INTRODUCTION
Gastroesophageal reflux disease (GERD) is a pathology that develops when gastric acid reflux causes symptoms, such as heartburn or regurgitation, and objective evidence of the disease, such as erosion or metaplasia of the esophageal mucosa, peptic stenosis, or abnormal exposure to gastric acid 1,2. In Latin America, the estimated prevalence ranges between 11.9% and 35%, according to a meta-analysis carried out in 2011 3. Prevalence in northern Peru was found to be around 26.5% 4, being comparable with the prevalence of North America and Europe 5. The clinical presentation of GERD is divided into typical (heartburn or regurgitation) and atypical (cough, dysphonia, dysphagia, wheezing, and other extra-esophageal symptoms) 6. The therapeutic management of GERD consists of suppressing gastric acid secretion and begins in a staggered manner, with low initial doses of proton pump inhibitors (PPIs), increasing progressively according to the persistence of symptoms. It is common, however, that a significant percentage of patients have a partial response or are refractory to treatment, even with maximum daily doses of PPIs 7.
Refractory GERD is defined as the persistence of symptoms despite receiving a maximum dose, in one or two doses a day of PPIs for a period of at least 8 to 12 weeks with objective evidence of GERD 7,8. This term encompasses a heterogeneous group of people, who may differ in the frequency and severity of symptoms, response to treatment, and dose of PPIs; hence it is a phenomenon determined by the individual characteristics of each patient. It is estimated that a failure to control symptoms occurs in a range of 10 to 45% of patients 8,9, however, this percentage is variable between studies; probably due to the use of different definitions, PPI doses, and unequal groups of subjects 10. The first step in the management of suspected refractory GERD is to optimize treatment with PPIs, which should be taken between 30 to 60 minutes before meals to provide better control of the pH of the acid, compared to administration during or after 11. If symptoms persist, a change from PPI -omeprazole to lansoprazole, for example- can be considered a strategy associated with an improvement of symptoms in approximately 20% of patients 12.
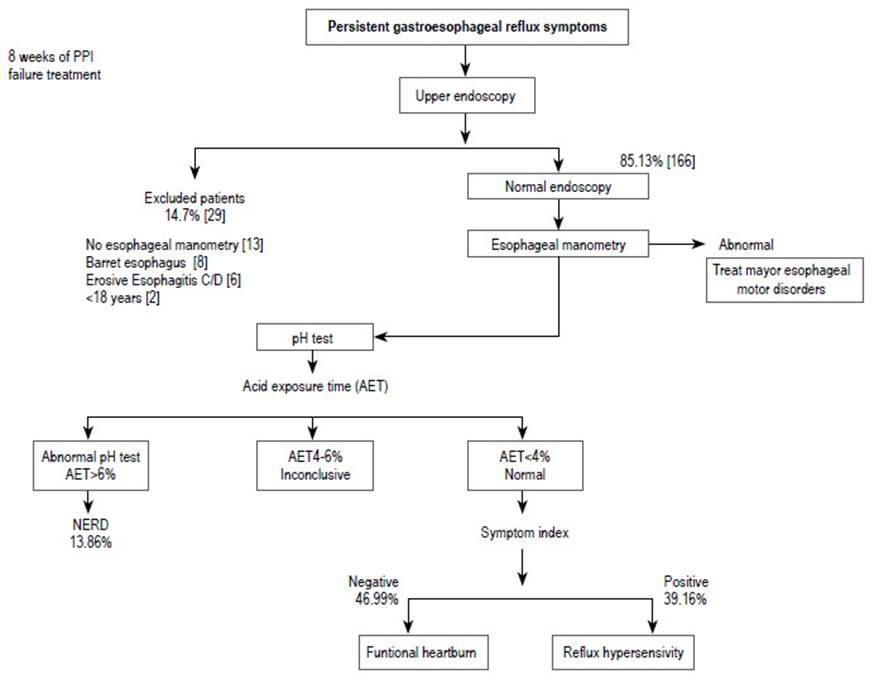
Patients with persistent symptoms despite optimization of PPI therapy require many additional diagnostic methods to rule out inadequate acid suppression, conditions that alter esophageal motility or integrity, or functional disorders. A digestive endoscopy should be performed first, to directly visualize the esophagus and rule out conditions that alter esophageal integrity, such as erosive esophagitis grade C or D according to Los Angeles classification, eosinophilic esophagitis, and Barrett’s esophagus 8, these being confirmatory of the diagnosis of GERD according 2,13. If to criteria established in the Lyon consensus esophageal lesions are not observed by endoscopy, an event that occurs approximately 70% of the time 14, nonerosive reflux disease (NERD) is suspected, which is the most common manifestation of GERD 5. The next step is to monitor reflux through esophageal pH-impedance measurement, which allows quantifying reflux in addition to measuring its pH 8. This procedure is performed in an outpatient manner and consists of placing a trans nasal catheter 5 cm above the lower esophageal sphincter, for 24 hours and is the only method that allows detecting the number of reflux episodes, both acidic (pH <4) and nonacidic (pH> 4), time of exposure to acid and its correlation with the patient’s symptoms. The diagnosis of true nonerosive reflux disease is confirmed in patients who have an abnormal reflux exposure (pH <4 and an exposure time greater than 6% for 24 hours), while in patients who have persistent symptoms with exposure to acid in normal ranges, the diagnosis of functional disorders should be considered 14,15.
Approximately 60% of patients who undergo esophageal pH-impedance testing suffer from functional esophageal disorders, up to 36% suffer from esophageal hypersensitivity, and 24% from functional heartburn, according to studies that calculated their prevalence 16,17. These conditions are not found within the definition of gastroesophageal reflux disease but manifest as reflux symptoms refractory to treatment 8. Both are diagnosed using the Rome IV criteria; an international consensus that represents an effort to establish, based on updated scientific evidence, diagnostic criteria for functional gastrointestinal disorders also known as alterations of the brain-gut axis 18. Esophageal hypersensitivity is a condition characterized by symptoms associated with exposure to non-acid gastric reflux (pH> 4). These patients have a positive correlation between reflux episodes and symptoms, with acid exposure within physiological ranges (less than 4% of the time of day). In these patients, mild or non-acid reflux and esophageal distention due to gas regurgitation are the causes of symptoms 19. Esophageal motility was classified as normal or ineffective. Within the esophageal pH-impedance findings, the percentage of time of exposure to acid (TEA) was considered; being pathological when greater than 6%, indeterminate when ranged between 4 to 6%, and physiological when less than 4%; the total number of reflux episodes per day, was considered pathological when more than 80 episodes, indeterminate when ranged between 40 to 80, and physiological when less than 40. In patients who had persistent symptoms despite optimal therapy, in addition to endoscopy without abnormal findings and exposure to gastric acid in physiological ranges, the diagnosis of functional disorders was established. Patients with pathological acid exposure were diagnosed as having true non-erosive reflux disease. To differentiate between functional heartburn and esophageal hypersensitivity, the association variables were considered: symptom index (the percentage of symptomatic events preceded by reflux episodes, considered positive when greater than 50%) and the probability of symptom association (probability of association between symptoms and reflux episodes considered positive when greater than 95%). Patients with functional disorders who had any of the positive symptom association variables were diagnosed with esophageal hypersensitivity, the rest were considered to have functional heartburn 2.
To establish the diagnosis, all the Rome IV criteria for esophageal hypersensitivity must be met: the onset of symptoms should be at least 6 months before diagnosis and for the last 3 months, retrosternal burning, normal endoscopy without evidence of eosinophilic esophagitis, absence of a major disorder of esophageal motility and evidence that the symptoms are triggered by reflux events, despite a normal exposure to acid evidenced by pH-impedance measurement 20,21. On the other hand, functional heartburn is a condition in which the persistence of symptoms does not present a positive correlation with episodes of reflux (acid or non-acid). Unlike esophageal hypersensitivity, in these patients, there is no association between symptoms and reflux episodes, and an augmented sensitivity to chemical or mechanical stimuli has not been demonstrated 22. To establish the diagnosis, all the Rome IV criteria for functional heartburn must be met: the onset of symptoms should be at least 6 months before diagnosis and for the last 3 months, retrosternal burning, absence of symptom relief despite optimal PPI therapy, absence of evidence that gastroesophageal reflux or eosinophilic esophagitis is the cause of the symptoms and the absence of a major esophageal motor disorder 20,21. The management of esophageal hypersensitivity and functional heartburn is different from that of conditions caused by reflux in pathological ranges (GERD and NERD) since the main objective is not necessarily to reduce acid secretion, but rather to modify the perception of symptoms through the adjuvant use of neuromodulators, such as serotonin reuptake inhibitors or tricyclic antidepressants, which confer a visceral analgesic effect, acting on a central nervous system level or the afferent pain pathways 10,23. Furthermore, since patients with a diagnosis of esophageal hypersensitivity present symptoms that are triggered by episodes of reflux -within normal ranges-, they may be candidates for surgical management 24.
Gastroesophageal reflux disease is costly. In the United States, the annual budget for the diagnosis and management of GERD exceeds USD 12 billion 25. Furthermore, refractory reflux symptoms are associated with a poorer quality of life, decreased physical and mental functionality, and work productivity 26. In Peru, the burden of this disease has not been calculated, but it could be assumed that it also represents high public spending and a poorer quality of life for patients.
Aims
Primary aim: to calculate the frequency of esophageal hypersensitivity and functional heartburn in patients with refractory reflux symptoms using the Rome IV international consensus and an algorithm of diagnostic procedures in patients from three fully equipped private hospitals in Metropolitan Lima, Peru.
Secondary aim: to contrast the demographic, clinical characteristics, and procedure results from the patients with the established diagnoses.
MATERIALS AND METHODS
A retrospective cross-sectional study was conducted, which corresponds to a database analysis from three private clinics in Lima to determine the frequency of functional heartburn and esophageal hypersensitivity in a population of patients with refractory gastroesophageal reflux symptoms. Patients had a previous upper gastrointestinal endoscopy and underwent esophageal manometry and esophageal pH-impedance analysis. The procedures were performed by three gastroenterologists in each of the participating hospitals in the study in the 2018-2021 period. Patients with findings of erosive esophagitis C or D according to the Los Angeles classification, adenocarcinoma, or Barrett’s esophagus were excluded, in addition, patients who presented major motility disorders according to the Chicago V4 classification evidenced through esophageal manometry were excluded.
Sample size
Power was calculated with the available sample size, 83 women and 83 men with refractory reflux symptoms, using a 95% confidence interval. Frequencies of functional heartburn reported by Savarino et al. (2012) 16 were used, which were 69.6% in women and 30.4% in men, and the power of the study was calculated to be 99.93%.
Variables
Demographic variables of age and sex were considered, as well as the symptoms presented by the patients, classified as typical (heartburn and regurgitation) and atypical (cough, dysphonia, dysphagia, wheezing, and other extra-esophageal symptoms). Within manometry findings -according to the Chicago classification, the morphology of the Gastroesophageal Junction (GEJ) was included, as it contrasts the relative location of the two contractile elements (lower esophageal sphincter and the crural diaphragm) and classifies it into three GEJ subtypes: GEJ type I (overlapping), GEJ type II (axially separated by less than 3 cm) and GEJ type III (separated by more than 2 cm). The tonicity of the esophageal sphincter was also evaluated and could be classified as hypotonic, competent, or hypertonic. Esophageal motility was classified as normal or ineffective. Within the esophageal pH-impedance findings, the percentage of time of exposure to acid (TEA) was considered; being pathological when greater than 6%, indeterminate when ranged between 4 to 6%, and physiological when less than 4%; the total number of reflux episodes per day, was considered pathological when more than 80 episodes, indeterminate when ranged between 40 to 80, and physiological when less than 40. In patients who had persistent symptoms despite optimal therapy, in addition to endoscopy without abnormal findings and exposure to gastric acid in physiological ranges, the diagnosis of functional disorders was established. Patients with pathological acid exposure were diagnosed as having true non-erosive reflux disease. To differentiate between functional heartburn and esophageal hypersensitivity, the association variables were considered: symptom index (the percentage of symptomatic events preceded by reflux episodes, considered positive when greater than 50%) 27 and the probability of symptom association (probability of association between symptoms and reflux episodes considered positive when greater than 95%). Patients with functional disorders who had any of the positive symptom association variables were diagnosed with esophageal hypersensitivity, the rest were considered to have functional heartburn 2.
Procedures
Once the protocol was approved by the Institutional Ethics Committee of Universidad Peruana Cayetano Heredia, access was requested to diagnostic procedures reports from San Felipe, El Golf and Internacional private hospitals, located in Lima. Information was obtained from esophageal pH-impedance and high-resolution esophageal manometry procedures, which were performed in patients who presented persistence of symptoms despite treatment with proton pump inhibitors for a minimum of 8 weeks. Codes were assigned to each patient to maintain the anonymity of each one of them. Estimation of the power of the sample was carried out with OpenEpi software (developed by Andrew G. Dean and Kevin M. Sullivan, Atlanta, Georgia, USA). The information collected was stored in a database in Microsoft Excel (developed by Microsoft Corporation, Redmond, Washington, USA). Subsequently, the information was analyzed using the software STATA version 17 (developed by StataCorp LLC, College Station, Texas, USA).
Statistical analysis
Descriptive analysis was performed using patients with suspected NERD as the total number and the two separate clinical conditions expressed as proportions: esophageal hypersensitivity and functional heartburn, obtaining frequencies for each clinical condition. Sociodemographic variables were described in percentage frequencies for qualitative figures, and quantitative variables were described using means and standard deviation. A bivariate analysis was carried out to determine the associations between clinical conditions and the different variables and it was determined using an odds ratio and a confidence 8 weeks of PPI failure treatment interval of 95%. Chi-square test was used to describe categorical variables and t-test was used to compare groups, the level of significance was considered by a p-value below 0.05.
RESULTS
A total of 195 reports of patients presenting with persistent gastroesophageal reflux symptoms (with at least 8 weeks of proton pump inhibitor treatment without response) were reviewed. The reports included information on upper gastrointestinal endoscopy, esophageal manometry, esophageal pH-impedance measurement, and demographic information on the patients such as age and sex. Fourteen patients were excluded for not having esophageal manometry: eight for having a diagnosis of Barrett’s esophagus, six for presenting erosive esophagitis C or D according to the Los Angeles classification. Another two, for being under 18 years of age. By total, the present study included 166 patient reports: 83 men and 83 women (Figure 1). The means (n, [± standard deviation]), odds ratio (95% CI), and frequencies (n, [%]) for each condition were calculated.
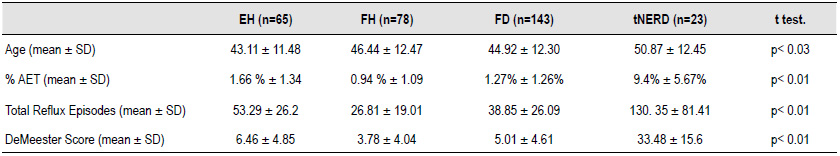
One hundred forty-three (86.1%) patients were diagnosed with functional disorders; 78 patients with functional heartburn (46.9%), 65 with esophageal hypersensitivity (39.2%) and 23 with true non-erosive reflux disease (13.9%). The most frequently reported symptoms were heartburn (59%) and belching (56%). The mean age was 45.75 (± 12.46), time of exposure to acid was 2.39% (± 3.69), and 51.52 (± 49.75) for the number of reflux episodes. In addition, 27 (16.27%) of patients presented the additional diagnosis of supragastric belching (Table 1).
Table 1 Basal characteristics of the study population.
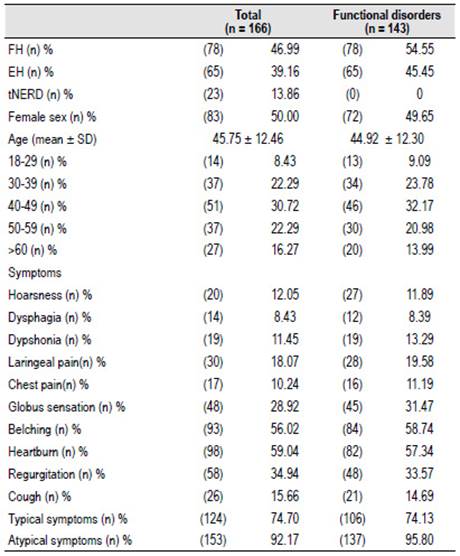
FH: Functional heartburn EH: Esophageal Hypersensitivity tNERD: True nonerosive reflux disease SD: Standard deviation Typical symptoms: at least one (heartburn or regurgitation)
In the group of patients diagnosed with functional heartburn, the mean age was 46.44 years (± 12.47), the meantime of exposure to acid was 0.94% (± 1.09) and the mean number of reflux episodes was 26.81 (± 19.01). A positive association was found with the symptoms of hoarseness (OR = 2.99; 95% CI [1.09-8.21] p <0.03) and dysphonia (OR = 5; 95% CI [1.58-15.79] p <0.01). A greater probability of presenting atypical symptoms was observed (OR = 5.43; 95% CI [1.16-25.31] p <0.02). No association was found with either age or sex of the patients. Regarding the manometric findings of patients with functional heartburn, a positive association was found with GEJ type I (OR = 2.77; 95% CI [1.37-5.56] p <0.01) and with preserved esophageal motility (OR = 2.15; 95% CI [1.14-4.07] p <0.03). Within the pH-impedance findings, a positive association was found with many reflux episodes of less than 40 (OR = 9.23; 95% CI [4.55-18.70] p <0.01), which is considered within the physiological range, and a negative association with a number between 40 and 80 reflux episodes (OR = 0.36; 95% CI [0.19-0.69] p <0.01), which is within the indeterminate range to determine pathological reflux according to the Lyon consensus (Table 2).
Table 2 Multivariate analysis of predictors of occurrence of non-erosive reflux disease and functional disorders.
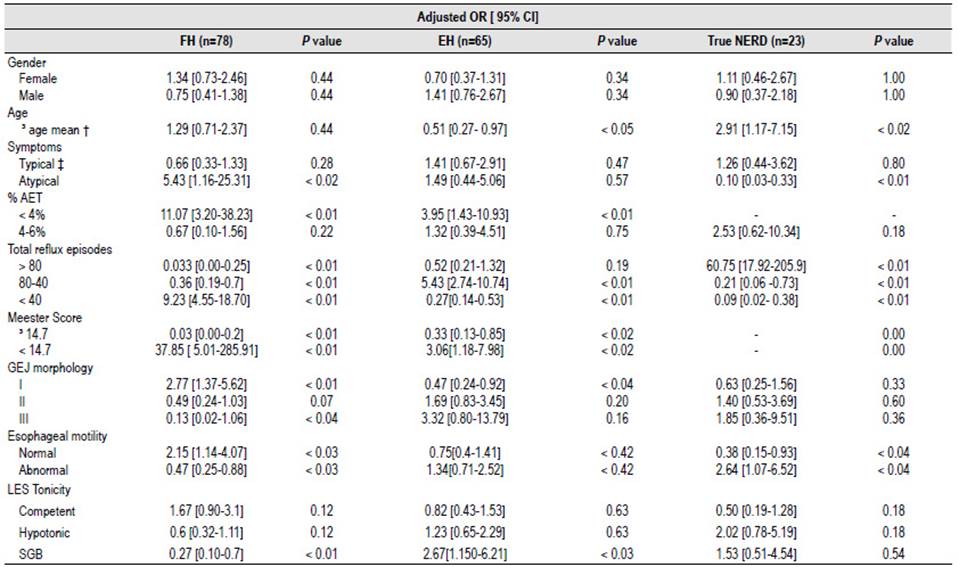
OR: odds ratio FH: functional heartburn, EH: esophageal hypersensitivity, true NERD: true non-erosive reflux disease, %AET: acid exposure time, SGB: supragastric belching, GEJ: gastroesophageal junction, LES: lower esophageal sphincter.
† Age mean (years): Functional heartburn = 46.44; esophageal hypersensitivity = 43.11; Non erosive reflux disease = 50.87.
‡ Typical symptoms = heartburn and regurgitation.
In the group of patients with esophageal hypersensitivity, the mean age was 43.11 years (± 11.48), the mean time of exposure to acid was 1.66% (± 1.34) and the mean number of reflux episodes was 53.29 (± 26.2). Also, belching (OR = 3.12; 95% CI [1.59-6.09] p <0.01) and regurgitation (OR = 2.23; 95% CI [1.16-4.29] p <0.02) were the symptoms with a positive symptom association. No association was found with the sex of the patients. Among the manometric findings and esophageal pH-impedance measurement, unlike the functional heartburn group, negative associations were found with GEJ type I (OR = 0.47; 95% CI [0.24-0.92] p <0.04) and with a number of reflux episodes of less than 40 (OR = 0.27; 95% CI [0.14-0.53] p <0.01); in addition to a positive association with reflux episodes in an indeterminate range of 40 to 80 (OR = 5.24; 95% CI [2.7410.74] p <0.01). In these patients, a greater probability of presenting the diagnosis of supragastric belching was found (OR = 2.76; 95% CI [1.15-6.21] p <0.03) (Table 2).
In the group of true non-erosive reflux disease, the mean age was 50.87 (± 12.45) years, and the difference with the mean age of the group of patients with functional disorders (44.92 ± 12.3) was statistically significant (p < 0.03). The mean time of acid exposure was 9.39% (± 5.67) and the mean number of reflux episodes was 130.35 (± 81.41) (Table 3). No association was found with sex but there was a positive association for the mean age, with patients aged 50.87 years and older being more susceptible (OR = 2.89; 95% CI [1.17-7.15] p <0.02). Patients who had at least one atypical symptom were less likely to present true non-erosive reflux disease (OR = 0.10; 95% CI [0.02-0.33] p <0.01). Within the manometry and pH-impedance findings, a higher risk of presenting true non-erosive reflux disease was observed in patients who had ineffective esophageal motility (OR = 2.64; 95% CI [1.07-6.52] p <0.04) and lower risk in patients who presented some reflux episodes in the indeterminate range (40 to 80) (OR = 0.21; 95% CI [0.060.38] p <0.01).
DISCUSSION
The main objective of the study was to evaluate the frequency of functional diagnoses in a group of patients who presented reflux symptoms refractory to medical treatment for at least 8 weeks. A frequency of 86.15% was obtained for all functional disorders, being 46.9% for functional heartburn and 39.2% for esophageal hypersensitivity. In comparison, previous studies have reported frequencies of approximately 60% for functional disorders 16,17, however, the prevalence of these has not been studied in-depth in our population, this difference could be attributed to cultural factors and the fact that this study was carried out in an urban setting, where a higher frequency of GERD has been reported. The remaining 13.9% were diagnosed as true non-erosive reflux disease, because all of them had an intact esophageal mucosa (without the presence of Barrett’s esophagus, peptic stricture, or erosive esophagitis Los Angeles C or D) and exposure to acid in pathological ranges according to the criteria established in the Lyon consensus. It considers time exposure to acid (greater than 6% of the day), some acid reflux episodes (greater than 80 episodes), and abnormal findings on high-resolution manometries, such as hypotension of the lower esophageal sphincter, esophageal hypomotility, or hernia Hiatal 2. A diagnosis that had not been considered was supragastric belching (swallowing air to induce belching), however a frequency of 16.27% was reported, this could represent a mechanism that would contribute to a greater total number of reflux episodes 28. The mean age of patients with refractory symptoms to treatment was 45.75 ± 12.46 years, and it has been previously described that the Hispanic population is more likely to present them despite treatment with PPIs 29. This is relevant since this is the main population in Peru and the mean age represents the bulk of the economically active population, therefore it can be assumed that the burden of functional esophageal disorders is high. The conditions that can present as refractory reflux symptoms are greatly underdiagnosed in our setting, mainly due to a lack of awareness and an insufficient number of the required diagnostic tools.
The non-pathological exposure to acid (an exposure time of less than 4% and reflux episodes less than 80 per day) without a positive association between the symptoms and the recorded reflux episodes established the diagnosis of functional heartburn according to the Lyon and Rome IV consensus 2,18. In this group, the meantime of acid exposure (0.94%) and the mean number of reflux episodes (26.81) was within the range of non-pathological exposure to acid. This group was more likely to present dysphonia, which may be an atypical symptom associated with GERD, caused by the damaging effect of acid reflux on the laryngeal mucosa 30, however, in these patients, the exposure to acid lays within physiological ranges. We suggest the coexistence with functional dysphonia, an entity caused by an excess of tension in the laryngeal muscles and associated with conditions such as anxiety or depression 31, factors also associated with functional heartburn 21. Among the manometry findings, a greater probability of presenting normal esophageal motility and a type I gastroesophageal junction morphology (overlapping lower esophageal sphincter and crural diaphragm) and a lower probability of presenting type II gastroesophageal junction morphology (lower esophageal sphincter and crural diaphragm axially separated less than 3 cm.) 32. This finding reaffirms the concept that patients with functional heartburn usually present symptoms that are not associated with pathological exposure to acid, therefore they should not present alterations in esophageal motility or the morphology of the gastroesophageal junction. Unlike previous studies, no association with a competent lower esophageal sphincter tonicity was found 33,34. Because the factors associated with this condition are mainly psychological-psychiatric (anxiety, depression, lack of social support), therapy with neuromodulators such as tricyclic antidepressants or selective serotonin receptor inhibitors is reasonable and usually effective. Some studies consider alternative approaches such as acupuncture or hypnosis, however, there is no robust evidence yet 21,35. Since exposure to acid is not the cause of symptoms, surgical management is ineffective in this group of patients 24.
Esophageal hypersensitivity has recently been introduced into practice as a new type of functional disorder 14, and the criteria established in the Lyon and Rome IV consensus were used to establish the diagnosis. This condition, unlike heartburn, is characterized by presenting a positive temporal association between symptoms and episodes of reflux registered through a pH-impedance measurement, which was determined by the symptom index (SI) or the symptom association probability (SAP). The symptom index is the percentage of symptomatic events preceded by reflux episodes and must be greater than 50% to be positive and it is a measure subjected to the association by chance since it does not consider the total number of reflux episodes 27. The symptom association probability uses more complex statistical calculations to express the probability of the association of symptoms and reflux episodes and is considered positive if the p-value is less than 5% 36. Both measures are complementary, SI is a measure of "effect size" and SAP is a measure of probability, therefore they cannot be comparable, and together they represent the best clinical evidence of an association between symptoms and reflux episodes 2. A greater risk of presenting esophageal hypersensitivity was found in patients younger than 43 years, which was the mean age in this group. The mean values of the time of exposure to acid (1.66%) and a total number of reflux episodes (53.29) were higher than in the case of patients with functional heartburn, however, they remain below the ranges considered pathological. As in the functional heartburn group, it was observed that patients suffering from esophageal hypersensitivity usually have a gastroesophageal junction without alterations, however, they may have minor alterations in their esophageal motility or decreased tonicity of the lower esophageal sphincter, as well as a greater probability of presenting supragastric belching, which may be related to the greater number of reflux episodes (40-80) compared to the functional heartburn group (less than 40). For this reason, esophageal hypersensitivity can be initially managed with dual antisecretory therapy -proton pump inhibitors and H2 antagonists 37, however, there is limited evidence regarding the regimen and dose and these patients have usually received this type of therapy months before diagnosis. Management with neuromodulators can be a reasonable pharmacological measure 37, in addition to alternative therapies such as hypnosis or acupuncture 21,35, which can also be part of the management of functional heartburn. In contrast with functional heartburn, the persistence of symptoms is associated with episodes of reflux, but exposure to acid is within physiological ranges. Despite being a functional disorder in which the mechanisms involve greater sensitivity at a peripheral level or an altered perception at a central level 21; It has been observed that this group of patients can benefit from surgical measures, such as Nissen fundoplication 24.
The group of patients diagnosed with true non-erosive reflux disease is exposed to acid in a range considered pathological, without obvious lesions in the esophageal mucosa, and differs with the groups of functional disorders in some aspects (Table 3). Patients older than 50.87 years had a greater susceptibility of suffering from true non-erosive reflux disease and the difference between the mean age of this group with that of functional disorders (esophageal hypersensitivity and functional heartburn) was statistically significant (p <0.03). This finding suggests that structural and motility mechanisms associated with advanced age predispose to pathological exposure to acid, which is reflected in the greater probability for these patients to have ineffective esophageal motility and decreased tone of the lower esophageal sphincter. Although according to the Lyon consensus, these types of alterations in manometry do not determine pathological acid exposure, they are suggestive of it and can serve as clinical predictors to ward off the possibility of a functional disorder 2. Patients with this condition, if antisecretory treatment is unsuccessfully optimized, should benefit from surgical management 38.
Some strengths of the study were the sample size that resulted in the studies high power. In addition, the participating subjects had undergone the diagnostic procedures required in a schematic way to establish the diagnoses. The methods, diagnostic equipment, and the interpretation of the results were standardized in the three private hospitals. However, most of the patients were evaluated by different specialties before undergoing diagnostic procedures. It is possible however, that being a cross-sectional study, an alternative diagnosis that better explained the symptoms was not ruled out 39.
In conclusion, the frequency the frequency of functional heartburn was 46.99%, esophageal hypersensitivity 39.16%, and true non-erosive reflux disease 13.86%. In total, the frequency of functional disorders -86.15%- was higher than that reported in previous studies; probably dietary, cultural, ethnic or lifestyle factors intrinsic to our environment play an important role in these results. From the results of this study, the coexistence of functional heartburn with the diagnosis of functional dysphonia is suggested since both conditions share psychiatric risk factors. Patients older than 50 years were more likely to present true non-erosive reflux disease and had a greater risk of presenting lower esophageal sphincter motility and tone alterations, unlike patients with functional disorders, so it is important to recognize these variables as possible clinical predictors. It is also important to consider the possibility that a patient with refractory reflux symptoms may have a functional disorder, as each diagnosis requires different approaches. It is necessary to carry out more studies to be able to describe frequencies that are generalizable to a national or regional degree and not limited to urban areas. Finally, cohort studies could help determine the efficacy of treatment best suited to the type of disorder presented.