INTRODUCTION
Portal hypertension is associated with the development of varices, which are dilated preexisting or newly formed portosystemic venous channels commonly located in esophageal and gastric regions 1. Acute variceal bleeding is a lifethreatening complication. The risk of bleeding from gastric varices is lower than that from esophageal varices; however, the associated bleeding can be more severe and more difficult to control, with higher mortality 2,3.
Endoscopic cyanoacrylate injection is used in the management of acute gastric variceal bleeding, effectively achieving hemostasis and preventing re-bleeding 1. Cyanoacrylate is a monomer in a liquid form that, in contact with hydroxyl ions in water or blood, undergoes rapid polymerization, acting as a chemical tissue adhesive and leading to hemostasis of the varix. To avoid occlusion of the injection needle and for fluoroscopic monitoring, cyanoacrylate is usually diluted with lipiodol 1,4,5. The mixture results in delayed polymerization, which also increases the risk of distal embolization. Embolism to distal organs is the most severe complication associated with its use. Cyanoacrylate is most commonly used as a 1:1 mixture with lipiodol, injecting 0.5 to 1.0 mL of cyanoacrylate solution into the varix in every injection. The endoscopist usually decides the proper dosage at the time of intervention, considering the dimension of the gastric varices and the initial success in stopping the bleeding. Nevertheless, larger doses could increase the risk of embolism to distal organs 4.
We describe a clinical case report in which multiple emboli occurred after the endoscopic injection of a cyanoacrylate and lipiodol mixture to treat gastric varices.
CLINICAL CASE
A 72-year-old woman was admitted to our hospital for acute digestive tract bleeding with a one-day history of hematemesis and melena. She denied prior gastrointestinal bleeding or the use of ulcerogenic medications. The medical history was compatible with non-stratified alcoholic chronic liver disease. On admission, at the emergency department, she had a pulse of 75 bpm, a blood pressure of 90/66 mmHg, a respiratory rate of 12 breaths/min and pale conjunctiva. Rectal examination demonstrated the presence of melena. Laboratory studies revealed the following: hemoglobin, 3.2 g/dL (reference interval, 12-18 g/dL); hematocrit, 10.8% (37%-49%) platelet count, 181,000/mm3 (135,000450,000/mm3); total bilirubin, 1.0 mg/dL (0.3-1.3 mg/dL); aspartate aminotransferase, 72 U/L (<35 U/L); and alanine aminotransferase, 23 U/L (<33 U/L); creatinine 2.5 mg/dL (0.6-1.1 mg/dL); blood urea nitrogen 80 mg/dL (<50 mg/dL). Her coagulation profiles were prothrombin time 21.6 s (14.5 s), activated partial thromboplastin time 33.3 s (24-35 s) and fibrinogen levels 179.0 mg/dL (200-400 mg/dL). Arterial blood gas analysis revealed serum lactate levels of 4.3 mmol/L. The patient started a blood transfusion with 3 units of erythrocyte concentrate, a proton pump inhibitor (80 mg bolus), and 1 g ceftriaxone. She underwent upper gastrointestinal endoscopy after 30 mg of propofol. Endoscopy showed a conglomeration of gastric varices on the gastric fundus, totaling approximately 40 mm, with an evident red nipple but no active bleeding. Treatment with cyanoacrylate was performed (2 punctures with 1mL each of a lipiodol solution, the second one close to the rupture site) (Figure 1). Following the intervention, the patient became comatose, 7-point in Glasgow Coma Scale, with spontaneous eye opening, absence of verbal response, and decerebrate posture. A cerebral computed tomography was immediately performed, showing multiple cerebral lipiodol emboli (Figure 2A). Due to persistent changes in the consciousness state, the patient was intubated for airway protection and placed on ventilatory support. A thoracic-abdominal-pelvic computerized tomography was also performed, depicting multiple emboli in both lungs, liver, spleen, and left kidney. Additionally, associated with the presence of embolic material, ischemic areas were observed in the spleen and left kidney (Figure 3). Therefore, a patent foramen oval was suspected but not confirmed by a transthoracic echocardiogram with bubble study. The patient repeated a brain computerized tomography scan two days later, showing signs of acute multifocal cerebral ischemia extensively involving the territories of the cortical branches of the middle cerebral arteries and in a moderate territory of the cortical branches of the right anterior cerebral artery (Figure 2B). No neurological improvement was observed during the 5 following days, and after multidisciplinary team discussion, palliative care was provided, and the patient presented a fatal outcome.

Figure 1 Upper digestive endoscopy. (A) Large varix in the gastric fundus. (B) Sclerosis therapy with cyanoacrylate.

(A) Non-contrast cerebral CT scan showing multiple hyperdense foci along the cortical grey matter, cortical grey-white matter junction and deep grey matter, in keeping with cyanoacrylate deposition. (B) CT scan after 2 days depicting signs of acute multifocal cerebral ischemia involving the territories of the middle cerebral arteries and right anterior cerebral artery, with hypoattenuation and loss of grey white matter differentiation.
Figure 2 Non-target cerebral embolism following endoscopic cyanoacrylate injection.
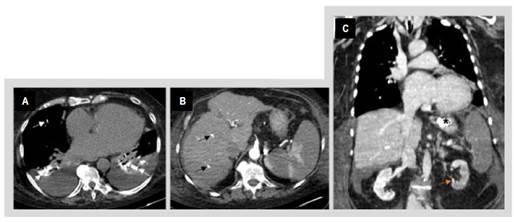
(A) Axial non-contrast chest CT showing bilateral hyperdense foci filling the pulmonary arteries (white arrows). Moderate bilateral pleural effusion is also depicted. (B) Axial abdominal CT after contrast administration depicting multiple splenic infarcts. Hyperdense foci along the liver are also seen (black arrows), in keeping with spillage of the glue. There are also signs of chronic liver disease. (C) Coronal CT after contrast administration showing cyanoacrylate embolization in the inferior pole of the left kidney (orange arrow) with signs of ischemic injury. The treated gastric varices (*), multifocal splenic infarcts, small hyperdense foci in the right lung, and small volume ascites are also evident.
Figure 3 Non-target cyanoacrylate embolism in the lungs, liver, spleen, and left kidney.
DISCUSSION
Gastrointestinal bleeding from gastric varices is a lifethreatening complication of portal hypertension. Endoscopic cyanoacrylate injection is an established and effective form of treatment for acute control of hemorrhage in this situation. Complications from cyanoacrylate treatment are rare; however, embolism to distal organs can occur and is a severe and potentially fatal complication 4-6. Systemic embolization from the portal circulation can occur to any organ, with the lungs the most commonly affected site. However, embolization to other sites has already been described, such as the spleen, portal vein and cerebrum 4,7. The factors that may predict a higher risk of embolization include the large size of gastric varices, the presence and size of collateral vessels, the number of injections per session, excessive dilution of cyanoacrylate with lipiodol, the volume of the injected mixture (>2 mL/ injection) and the speed of the injection 8.
We report here a severe complication after an endoscopic cyanoacrylate injection of a gastric varix in 72-year-old women. This case illustrates the risk of systemic embolization following treatment of large gastric varices with cyanoacrylate and lipiodol. We believe that the size of the varix was a significant risk factor for embolization in this patient. The large size of the gastric varices found in this case report may be associated with the presence of a portosystemic gastrorenal shunt that acts as a shortcut to embolization, therefore allowing for fast blood flow and the consequent systemic migration of the material through these collateral vessels. Additionally, large size gastric varices are associated with the need for repeated injection 8. The embolic material presumably migrated to the lung by passing through a right-to-left intrapulmonary shunt into the systemic circulation, since a foramen oval was ruled out by echocardiography with bubble study. The intrapulmonary arteriovenous shunt could have arisen in the context of hepatopulmonary syndrome, which can be found in about 20% of patients with cirrhosis. This syndrome is characterized by pulmonary microvasculature dilation with right-to-left shunting, therefore allowing for the entry of the cyanoacrylate into the systemic circulation 9.
Endoscopic cyanoacrylate injection is a safe and efficacious procedure for the treatment of gastric variceal bleeding. Systemic embolization, despite its rarity, should be considered among the severe complications, due to its high morbidity and potentially fatal outcome.















