinoma replacing the submucosa (arrow) and invading the lamina propria mucosa between native glands.
With a diagnosis of stage IV pancreatic tail neoplasm with colon involvement, (TNM), palliative surgical treatment was considered. In the preoperative assessment, the patient presented a new episode of bleeding with a progressive decrease in Hb to 7.3 g/dL. Two volumes of red blood cells were transfused and a palliative corporal-caudal pancreatectomy with splenectomy and en bloc resection of the splenic flexure of the colon and left adrenal gland with end colostomy was performed. The anatomy of the surgical piece confirmed 10.5 cm moderate to poorly differentiated ductal ADC of the pancreas that infiltrated the colon and left adrenal capsule with 11 lymph nodes and 2 metastatic.
As a postoperative complication, he presented two retroperitoneal collections that required percutaneous drainage with a positive culture for Enterobacter cloacae complex. Broad-spectrum antibiotic treatment was given, with poor evolution, and the patient died 3 months after surgery.
DISCUSSION
In the present case, the diagnosis of pancreatic tail cancer was reached in a patient who presented with enterorrhagia associated with intense pain in the hypochondrium and left flank of organic characteristics, with irradiation to the back and general repercussion.
Worldwide, the incidence is higher for men than women (5.5 vs 4.0 per 100,000, respectively), however, in Uruguay it is the same for both sexes 1,2). In the present case, the diagnosis was made at 61 years, which is consistent with what is reported in the literature, being more frequent in people over 55 years of age with the peak incidence at 70 years of age 1,2).
The most frequent involvement of PC is at the level of the head and uncinate process (60-70%), in this case the location was at the level of the tail, this being infrequent (10-15%) 1,2,14). According to a cohort study led by Beetz et al., the clinical presentation with abdominal pain and weight loss are the most frequent symptoms reported, with a frequency of 68.1% and 39.4%, respectively 7).
Gastrointestinal bleeding due to cephalopancreatic involvement can manifest as melena or enterorrhagia and, less frequently, hematemesis 10). These manifestations are due to gastroduodenal involvement, reported in the study by Ohtsubo et al. involvement of the duodenal bulb in 10% of patients with cephalic PC and 65% in the second duodenal portion 15).
Although it has been reported that PC can infiltrate the colon in 17% of cases, HD due to its infiltration is extremely infrequent, accounting for 1.6% 9). It corresponds to a severe form with an ominous prognosis such as it was in this case 10,15). Clinically, the patient did not present hemodynamic repercussion, which is consistent with the reports that showed arterial hypotension in only 3.2% 10).
Unresectability of distal PC is the norm at diagnosis 1,2,14). In the vast majority, due to infiltration of adjacent organs, as well as invasion of blood vessels and distant metastases 1). The presence of peritoneal carcinomatosis, lung and liver metastases stage the patient in stage IV, according to the Union for International Cancer Control (UICC)(2). Locoregional and distant involvement of the patient was clearly evidenced by colonic and anterior pararenal fascia infiltration, as well as the presence of liver and adrenal metastases, respectively. This coincides with a national study, led by López et al. where 43% of the patients were diagnosed in stage IV, of which 92% of the cases the stage marker was the presence of liver metastases 2). In the reported case, staging by chest CT or bone scan was not continued due to evidence of advanced disease, with poor short-term survival.
PC treatment is multidisciplinary, with the participation of surgeons, endoscopists, radiologists, and oncologists. Although surgery is the only purportedly curative treatment for PC, only 10 to 20% of these are resectable 1,2). Palliative treatment is the treatment of choice in patients with locoregional, large-vessel involvement, pulmonary, hepatic, and peritoneal metastatic disease 2). In the reported case, given the presence of PC complicated by gastrointestinal bleeding, palliative surgical treatment with corpocaudal pancreatectomy was chosen, en bloc resection of the splenic flexure of the colon, left adrenal gland, and splenectomy with end colostomy. The surgical piece corresponded to a poorly differentiated ADC, which is consistent with the literature where 90% of pancreatic neoplasms correspond to ADC 1,6).
Multivisceral resection for ADC of the advanced tail of the pancreas is justified, since it does not increase mortality and can even prolong long-term survival, with an increase in postoperative morbidity 7). In the reported case, the patient presented multiple post-surgical collections that required percutaneous drainage, which caused an increase in morbidity and mortality, dying 3 months later due to said complication. In a cohort study by Beetz et al. postoperative complications were observed in a third of the patients. Surgical reintervention was required in 8.5% cases and percutaneous drainage in 77% of the patients who presented fistulas and/or collections. Six percent of the patients died in the immediate postoperative period.(7 The estimated median survival after multivisceral surgical treatment for PC that was supposedly curative was 12.7 months with survival rates at 1, 3 and 5 years of 53.2%, 15.8% and 9%, respectively 7). However, the mean survival of metastatic patients in a Uruguayan study was 2 months with various palliative therapies 2). This coincides with the 3-month survival presented by the patient, possibly linked to post-surgical complications. In cases of unresectable disease, the median survival is around 7 months 7).














