INTRODUCTION
Abdominal pain could be intense in 80% of patients with pancreatic cancer, and it is more difficult to alleviate in cases with unresectable disease 1-3. Patients often require the chronic use of high-dose analgesics and some of them experience serious drug-related side effects that can markedly reduce their quality of life 4. Endoscopic ultrasound-guided celiac plexus neurolysis (EUS CPN) has shown to control cancer-associated pain and it consists of the injection of a neurolytic agent around or within the neural network of the celiac plexus. In a meta-analysis on the use of EUS CPN, the proportion of patients with pancreatic cancer who showed pain relief was 80% 5. Another randomized, controlled, double-blind trial demonstrated that in patients with painful unresectable pancreatic cancer, early EUS CPN reduces pain and the use of morphine 6. We present three different technical approaches for EUS CPN.
CASE REPORT
The procedure was performed with the patient in in the left lateral decubitus position, and sedation was administered by the anesthesiologist. A fine needle aspiration (FNA) Nº 22 gauge was employed for the injection of the neurolytic agent. In cases of bilateral puncture, 10 ml of 0.25% bupivacaine and 10 ml of absolute alcohol (99%) were injected on each side of the celiac trunk. Conversely, in instances of unilateral puncture, the entire dose was injected in the specific area, either into the celiac ganglia or above the outlet of the celiac trunk.
The Visual Analogue Scale was utilized to evaluate the pain intensity reported by the patients both before and after the procedure. This scale consists of a horizontal line measuring 10 cm, where patients marked their current pain level. Pain intensity was scored from 0 to 10, with "0" indicated "no pain" and "10" representing "the worst pain possible" 7.
Case 1
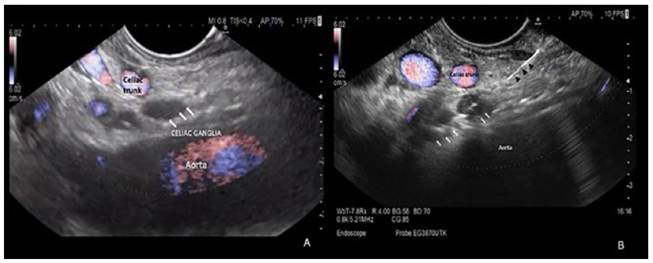
An 89-year-old man with metastatic pancreatic cancer on chronic morphine was referred to our hospital for celiac plexus neurolysis (CPN). Neurolysis of the central celiac plexus was performed by endoscopic ultrasound with ethanol injection just above the root of the celiac trunk (Figure 1A and 1B). There were no adverse events in relation to the procedure.
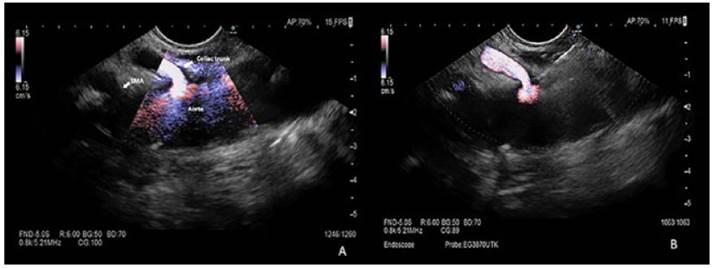
Figure 1 (A) EUS identification of anatomical landmarks for CPN, no celiac ganglia was identified, we performed central CPN. SMA: superior mesenteric artery. (B) Central CPN: injection of ethanol with a 22G Fine Needle Aspiration just above the root of the celiac trunk
In the evaluation of pain, basal score was 8/10 and immediately we obtained a good clinical response (score of 3/10 until 4 weeks). Unfortunately, one month later the patient had more pain (5/10) and had to restart oral morphine.
Case 2
A 72-year-old female patient with pancreatic cancer with liver metastases complained of intractable pain even with the use of oral morphine. She was referred for EUS CPN. She underwent bilateral CPN with ethanol injected on both sides of the celiac trunk (Figure 2 and 3). The patient developed transient hypotension after the procedure, but it was resolved with fluid therapy. A good clinical response was obtained with improvement on pain scale, from basal score of 7/10 to posterior score of 3/10. Patient had not required narcotics until 12 weeks of follow-up and the remaining pain was managed with oral tapentadol.
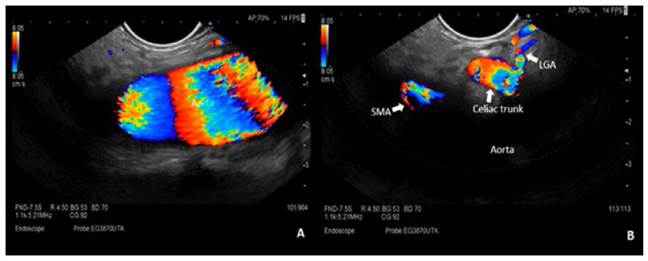
Figure 2 EUS identification of anatomical landmarks for CPN. (A) Celiac trunk and SMA are not located exactly on the central axis of the aorta. (B) With subtle clockwise torque of the endoscope, we were able to visualize the celiac trunk and SMA. SMA: superior mesenteric artery, LGA: left gastric artery.
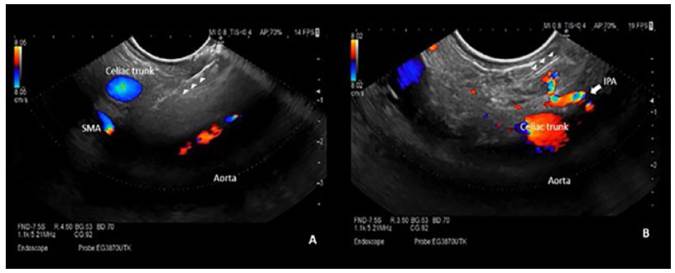
Figure 3 Bilateral CPN: injection of ethanol with a 22G Fine needle aspiration (arrow heads) parallel to the celiac trunk. (A) Injection to the right of the celiac trunk. (B) Injection to the left of the celiac trunk, diffusion of ethanol in the target area. SMA: superior mesenteric artery, IPA: inferior phrenic artery.
Case 3
A 67-year-old female patient with pancreatic carcinoma and refractory cancer-associated pain on intravenous morphine infusion pump (basal score pain of 9/10) was referred for CPN. We identified two celiac neurological nodes with the EUS and performed a neurolysis of the celiac ganglia with direct ethanol injection (Figure 4A and 4B). The patient developed transient hypotension in the immediate post procedure period but was reversed with fluid therapy. The patient persisted with pain during the first weeks after the procedure (score pain of 5/10) and required morphine. From the third week post-neurolysis, she achieved a good clinical response with significant improvement on pain scale (score of 1-2/10). Patient stopped using morphine, requiring only oral tapentadol for complete pain control until 9 weeks of follow-up. .
DISCUSSION
The goal of the CPN is to reduce abdominal pain and the requirement of narcotics to achieve a better quality of life. Endoscopic ultrasonography has shown to be an optimal tool to access the celiac plexus and perform CPN. There are several techniques described for performing CPN via EUS. The first one is celiac ganglia neurolysis (CGN), which consists of the direct injection of ethanol into the celiac ganglia. The first studies about direct neurolysis of the celiac node described detection rates via EUS of at least one node in 81% and 89% of cases, respectively 8,9. In a recent study, it was shown that it is possible to visualize an average of two nodes per patient; 29.9% left the celiac axis, 65.7% central and 4.5% on the right side 10 through EUS. The second technique is neurolysis of the central celiac plexus (central CPN) which consists in a single injection of ethanol immediately above the outlet of the celiac trunk. The last procedure is the neurolysis of the bilateral celiac plexus (bilateral CPN) which consists of injecting ethanol on both sides of the celiac trunk.
The first report on the efficacy and safety of CGN was made by Levy et al. In this series, 16 of 17 pancreatic cancer patients (94%) reported complete or partial pain relief 11. In a randomized clinical trial, it was evidenced that CGN by EUS was significantly superior to central CPN in the relief of pain. Also, the rate of positive response in the CGN group was significantly higher than in the central CPN group (73.5% vs. 45.5%; p=0.026). Meanwhile the complete response rate was also significantly higher in the CGN group compared to the central CPN group (50.0% vs. 18.2%; p=0.010) 12.
Regarding the efficacy of central versus bilateral CPN, in a prospective cohort study, it was found that the bilateral technique achieved significantly more pain relief compared to unilateral CPN (average pain reduction percentage of 70,4% vs. 45.9%; p=0.0016); likewise, the only predictor of pain reduction by> 50% was bilateral injection (OR 3.55) 13. Along the same line, the meta-analysis by Puli et al. found that bilateral CPN achieved a higher proportion of patients with pain relief versus the unilateral technique (84.54% vs. 45.99%) 5.
Although scientific evidence shows that bilateral CPN is more effective than central one, there is no formal study that support one procedure over the other. We suspect that they are comparable techniques because most nodes are lateral to the celiac artery. Therefore, if the celiac nodes are not echoendoscopically visible, bilateral injection seems to be the best option.
Regarding adverse events related to CPN, a recent review found that in 661 cases of EUS CPN, 21% had mild and self-limited adverse events that usually lasted <48 hours and rarely 14 days. The most frequent were diarrhea (7%), transient hypotension (4%) and transient increase in pain (4%). Major complications occurred in 0.2% of the cases 14.
In this short series of cases, we describe that EUS CPN is a safe technique, with mild and self-limited adverse events, as described by the literature. Regarding the efficacy, we had a better and more durable clinical response with bilateral CPN and GCN in comparison to central CPN.