INTRODUCTION
In the middle of May 2022, an out-break of Human Monkeypox (hMPXV) began in the UK with epidemiological features different from those described by Heymann 1 et al. (Central Africa, 19701986). This outbreak of hMPXV outside of Africa, now in 110 countries, is limited to populations of men who interact sexually with men (MSM), emerging a new clinical forms of the disease, depending on the site of primary inoculation, in the oral cavity, the anorectal canal, anus: stomatitis, proctitis, anus proctitis, respectively.
On June 26, 2022, the Ministry of Health of Perú (MINSA) notified the first case of hMPXV in Lima. On July 26, one month later, when there were 978 cases in South America, 224 (23%) were from Perú 2. Of the first 275 hMPXV cases reported as of July 29, 2022, 274 (99.6%) were male, 193 (70.2%) were people living with HIV (PLHIV), 156 (80.8%) of 193 they were PLHIV with HAART, 43 (15.6%) had syphilis, 196 (71.2%) defined themselves as homosexual or bisexual, 23% refrained from answering about their sexual choice 3.
The objective of this publication is to show the histopathological substrate of an atypical and extensive lesion located in the perineum and buttocks, in an HIV-AIDS receptive homosexual patient without HAART with hMPXV treated at a Social Security Hospital ESSALUD in Lima, Perú, the country Latin American with more cases (102) per million inhabitants.
CASE REPORT
The respective informed consent forms were obtained and exposed to the Hospital Ethics Committee. There were no observations. Data and dates that identify the patient are reserved.
A 39-year-old homosexual man was admitted to the Almenara Social Security Hospital in Lima, Peru, with pustular lesions on his body, carrying a PCR Test (+) for Monkeypox and HIV Test (+) diagnosed for the first time. Upon interrogation (second week of October 2022) he stated that his illness began with severe anorectal pain and fecal incontinence, five days after sexual intercourse (receptive) with a foreign citizen, and later the appearance of pustular lesions on his body.
On examination: Glasgow´s scale of 15, pustular lesions with confluent perianal craterlike necrosis of 3.0 cm outside the anal margin, pustular lesions throughout the body (25-30), and signs of oropharyngeal candidiasis. Thoraco-abdomino-pelvic CT scan show pulmonary nodules. Abdomen without alterations. Rectal examination shows severe edema of the anorectal canal. No crepitus in the perianal region or buttocks.
In laboratories results there were 8510 leucocytes, hemoglobin at 13.3 gr%, 4.52 x 105 / mm3 platelets, PCR COVID-19 was negative, CD4: 28 cells/ mm3, HIV viral load at 855 000 copies/ mm3, TORCH: Toxoplasma: Ig G (-) / Ig M (-), Rubella: Ig G (-) / Ig M (-), Cytomegalovirus viral load: 218 502 copies/mm3, HBsAg: negative, HBcAb: indeterminate, HBAnti-IGM: negative, HBsAb: 0.44, HBeAb: negative, HCV: negative, RPR: non-reactive, no BK in gastric juice.
Before the end of the third week of October 2022, a large scabby black lesion was discovered that had spread symmetrically to both buttocks (Figure 1A) and perineum (Figure 1C) within a radius of 15 cm. outside the anus, surrounded by an inflammatory halo. With the presumptive diagnosis of Perianal Fournier Fasciitis (PFS), he is scheduled for debridement and sigmoid colostomy. In the intraoperative examination, it was evidenced that the large black scabby lesion is not compatible with PFS, there is no pus, and no bad odor. Under this crust, the hypodermis is vital. Only loop sigmoid colostomy (due to fecal incontinence) and wide and deep wedge biopsy of the lesion were performed (Figures 1B, 1D).

Figure 1. A. Patient with HIV-AIDS and hMPXV proctitis, complicated by a scabby, black lesion with symmetrical distribution on both buttocks, confused with Fournier fasciitis. It was also accompanied by fecal incontinence. B. Deep wedge biopsy, including scabby and healthy tissue. C. The scabby lesion extended to the perineum. D. Appearance of the obtained biopsy
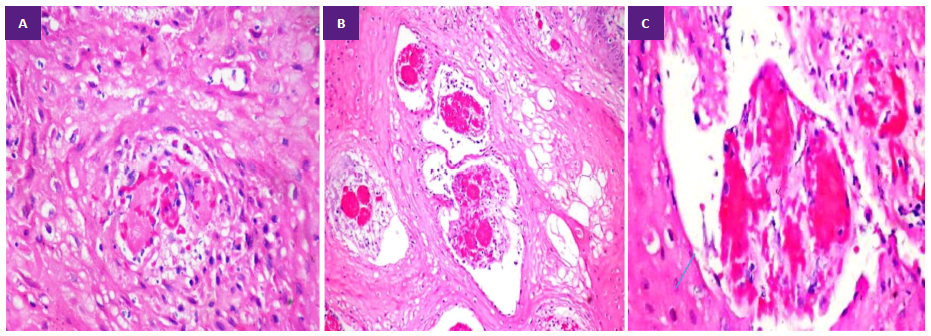
In blood culture (third week of October), Acinetobacter baumannii complex was isolated. The culture of necrotic perineal tissue (deep wedge) was negative. In histopathology, an extensive dermal-epidermal necrosis, congestion, focal hemorrhage (Figure 2A, 2B), and loss of demarcation between epidermis and dermis. In another area of the sample, we observed hyperplastic epidermis and vacuolization of keratinocytes. In the papillary dermis vascular congestion and fibrin micro thrombi (FM) (Figure 3A, 3B, 3C). The patient died the first week of November 2022.
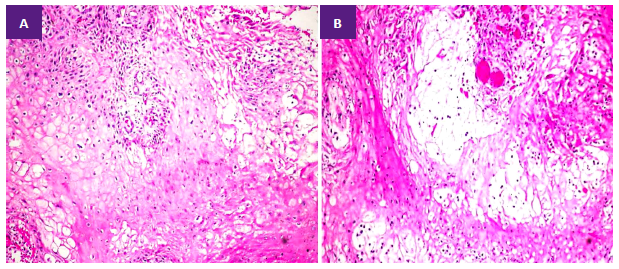
Figure 2. A. Viable skin edge wedge biopsy shows hyperplastic epidermis, keratinocyte vacuolization, vascular congestion in the papillary dermis, and focal necrosis. (H&E 10X). B. Edema and vascular congestion in the papillary dermis (H&E 10X).
DISCUSSION
In Peru, hMPXV emerged as a nationwide epidemic outbreak; 3408 cases were confirmed until the second week of November 2022 in a population of 33, 396,700 inhabitants, implying an incidence of 102 cases per million. Peru was the second nation in South Ame-rica and the seventh in the world with more diagnosed cases 2,3. According to the results of the Virtual Survey for the LGTB Population of Peru 2017 4,5, about of 8,630 adult associates between 18-29 years old, 65.5% reside in Lima, 6% in Arequipa, 5% in Callao, in La Libertad 4%, in Piura 2.2%. The MINSA-Peru reports highlight 3 regions with a high incidence of hMPXV: Lima (2,648 cases), La Libertad (155 cases) and Arequipa (143 cases) 6. This frequency distribution of hMPXV cases coincides with the distribution of the LGTB population in Peru.
Papulopustular lesions of hMPXV in the MSM population begin at the primary inoculation site: mouth, rectum, anus, and perineum. It is necessary to highlight that this rectal and genital involvement is only observed in people whose mucosa has been in close contact with fluids infected with MPXV 7. In the series of 48 cases reported by Orviz 8, 7 of 10 patients who had receptive anal sex suffered perianal lesions compared to 1 of 13 patients who were insertive (p < 0.001); of these 13 insertives, 12 had mainly genital involvement, compared to 1 of the 10 receptives (p < 0.001).
In this outbreak there have been atypical behaviors in the evolution of the disease never described in classic hMPXV from Congo or West Africa. Boesecke 9, has reported the case of a man with hMPXV and a pustule on the nasal apex that in a short time evolved to superficial necrosis of the nasal dorsum and wing in a context of HIV-AIDS that had never been treated. This case is morphologically similar to the case we report.
Patel’s 10) descriptive series refers to “new lesions” other than the classic West African and Congo outbreaks. It is interesting to compare our case and two cases in this series, which in the authors’ opinion, one was secondary to bacterial infection (Staphylococcus aureus and Streptococcus dysgalactiae) and the other was due to coalescence of scabby lesions. In the case that we report, the lesion did not present an exudative or purulent aspect, the culture of the epidermis and deep dermis were negative. Likewise, we do not prove that our patient’s injury is the consequence of confluent lesions; there were no pustular-scabby lesions as a background to the large scabby lesion of the perineum and buttocks, which was seen in the patient in Patel’s series.
The histopathological findings of the crusted and black lesion that we report (indistinction between the epidermis and dermis due to necrosis of the basal layer and necrosis of the overlying epidermis, hyperplastic epidermis underlying healthy skin, vacuolization of keratinocytes, and fibrin micro thrombi in the dermis) were described in part before Stagles 11) (1985) in experimental papular lesions in cynomolgus monkeys, except for fibrin micro thrombi (FM), the latter has never been reported in hMPXV histopathology. The Stagles study, the first described from a human papulonecrotic lesion of 5 days of evolution, did not report FM in the papillary dermis.
There is an evident fact, that the anatomopathological substrate of the symmetric necrosis of the skin of the buttock and perineum free of papulopustules is due to infarction of the dermal-epidermal layer as a consequence of fibrin microthrombosis in the papillary dermis, therefore we postulate that the latter is a novel cytopathogenic effect of MPXV, absent in classical histopathological descriptions.
FM is common in the histopathology of other viruses with dermoepidermal damage: leukocytoclastic FM in measles rash, FM and lymphocytic infiltrate in varicella zoster, FM and endothelial damage in dengue hemorrhagic fever, FM and perivascular infiltrate in zika, acral perniotic lesions due to FM and lesion severe endothelial 12) in severe SARS-Cov-2.
In conclusion, we report a new cytopathogenic effect of MPXV: fibrin micro thrombosis, which plausibly would explain the extensive epidermal-dermal necrosis of the skin of the buttocks and perineum free of papules or pustules, in a severely immunosuppressed patient, never treated with HIV-AIDS, a pathophysiological context that would have increased the aggressiveness of MPXV.