INTRODUCTION
In the differential diagnosis of submucosal lesions of the gastrointestinal tract, the Inflammatory Fibroid Polyps (IFP) or Vanek's tumor are an unusual mesenchymal benign tumor more commonly found in the gastric antrum and small bowel between the 5th and 7th decade of life. The present case is reported due to its unusual clinical presentation as a bleeding submucosal lesion in the cecum in a young patient, and a review of the literature is performed.
CASE REPORT
A 21-year-old man was evaluated in emergency by a lower gastrointestinal bleeding, paleness, and a pre-syncope episode. He has no family history of gastrointestinal malignancies. Vital functions were stable except for tachycardia. Physical examination was unremarkable outside of the paleness and the digital rectal examination which revealed hematochezia.
His hemoglobin was 5.3 g/dL, so he was transfused 3 units of red blood cells. A diagnostic upper endoscopy was performed without remarkable findings. Colonoscopy was performed, showing where the ileocecal valve should be, a rounded submucosal mass of 50 mm protruding into the lumen, with no active bleeding, firm to palpation, biopsies were taken (Figure 1). Also computerized tomography (CT) was performed, evidencing a 4cm cecal mass without extramural extension.
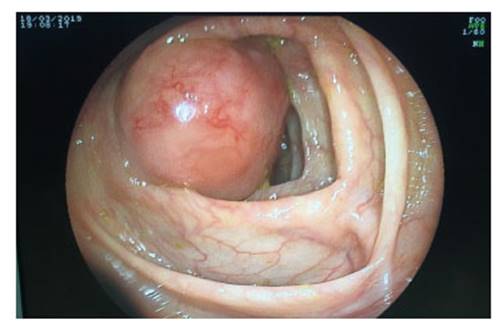
Figure 1 Colonoscopy. A subepithelial lesion is identified at the level of the cecum that does not allow the evaluation of the ileo-cecal valve.
During hospitalization, patient had a new bleeding episode, with persistent hypotension despite fluid therapy and blood transfusion therapy. He was evaluated by a multidisciplinary team and decided an emergency surgery.
During the surgery it was found a cecal tumor of 5x5 cm adjacent to the ileocecal valve and adjacent lymphadenopathies (Figure 2).

Figure 2 Resected surgical specimen. Submucosal lesion without extramural invasion is evident, located at the cecal level and adjacent lymphadenopathy.
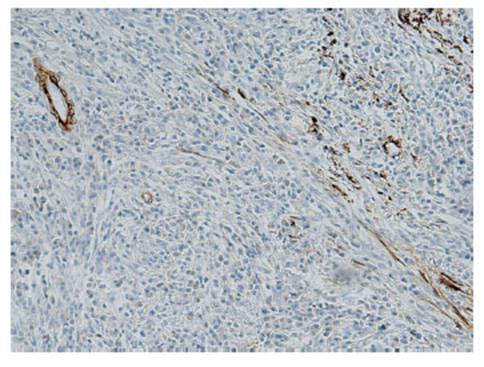
Macroscopic features of the resected specimen showed a polypoid mass of 5x3x3 cm in cecum, which didn’t depend on the mucosa layer (Figure 3) Microscopy showed a submucosal tumor with severe inflammation and absence of malignant cells. Inmunohistochemistry showed CD117( - ) CD34(+), S100(-), Desmin(-), Actin (weakly positive) and Ki67 (˂1%); all this in relation with Vanek's tumor (Figure 4). The patient was discharged 1 week after surgery and had a satisfactory post-operative course.
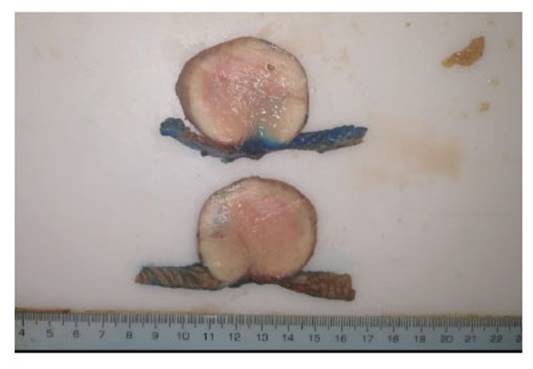
Figure 3 Submucosal lesion of 5 x 5 cm approx, without mucosal involvement, without extramural invasion.
DISCUSION
Inflammatory fibroid polyp (IFP), also called Vanek's tumor or eosinophilic granuloma, is a benign mesenchymal gastrointestinal tumor (1). In 1920, Konjetzny initially reported it as “polypoid fibroma”; later, in 1949, Vanek described a series of cases with 6 patients and named them “gastric submucosal granuloma with eosinophilic infiltration”. In 1953, Helwig and Ranier were the first to coin the term IFP 2).
The etiology of IFP is still unknown. It is believed to be a benign reactive process like the formation of a granuloma in response to an external agent 3). These triggers can be chemical, physical, metabolic, and infectious agents such as parasitic or H. pylori infections 2,4). It is also believed that there may be a genetic role since in some cases it is associated with mutation in the platelet-derived growth factor receptor alpha (PDGFR-a).
This entity is rare, most are incidental findings in endoscopic studies or during surgical interventions 5,6). Although it can affect any age group, the peak incidence occurs between the fifth and seventh decade of life 5). Likewise, it can affect any area of the gastrointestinal tract, being more frequent at the level of the gastric antrum and small intestine. The affection of the colon is very rare, but when occurs the most frequent location is the cecum and the rectum 1,7). The present case shows colonic involvement in a young patient, data that are not very frequent in this type of lesions.
They are usually asymptomatic lesions, but when symptoms occur, they depend on their location and size. The most frequent symptoms when located in the stomach are abdominal pain and gastrointestinal bleeding 1,8). When they are in the colonic region, they can also generate bloody stools, weight loss, diarrhea, and anemia 9), as in the present case that generates significant bleeding with hemodynamic instability. It can also generate complications such as acute abdomen secondary to intussuception or intestinal obstruction (3, 10).
This lesion is endoscopically seen as a pedunculated or sessile polypoid lesion, which may present erosions or superficial ulcerations 3,10). Reports refer that the average size is 2 to 5 cm, however there are reports of cases up to 20 cm 5,6). Echoendoscopy could be useful to better characterize the lesion that is shown as a homogeneous hypoechogenic lesion that originates within the second and third layers of mucosa; In addition, it may have internal echoes corresponding to blood vessels 2). Although it has no specific signs, tomography is the most sensitive imaging method for detecting polyps and their complications 11).
Diagnosis is defined with histopathology and immunohistochemistry. Microscopy shows spindle cells organized in a pattern like onion skin around blood vessels and mucous glands. There may be irregular proliferation of blood vessels with thickness of their walls of different sizes, as well as mixed inflammatory infiltrate with a predominance of eosinophils and lymphocytes 3,11). There are studies that suggest that histological characteristics may vary in relation to the size of the lesion. The first two stages correspond to the nodular and fibrovascular phase characterized by concentric formations of mature and immature fibroblasts and marked inflammatory infiltration. The next two stages, called sclerotic and edematous, characterized by concentric formations by fibroblast-like 5). Some reports mention PDFGR-a mutations can generate a malignant potential, although there is no evidence that this is demonstrated 5,12 since in most reports and case series they do not show recurrence and metastasis 1).
The differential diagnosis is broad, and immunohistochemistry helps us differentiate the lesions. IFPs are characterized by positive CD34 and vimentin, as well as positive for actin, calponin, CD35 and cyclin D1. Differential diagnoses include gastrointestinal stromal tumor (GIST) which is positive for CD 117, also called c-kit; while IFP does not express it; schwannoma is generally positive for S100 protein; and leyomoma expressing desmin, a muscle cell cytoskeleton protein 8,12).
The definitive treatment of this type of tumor is surgical removal. In this case intestinal resection (right hemicolectomy with transverse ileus anastomosis) was the procedure performed as an emergency surgery because of the persistent bleeding. Vanek's tumors are rare lesions, in this case with a very atypical location, mimicking a GIST.
In conclusion, IFP is a rare entity included in the differential diagnosis of submucosal gastrointestinal tumors. The most frequent location is gastric; However, it may be present in other regions of the gastrointestinal tract, such as the colon. Generally asymptomatic but, depending on size and location, can generate symptoms such as pain and bleeding. Immunohistochemistry positive for CD34, vimentin, actin, cyclin D1, CD 35 and calponin; and unlike GIST, they do not express CD117. They are benign lesions that have not demonstrated malignant potential now.