INTRODUCTION
Veterinary practitioners frequently perform surgical procedures in small animal clinic practice. Ovariohysterectomy is the most common surgery (Davidson et al., 2004; Gunay et al., 2011) as birth control as well as a preventive or treatment for diseases related to the reproductive apparatus, such as mammary or uterine tumors, and ovarian cysts, among others (González & Adami, 2022). As in every surgery that needs to get the patient in an anesthetic plane, it not only requires an effective induction but the assurance that the anesthetic protocol effectively provides suitable sedation, hypnosis, and analgesia (Gutiérrez, 2016). Currently, no anesthetic drug provides those effects by itself, making it necessary to take advantage of pharmacological interaction between several drugs to get an adequate surgical plane (Laredo et al., 2014). Nevertheless, anesthesia always carries a risk for the patient due to the hemodynamic alterations related to each drug used. This is the importance of knowing and evaluating the effects of each protocol tobe used to identify which has a lower negative impact (Gutiérrez, 2016).
Every anesthetic procedure has four steps, and it must always begin with the premedication, in which the patient is prepared to go through the subsequent steps (Otero et al., 2016). Then the induction, which requires paying extra attention to respiratory depression generated by some medications. The third is the maintenance, which is the incorporation of central nervous system depressants to guarantee an adequate level of hypnosis, analgesia, and hemodynamic balance and it must extend as long as the surgical procedure (Merigo et al., 2018). Finally, it is the recovery, which requires as well as the steps before, constant monitoring to confirm the patient’s clinical condition, until the complete restoration of typical physiological values (González &Adami, 2022).
Veterinary surgeons commonly perform Total Intravenous Anesthesia (TIVA) in surgical procedures. This is a general anesthesia technique in which administration drugs occur intravenously, widely used to ensure rapid and straightforward anesthetic induction (Raffe, 2020). Ovariohysterectomy (OVH) involves removing the ovaries, uterine horns, and part of the uterus body, which generates a significant amount of damage and, therefore, pain to the dog, pain that could be reflected in the patient’s physiological parameters (Zúñiga, 2012). Those parameters should be continuously monitored before, during, and after the surgery to detect variations indicating inherent risks of anesthesia. For this reason, it is necessary to use equipment for the monitoring the physiological constants and electrical activity of the heart (Robertson, 2019).
To evaluate the heart function is necessary to consider the clinical examination, the determination of cardiac serum enzymes, diagnostic images, and electrocardiography (Teixeira et al., 2018). The intrinsic cardiac conduction system is responsible for promoting the depolarization sequence of myocardial cells and generates the spreading of the electrical impulse (EI) to all myofibrils. Myocardial cells are specialists in generating and conducting EI at variable speeds; any interruption can affect the heart’s functioning and, therefore, the failure of other organs (Basto & Arcila). Previous studies show that anesthetic drugs affect heart function in many ways (Quinn & Kohl, 2021), causing irregular heart rhythms and decreased contraction force. Since every anesthetic medication has a different mechanism of action, and its effects can be exacerbated by the preoperative cardiac function, coexisting diseases, valvular problems, and the increase in blood pressure (Teixeira et al., 2018), the present study aimed to compare the general electrical heart’s activity, blood pressure, and heart rate in three widely used anesthetic protocols for ovariohysterectomy in female dogs.
MATERIALS AND METHODS
This work took place in Bucaramanga, Colombia, in the operating room of the Small Animal Veterinary Clinic of the University of Santander. In total, 33 healthy canines females were selected from shelters, distributed in 3 groups of 11 animals each, aged between 1 and 3 years. These animals weighed 8 to 15 kg, and have good health, normal electrical activity of the heart before the surgery, and classified as ASA I. Dogs with problems at the blood level, tick and flea infestation, positive to hemoparasites in peripheral blood smear and any other heart or health issue identified by semiological examination were discarded.
Three anesthetic protocols were evaluated in a completely randomized experimental design and was taking into account the four steps of anesthesia procedures:
Protocol 1: Ketamine (7 mg/kg) + Pentobarbital sodium (1 mg/kg)
Protocol 2: Ketamine (7 mg/kg) + propofol (3 mg/kg)
Protocol 3: Tiletamine + Zolazepam (7 mg/kg)
Five animals were intervined per day, and every patient got into the surgery with an 8-hour fast. For reducing stress and avoid measurement disturbances, patients rest 20 minutes in a quiet environment as an adaptation period before the procedure. Physiological constants were registered using the Littman cardiology 3M stethoscope, Surgyvet WWV9010 multiparameter equipment, and Welch Allyn blood pressure monitor for cardiovascular activity measures. The surgical team was made up of a surgeon, surgery assistant, anesthesiologist, instrumented, and operating room assistant.
Data was collected from cardiac auscultation, monitored the electrical activity of the heart, and measured blood pressure before, during, and after the surgical intervention. It was administered intravenously (IV) neuroleptanalgesia premedication (acepro-mazine at 0.1 mg/kg, and 3 mg/kg tramadol), and intramuscular (IM) antibiotic therapy (cephalexin 25 mg/kg). The induction and maintenance were administrated IV according to the protocols above. When the anesthetic plane was achieved, physiological constants, electrical heart’s activity, blood pressure, and heart rate were monitored every 5 minutes along with the intervention (20 to 30 minutes). Monitoring continued until the anesthetic effect passed.
It was also administrated a non-steroidal anti-inflammatory drug (Meloxicam 0.1 mg/kg subcutaneously [SC]) as a recovery protocol, and to reduce any postoperative complications. For the statistical analysis, the ANOVA statistical hypothesis and Duncan test were performed to analyse and compare the results.
The present investigation was approved by the Research Committee of the Veterinary Medicine of the University of Santander and consigned in the 074 Act. Dog owners participating in the Project were informed of the research objectives and signed the ‘Informed Consent Form’ before sample collections.
RESULTS
Surgical Phases
Pre-surgical phase. No patients showed any clinical alteration or pathology at the moment of the intervention. Heart rate and blood pressure were between normal values and did not show any significant difference between protocols (Table 1).
Table 1. Comparison of cardiac parameters evaluated according to the protocol and anaesthetic pase
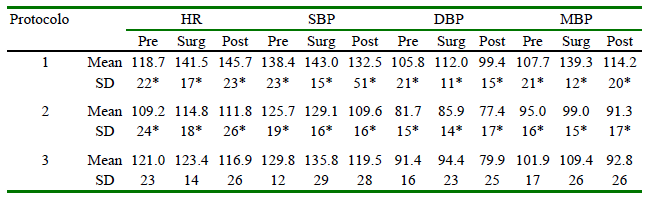
HR: Heart rate; SBP: Systolic blood pressure; DBP: Diastolic blood pressure: MBP: Mean blood pressure Min: Minimum; Max: Maximum; SD: Standard difference
Pre: Pre-surgical phase; Surg: surgical phase, Post: Post-surgical pase
*Differ statistically (p<0.05) from other values in the same column
Surgical phase. There was a considerable increase in heart rate (HF), diastolic blood pressure (DBP), systolic blood pressure (SBP), and mean blood pressure (MBP), in patients with the Protocol 1 as compared with other protocols (p<0.05), as shown in Table 1.
Post-surgical phase. Protocols 2 and 3 had small parameter variations, being Protocol 2 more stable than the other ones. Moreover, Protocol 1 evidenced a significant increase (p<0.05) in all values in this phase compared to reference values for healthy dogs (Table 1).
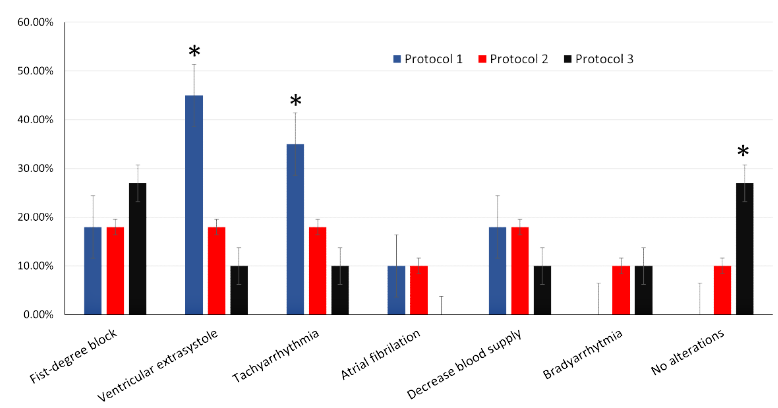
Heart Electrical Conduction
The occurrence of electrical heart alterations was observed in all protocols (Figure 1). Ventricular extrasystole in protocol 1 (46%), protocol 2 (36%), and protocol 3 (9%). The first-degree block was low in protocols 1 and 2 (18%), but relatively high in protocol 3 (27%), tachyarrhythmias were more common in protocol 1 (36%) than in protocol 2 (18%) and 3 (9%), atrial fibrillation was low in protocols 1 and 2, but null in protocol 3. Moreover, protocol 3 presented the highest number of unaltered variables during the surgery (27%).
Recovery Period
The recovery time after surgical procedure was the longest for patients in protocol 1 (1 and 3 hours). On the other hand, although protocol 2 had a short recovery time, muscle tremors were observed. Finally, the fastest anaesthesia recovery, calm and gentle awakening was observed in patients on protocol 3.
DISCUSSION
None of the patients presented alterations on physiological constants in the presurgical phase, probably due to the careful selection of patients. The heart rate alterations observed in the surgical phase on Protocol 1 were probably associated with ketamine dissociative effects between the thalamus, mesocortical system, and reticular bulbar activator, which triggers tachycardia, hypertension, auditory and somatosensory suppression, among other effects (Cruz et al., 2009; López & Sánchez, 2007). Besides, the diastolic blood pressure increase could also be due to the stimulation of sympathetic activity and the inhibition of neuronal catecholamine uptake by ketamine (Callegari et al., 2011).
Sodium pentobarbital is a barbiturate with a depressing effect on the central nervous system by the gamma-aminobutyric acid (GABA) receptor binding, which inhibits neurotransmission, depresses the sensory cortex, decreases motor activity, and disturb cerebellum, causing drowsiness, sedation, and hypnosis (Béjar, 2012). Side effects caused by sodium pentobarbital on the cardiovascular system like myocardial depression, anoxia, hypotension, tachycardia, and arrhythmias, could be associated with the highest heart rates and blood pressures presented in dogs with Protocol 1.
Furthermore, although the barbituric mixtures do not seem to generate side effects on cardiovascular performance, it possibly associates with the non-involvement of peripheral vascular resistance (Padilla & Cardona, 2013). On the other hand, the side effects of ketamine were probably reduced in Protocol 2 by the rapid metabolism of propofol and its synergistic effect with ketamine (Saberfard et al., 2022). Likewise, this mixture not only has been reported reducing those side effects but improving the recovery of patients (Campos, 2014).
Meanwhile, although tiletamine produces a dissociative effect, stimulating the central nervous system, and causing myocardial depression, zolacepam, like other benzodiazepines minimize that cardio-stimulatory response, blocking those side effects of dissociative anesthetics (López & Sánchez, 2007; Kucharski & Kielbowicz, 2021; Saberfard et al., 2022). This mixture provides a muscle relaxation effect, which allows reducing adverse effects on the cardiovascular system (Cruz, 2005; Kucharski & Kielbowicz, 2021). Therefore, it acts as a secure protocol that provides stability during anaesthesia in surgical procedures (Svorc et al., 2015; Kucharski & Kielbowicz, 2021).
The post-surgical phase showed a temporary elevation of HR in Protocol 1, probably due to the inhibition of sympathetic neuronal uptake of norepinephrine (Callegari et al., 2011). Protocols 2 and 3 provided stability in this parameter because of the rapid metabolism of the drugs used. On the other hand, blood pressure parameters (PAS, PAD, PAM) did not show alterations, which is associated with the decreased availability of the drug in blood circulation and its adverse effects (Kucharski & Kielbowicz, 2021; Saberfard et al., 2022).
The high ventricular extrasystole and tachyarrhythmias present in Protocol 1 was probably associated with ketamine action. Compared to sodium pentobarbital, this one is less potent, prolonging atrioventricular conduction time and the intrinsic frequency of sinus node (Béjar, 2012; Saberfard et al., 2022). However, due to its sympathetic action and the increase in circulating catecholamine after its administration may affect cardiac arrhythmogenesis. (Zaballos et al., 2005).
High ventricular extrasystoles was also observed in Protocol 2. Although propofol is supposed to counteract tachycardia by conferring adequate hemodynamic stability and producing a decrease in systemic vascular resistance, given its chroneuotropic negative effect (Torres et al., 2001), it did not show a significant difference compared to Protocol 1. In contrast, Protocol 3 showed a lower percentage of electrical conduction disturbances associated with a decrease in hemodynamic consequences (Svorc et al., 2015; Kucharski & Kielbowicz, 2021).
CONCLUSIONS
A very positive cardioprotective effect with less variation in heart rate, diastolic, systolic and mean arterial pressure were observedinprotocols2(Ketamine[7mg/kg] + propofol [3 mg/kg[) and 3 (Tiletamine + zolazepam [7 mg/kg]).
Protocol 3 presented fewer alterations in the electrical conduction of cardiac activity than the other protocols. In addition, it showed a better awakening at a dose of 7 mg/kg IV.












 uBio
uBio