Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Medicina Experimental y Salud Publica
versión impresa ISSN 1726-4634
Rev. perú. med. exp. salud publica vol.37 no.2 Lima abr./jun 2020
http://dx.doi.org/10.17843/rpmesp.2020.372.4779
Original article
Risk of brain damage in premature infants under 34 weeks of gestational age exposed to histological chorioamnionitis Lima, Peru
INTRODUCTION
Five decades ago, Eastman and DeLeon 1 linked maternal fever to cerebral palsy (CP) in full-term infants. Since then, it has been known that chorioamnionitis (CA) can induce preterm birth and potentially cause brain damage in the infant 2.
CA is produced by bacterial invasion of the placenta with subsequent infiltration of polymorphonuclears (PMN) 3, and is considered one of the main causes of obstetric morbidity in Lima 4. Clinical CA (CCA) affects 0.5% to 10% of all pregnancies, and increases the risk of premature birth by three times 5. Meanwhile, histological CA (HCA) is present in 25-40% of all preterm births and up to 80% in preterm births under 30 weeks 6. In this regard, several studies have demonstrated the poor correlation between clinical and histological diagnosis 2 , 5 , 7.
In Peru, brain lesions prevalent in premature infants under 34 weeks have been reported. The diagnosis was made using clinical and serial ultrasound examinations; lesions found were more severe as the gestational age decreased 8. Likewise, experimental studies and clinical observations have shown that CA can produce brain damage by direct invasion of pathogenic bacteria (sepsis/meningitis) 9 - 11 or by the effect of inflammatory products (cytokines) generated during placental infection 6 , 12. In this process, cytokines could pass the blood-brain barrier (BBB), injure the cerebral white matter 6 , 11 and sometimes generate intraventricular hemorrhage 2.
In the long term, it has been observed that infants exposed to HCA are at increased risk of developing CP and other neurodevelopmental disorders 6 , 13. However, recent studies have questioned these findings and propose the development of new research methodologies to resolve the possible underlying mechanism 14 , 15.
The histopathological study of the placenta and the clinical follow-up offer more evidence to characterize the possible association between HCA and brain damage in the preterm infant. Therefore, the objective of this study was to explore the risk of brain damage in preterm infants under 34 weeks of age exposed to HCA, identified sequentially by age, up to 40 weeks of corrected gestational age. As a secondary objective, due to their relevance in intensive care, maternal and neonatal characteristics were analyzed according to the condition of HCA.
KEY MESSAGES
Motivation for the study: Chorioamnionitis is frequent and very risky in pregnant women. The potential harmful role of histological chorioamnionitis subtypes on the immature brain of the premature infant has not been determined.
Main findings: Concurrent infection of chorion and amnion doubles the risk of intraventricular hemorrhage during the first week of life and triples the risk of white matter lesions between 7 and 30 days of age in premature infants under 34 weeks.
Implications: To encourage obstetric surveillance and include histological examination of the placenta in all preterm deliveries. Recommend periodic neonatal neurological evaluation.
MATERIALS AND METHODS
Design and population
A prospective cohort study of preterm infants under 34 weeks conducted at the Cayetano Heredia Hospital (Lima, Peru). Subtypes of HCA were related to types of brain damage by age, up to 40 weeks of corrected gestational age. The sample size was estimated at 36 preterm infants without a history of HCA and 36 preterm infants with past history of HCA. For the calculation, a 95% confidence level, power of 80% and precision of 0.133 was assumed, which is the difference in the anticipated probabilities of neurological disease between exposed (0.583) and unexposed (0.450) preterm infants, based on an exploratory pilot in the same setting and under the same conditions.
Premature infants under 34 weeks of age born during the year 2015 with histological examination of the placenta were included. Gestational age was recorded in the following certainty order, by date of last menstruation, first trimester ultrasound or Ballard’s scale. Newborns with severe malformations and those whose mothers had uncontrolled neuropsychiatric pathologies were excluded.
Variables
Maternal, neonatal, anthropometric data, clinical evolution, ultrasounds and histopathological examination of the placenta were recorded in a clinical file. All placentas had macroscopic and microscopic examination performed. HCA was defined as the presence of diffuse or parceled PMN infiltrate in the placenta (≥10 PMN/field). Pathological findings were classified according to the inflammation progression, and the following types were defined: sub-chorionitis, chorionitis and chorioamnionitis. Funisitis was also studied, and it was defined as the presence of PMN infiltration in the umbilical cord.
According to the highest probability of brain injury by age of the premature infant, brain damage 7 was defined as any type of identifiable brain injury during the first week (0 to 7 days), between the first and fourth week (7 to 30 days), and at 40 weeks of corrected age. The types of damage were classified as intraventricular hemorrhage (IVH), periventricular leukomalacia (PVL), neonatal encephalopathy (NE), meningitis (MEC), striated lenticule vasculopathy (SLV), parenchymal hemorrhage (PH), cerebral infarction (CI) and cerebral hypoplasia (CH). Hemorrhagic and ischemic lesions tend to be much more frequent in the first week; white substance lesions, between the third and fourth week; and brain trophic effects, at 40 gestational weeks of corrected age 8 , 16.
Probable sepsis was considered in those cases with clinical signs and evidence of leukocytosis, C-reactive protein or procalcitonin positive. Confirmed sepsis was considered in cases with positive clinical signs and blood cultures 17.
Cases of meningitis required demonstration of pleocytosis (≥30 leukocytes per milliliter in CSF), cases of encephalopathy were defined as the presence of clinical manifestations (hypoactivity, hypotonia, epileptic seizures) and metabolic acidosis.
All patients underwent neurological examination, head circumference measurement and brain ultrasound, during the first three days, then weekly for three weeks, and then every four weeks until 40 weeks of corrected age. Tests were performed by a neuropediatrics specialist. All ultrasounds were reviewed a second time by a neonatal brain ultrasound specialist.
Ethical considerations
All infants received neonatal care in intensive care units in accordance to both, the hospital protocol and the Peruvian Ministry of Health protocol 18. In all cases, informed consent was requested; in addition, when the mother was under 18 years old, the assent and consent of an adult family member was requested. The study was approved by the Ethics Committees of Universidad Peruana Cayetano Heredia and the Cayetano Heredia Hospital.
Statistical analysis
The information collected was stored in a protected database and analyzed with STATA 13. Numerical variables with normal distribution were analyzed with the Student’s T-test, and numerical variables without normal distribution, with the Mann-Whitney U test.
For the bivariate analysis of neonatal characteristics, the Fisher’s exact and Chi-square tests were used, depending on the expected frequencies. For multivariate analysis, variables were analyzed by preterm age groups, 0-7 days, 7-30 days, and 40 weeks corrected age, according to the probability of highest risk. The relative risk of developing brain damage in infants exposed to HCA was determined with a generalized linear model, of the Poisson family for dichotomous variables, used by the form of variable distribution response (brain damage), with robust error variance. For this analysis, confounding variables that were associated with brain damage were included in the bivariate analysis.
RESULTS
Patient enrollment
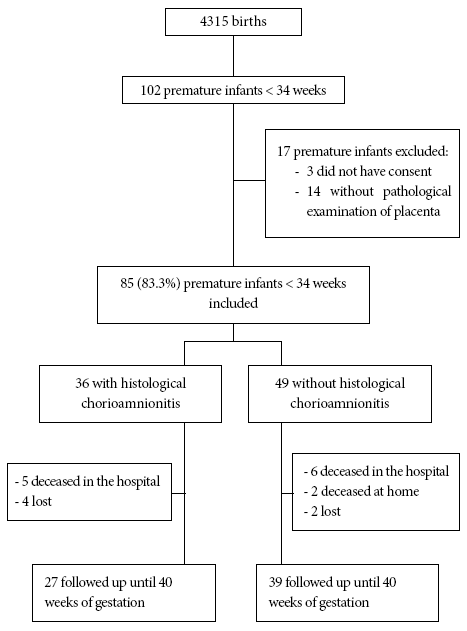
In 2015, 102 premature infants under 34 weeks of age were born. For this study 85 patients were included, 66 of them concluded the follow-up up to 40 weeks of corrected age, 6 abandoned the follow-up (7.1%) and 13 died (15.3%). The study was concluded in March, 2016 at the completion of the last preterm patient follow-up (Figure 1).
General characteristics of the study population
From the total of preterm infants, 42.4% (36/85) was born exposed to HCA (Figure 1). The average maternal age was 27.6 years (SD: 7); and 45.9% (39/85) had adequate prenatal controls. Urinary tract infection and premature rupture of membranes (PROM) were found in 28.2% and 25.9% of the mothers, respectively; and were also the most common maternal antecedents. Gestational age average was 30.9 weeks (SD: 2.6) and average weight was 1,670 g (SD: 526.1). Most infants had low weight for their gestational age and the average length at birth was 41.3 cm (SD: 4.5) (Table 1).
Table 1 Frequency of maternal and neonatal characteristics.
| Maternal | n (%) | Neonatal | n (%) |
|---|---|---|---|
| Age, mean (SD) | 29 (4.6) | Gender | |
| Educational level | Female | 40 (47.1) | |
| Primary | 4 (4.7) | Male | 45 (52.9) |
| Secondary | 58 (68.2) | Gestational age (weeks) | |
| College | 23 (27.1) | 24 to 29 | 26 (30.6) |
| Marital status | 30 to 31 | 27 (31.8) | |
| Single | 20 (23.5) | 32 to 33 | 32 (37.6) |
| Live-in partner | 52 (61.2) | Weight, mean (SD) | 1670.5 (526) |
| Married | 13 (15.3) | Length, mean (SD) | 41.3 (4.5) |
| Adequate prenatal controls | 39 (45.9) | Cranial circumference at birth, mean (SD) | 28.7 (2.8) |
| Clinical chorioamnionitis | 6 (7.1) | Cranial circumference percentile, mean (SD) | 55.2 (28.5) |
| Multiple gestation | 18 (21.2) | Weight / Gestational Age Adequacy | |
| Vaginosis | 13 (15.3) | Adequate | 2 (2.4) |
| Urinary tract infection | 24 (28.2) | Low birth weight | 56 (65.9) |
| Gestational hypertension | 6 (7.1) | Very low birth weight | 16 (18.8) |
| Preeclampsia / eclampsia | 15 (17.6) | Extremely low birth weight | 11 (12.9) |
| Third trimester hemorrhage | 12 (14.1) | Deceased | 13 (15.3) |
| Intrauterine growth restriction | 6 (7.1) | Sepsis | |
| Gestational diabetes | 6 (7.1) | No | 32 (37.6) |
| Peripartum fever | 15 (17.6) | Possible | 4 (4.7) |
| Premature rupture of membranes pre-term | 22 (25.9) | Probable | 28 (32.9) |
| Premature rupture of membranes > 18 hours | 13 (15.3) | Confirmed | 21 (24.7) |
| Abnormal obstetric ultrasound | 10 (11.8) | Acute renal failure | 12 (14.1) |
| Prenatal steroid use | 27 (31.8) | Hyaline membrane disease | 45 (52.9) |
| Birth | Hypoglycemia | 21 (24.7) | |
| Vaginal | 19 (22.4) | Pneumonia | 14 (16.5) |
| Cesarean section with labor | 23 (27.1) | Anemia | 29 (34.1) |
| Cesarean section without labor | 43 (50.6) | Prematurity Apnea | 24 (28.2) |
| Reanimation | Necrotizing Enterocolitis | 6 (7.1) | |
| No | 25 (29.4) | Jaundice | 49 (57.6) |
| Oxygen | 7 (8.2) | Neonatal Encephalopathy | 9 (10.6) |
| Neopuff | 39 (45.9) | Bilirubin Encephalopathy | 1 (1.2) |
| T tube | 8 (9.4) | Persistence of ductus arteriosus | 22 (25.9) |
| Massage | 6 (7.1) | Pneumothorax | 5 (5.9) |
| Amniotic fluid | |||
| Clear | 74 (87.1) | ||
| Meconial fluid | 8 (9.4) | ||
| Meconial thick fluid | 3 (3.5) | ||
Characteristics associated with histological chorioamnionitis
HCA was distributed as follows: subchorionitis 38.9% (14/36), chorionitis 38.9% (14/36), and chorioamnionitis 22.2% (8/36). All the cases of funisitis 44.4% (16/36) were combined with some type of affectation in the placental layers.
Maternal education was a factor negatively associated with HCA (p = 0.042). PROM and rupture of membranes for over 18 hours were more frequent in preterm infants exposed to HCA (p = 0.004 and p = 0.033, respectively). Prenatal steroid use was less frequent in the HCA group (p = 0.002). Vaginal delivery was more frequent in the HCA-exposed group (p = 0.044), while caesarean section without labor was more frequent in the non-exposed group (p = 0.044). Other characteristics of the mother, according to the status of the HCA, are detailed in Table 2.
Table 2 Maternal characteristics according to the histological chorioamnionitis status.
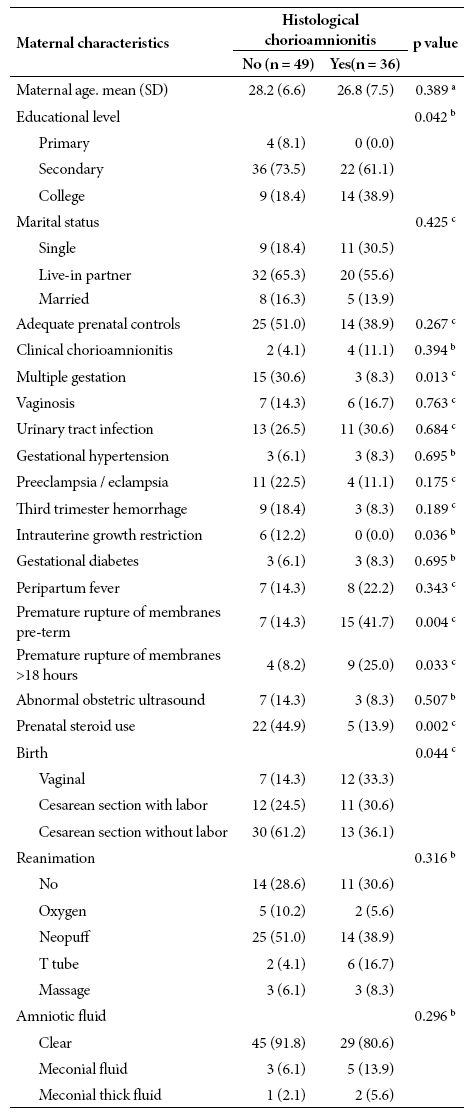
a Student’s T-test, b Fisher’ s exact test, c Chi-square test
The average head circumference percentile for the group with HCA was 47.6 (standard deviation: 28.3), lower (p = 0.035) than the group without HCA (60.7, standard deviation: 27.6). Of the total of patients, 57.6% (49/85) had probable or confirmed sepsis, which was more frequent in preterm infants exposed to HCA (p = 0.013). Other characteristics of the newborn, according to the status of the HCA, are described in Table 3.
Table 3 Neonatal characteristics of preterm infants according to the histological chorioamnionitis status.
| Neonatal Characteristics | Histologic chorioamnionitis | p value | |
|---|---|---|---|
| No (n = 49) | Yes (n = 36) | ||
| Gender | 0.679 a | ||
| Female | 24 (49.0) | 16 (44.4) | |
| Male | 25 (51.0) | 20 (55.6) | |
| Gestational age | 0.097a | ||
| 24 to 29 | 14 (28.6) | 12 (33.3) | |
| 30 to 31 | 20 (40.8) | 7 (19.4) | |
| 32 to 33 | 15 (30.6) | 17 (47.2) | |
| Weight | 1,688.7 (500) | 1,645.6 (567) | 0.711 b |
| Length, median (IQR) | 41.6 (4.6) | 40.8 (4.3) | 0.215 c |
| Cranial circumference at birth, mean (SD) | 29.1 (2.3) | 28.2 (3.3) | 0.179 b |
| Cranial circumference percentile, mean (SD) | 60.7 (27.7) | 47.6 (28.3) | 0.035 b |
| Weight/Gestational Age Adequacy | 0.818 d | ||
| Adequate | 1 (2.0) | 1 (2.8) | |
| Low birth weight | 34 (69.4) | 22 (61.1) | |
| Very low birth weight | 9 (18.4) | 7 (19.4) | |
| Extremely low birth weight | 5 (10.2) | 6 (16.7) | |
| Deceased | 8 (16.3) | 5 (13.9) | 0.758 a |
| Sepsis | 0.013 d | ||
| No | 25 (51.1) | 7 (19.4) | |
| Possible | 1 (2.0) | 3 (8.3) | |
| Probable | 12 (24.5) | 16 (44.4) | |
| Confirmed | 11 (22.4) | 10 (27.8) | |
| Acute renal failure | 6 (12.2) | 6 (16.7) | 0.563 a |
| Hyaline membrane disease | 29 (59.2) | 16 (44.4) | 0.179 a |
| Hypoglycemia | 15 (30.6) | 6 (16.7) | 0.141 a |
| Pneumonia | 8 (16.3) | 6 (16.7) | 0.967 a |
| Anemia | 16 (32.7) | 13 (36.1) | 0.740 a |
| Prematurity apnea | 12 (24.5) | 12 (33.3) | 0.371 a |
| Necrotizing Enterocolitis | 4 (8.2) | 2 (5.6) | 1.000 d |
| Jaundice | 26 (53.1) | 23 (63.9) | 0.318 a |
| Neonatal Encephalopathy | 5 (10.2) | 4 (11.1) | 1.000 d |
| Bilirubin Encephalopathy | 0 (0.0) | 1 (2.8) | 0.424 d |
| Ductus arteriosus persistence | 12 (2.5) | 10 (27.8) | 0.732 a |
| Pneumothorax | 2 (4.1) | 3 (8.3) | 0.646 d |
SD: standard deviation, IQC: interquartile range
a Chi-square test, b Student’s T-test, c Mann-Whitney U-test, d Fisher’s exact test
Neonatal characteristics associated with neurological damage
A high frequency 52.9% (45/85) of neurological pathologies was found. It was higher in the group with HCA (63.9%) compared to the group without HCA (44.9%) (p = 0.083). SLV was notable with 33.3% of cases in the group with HCA compared to 20.4% in the group without HCA (p = 0.179). IVH was also notable with 25% in the group with HCA compared to 20.4% in the group without HCA (p = 0.616). Frequencies of PVL, MEC and NE were very small and similar in both groups.
Sepsis had the greatest impact on neurological damage during the first week of life (p = 0.015) and between 7 and 30 days of life (p = 0.008). Renal failure, hyaline membrane disease, necrotizing enterocolitis and persistent ductus arteriosus were found to be associated with neurological damage between 7 and 30 days of life (p < 0.050). Pneumonia only had impact during the first 7 days (p = 0.017), and necrotizing enterocolitis was the only one associated with alterations found at 40 weeks of corrected age (p = 0.029). The association between other pathologies and neurological damage are presented in Table 4.
Table 4 Neurological damage according to neonatal clinical characteristics by age group in premature infants under 34 weeks.
| Characteristics | 0 to 7 day from birth (IVH, SLV, MEC, NE) | 7 to 30 days from birth (PVL, SLV) | At 40 corrected weeks (SLV o hypoplasia) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| No (62) | Yes (23) | p value | No (55) | Yes (30) | p value | No (45) | Yes (21) | p value | |
| Respiratory depression at birth | 2 (3.2) | 2 (8.7) | 0.295 a | 1 (1.8) | 3 (10.0) | 0.124 a | 2 (4.4) | 1 (4.8) | 1.000 a |
| Age gestational (weeks) | 0.027 b | 0.001 b | 0.222 b | ||||||
| 24 to 29 | 14 (22.6) | 12 (52.2) | 10 (18.2) | 16 (53.3) | 8 (17.8) | 7 (33.3) | |||
| 30 to 31 | 21 (33.9) | 6 (26.1) | 18 (32.7) | 9 (300) | 15 (33.3) | 8 (38.1) | |||
| 32 to 33 | 27 (43.6) | 5 (21.7) | 27 (49.1) | 5 (17.7) | 22 (48.9) | 6 (28.6) | |||
| Sepsis | 0.015 a | 0.008 a | 0.710 a | ||||||
| No | 28 (45.2) | 4(17.4) | 27 (49.1) | 5 (16.7) | 21 (46.7) | 7 (33.3) | |||
| Possible | 3 (4.8) | 1 (4.4) | 3 (5.4) | 1 (3.3) | 2 (4.4) | 2 (9.5) | |||
| Probable | 21 (33.9) | 7 (30.4) | 16 (29.1) | 12 (40.0) | 14 (31.1) | 8 (38.1) | |||
| Confirmed | 10 (16.1) | 11 (47.8) | 9 (16.4) | 12 (40.0) | 8 (17.8) | 4 (19.1) | |||
| Acute renal failure | 2 (3.2) | 10 (43.5) | 0.000 a | 4 (7.3) | 8 (26.7) | 0.022 a | 2 (4.4) | 2 (9.5) | 0.587 a |
| Hyaline membrane disease | 28 (45.2) | 17 (73.9) | 0.018 b | 22 (40.0) | 23 (76.7) | 0.001 b | 18 (40.0) | 12 (57.1) | 0.289 b |
| Hypoglycemia | 14 (22.6) | 7 (30.4) | 0.456 b | 13 (23.6) | 8 (26.7) | 0.757 b | 9 (20.0) | 7 (33.3) | 0.239 b |
| Pneumonia | 6 (9.7) | 8 (34.8) | 0.017 a | 7 (12.7) | 7 (23.3) | 0.232 a | 3 (6.7) | 5 (23.8) | 0.098 a |
| Anemia | 18 (29.0) | 11 (47.8) | 0.104 b | 16 (29.1) | 13 (43.3) | 0.186 b | 11 (24.4) | 5 (23.8) | 0.955 b |
| Prematurity apnea | 19 (30.7) | 5 (21.7) | 0.418 b | 18 (32.7) | 6 (20.0) | 0.213 b | 13 (28.9) | 5 (23.8) | 0.666 b |
| Necrotizing Enterocolitis | 2 (3.2) | 4 (17.4) | 0.043 a | 0 (0.0) | 6 (20.0) | 0.001 b | 0 (0.0) | 3 (14.3) | 0.029 a |
| Jaundice | 36 (58.1) | 13 (56.5) | 0.898 b | 30 (54.5) | 19 (63.3) | 0.433 b | 24 (53.3) | 15 (71.4) | 0.164 b |
| Neonatal Encephalopathy | 5 (8.1) | 4 (17.4) | 0.245 a | 6 (10.9) | 3 (10.0) | 1.000 a | 6 (13.3) | 1 (4.8) | 0.416 a |
| Bilirubin Encephalopathy | 1 (1.6) | 0 (0.0) | 1.000 a | 0 (0.0) | 1 (3.3) | 0.353 a | 0 (0.0) | 1 (4.8) | 0.318 a |
| Ductus arteriosus persistence | 11 (17.7) | 11 (47.8) | 0.005 b | 7 (12.7) | 15 (50.0) | 0.000 b | 7 (15.6) | 7 (33.3) | 0.117 a |
| Pneumothorax | 3 (4.8) | 2 (8.7) | 0.609 a | 3 (5.4) | 2 (6.7) | 1.000 b | 2 (4.4) | 1 (4.8) | 1.000 a |
IVH: intraventricular hemorrhage, SLV: striated lenticulum vasculopathy, MEC: meningitis, NE: neonatal encephalopathy, PVL: periventricular leukomalacia, CH: cerebral hypoplasia
a Fisher’s exact test, b Chi-square test
From the total of patients, 13 premature infants died with an average gestational age of 27.8 (SD: 3.5) weeks, 61.5% (8/13) were male, and five showed clinical chorioamnionitis. In the group without HCA, 8 children died, 5 of which presented neurological damage 5/8 (62.5%). In the group with HCA, 5 children died, all with neurological damage 5/5 (100%) (Figure 1).
Risk of brain damage based on history of histological chorioamnionitis
Table 5 shows the multivariate analysis of relative risk (RR), where the effect of the variables like, sepsis, use of steroids, acute renal failure, pneumonia, necrotizing enterocolitis and persistence of the ductus arteriosus was controlled. Likewise, the effects of IVH, MEC and NE between birth and the first four weeks of age were filtered for their potential deleterious effect up to 40 weeks of gestational age.
Table 5 Risk of brain damage in premature infants under 34 weeks of age exposed to histological chorioamnionitis.
| Pathological findings | 0 to 7 days from birth (IVH, SLV, MEC, NE), n = 85 | 7 to 30 days from birth (PVL, SLV), n = 85 | At 40 corrected weeks (SLV, CH), n = 66 a | ||||||
|---|---|---|---|---|---|---|---|---|---|
| RR | p value | 95%CI | RR | p value | 95% CI | RR | p value | 95% CI | |
| Histological chorioamnionitis | 1.13 | 0.717 | 0.58-2.19 | 1.43 | 0.366 | 0.66-3.10 | 0.91 | 0.796 | 0.44-1.89 |
| Sub-chorionitis | 0.60 | 0.389 | 0.19-1.92 | 1.69 | 0.189 | 0.77-3.72 | 0.93 | 0.868 | 0.39-2.23 |
| Chorionitis | 0.92 | 0.846 | 0.41-2.09 | 0.33 | 0.123 | 0.08-1.35 | 1.04 | 0.939 | 0.40-2.69 |
| Chorioamnionitis | 2.11 | 0.027 | 1.09-4.11 | 2.72 | 0.035 | 1.07-6.88 | 0.83 | 0.781 | 0.22-3.08 |
| Funisitis | 1.17 | 0.616 | 0.63-2.18 | 0.91 | 0.845 | 0.37-2.25 | 0.80 | 0.660 | 0.30-2.16 |
| Chorioamnionitis and funisitis | 2.33 | 0.042 | 1.03-5.27 | 3.23 | 0.000 | 1.84-5.66 | 2.66 | 0.012 | 1.24-5.71 |
This table presents the regression analysis of each of the 6 variables independently, each row is an adjusted regression analysis (Histological Chorioamnionitis, Subchorionitis, Chorionitis, Chorioamnionitis, Funisitis, Chorioamnionitis and Funisitis)
IVH: intraventricular hemorrhage, SLV: striated lenticulum vasculopathy, MEC: meningitis, NE: neonatal encephalopathy, PVL: periventricular leukomalacia CH: cerebral hypoplasia, RR: relative risk, 95% CI: 95% confidence interval
a At 40 weeks corrected, the effect of IVH, MEC, PVL and NE was filtered out.
Chorioamnionitis (histological involvement of chorion and amnion) was the only type of HCA associated with neurological damage (p = 0.006). This subtype of HCA, doubled the risk of brain damage in the first week of life (RR = 2.11, 95% CI 1.09-4.11), which included IVH, EN, MEC and SLV. Individualized analysis for IVH alone in the same period increased the risk of damage (p = 0.007) (RR = 2.46; 95% CI: 1.28-4.72). With the same factor, the damage risk almost tripled between 7 and 30 days of age, a period in which the types of white matter, SLV and PVL were predominant (RR = 2.72; 95% CI: 1.07-6.88).
Funisitis as a single factor was not associated with neurological damage; however, a potentiating effect is observed when associated with chorioamnionitis, as the relative risk increases from 2.11 to 2.33 at 0-7 days of age and from 2.72 to 3.23 at 7-30 days of age.
Other relevant findings
Brain damage between 7 and 30 days of age was associated with the lowest gestational age and lowest head circumference at birth (p = 0.000). Also, extreme preterm infants with HCA had more extensive brain damage at 40 weeks of corrected age (p = 0.027).
Among non-placental factors, pneumonia was found to be a risk factor for neurological damage at any time (P < 0.001) (RR = 1.89, 95% CI 1.34-2.69), similar to chorioamnionitis. Among other effects, chorioamnionitis was found to be a risk factor for ductus arteriosus persistence (P=0.013) (RR = 2.8, 95% CI 1.4- 5.6).
DISCUSSION
Histological chorioamnionitis has a deleterious effect at different ages of the premature infant under 34 weeks, with a risk of producing or contributing to some early and late brain injuries. These effects are known as “distantly injurious” because they emphasize cytokine mediated mechanisms 12.
The research model we present is innovative, because it allows us to establish the effect of HCA on brain tissue as seen by preterm age. The design, underutilized in the literature, highlights the importance of histological examination of the placenta and its relationship with neurological and ultrasound monitoring of the patient 16.
The neurological damage related to histological chorioamnionitis in premature infants is a controversial issue that has been analyzed in experimental animal studies. Although the susceptibility of brain tissue has been demonstrated 19, the results of clinical studies have not been able to conclusively clarify this association 15 , 20 , 21.
CA is an intense inflammatory process, whose main mechanism begins with the premature rupture of the amniotic membranes, which facilitates the entry of microorganisms from the vaginal flora into the intrauterine space 3. Thus, PROM and prolonged rupture of membranes are frequently associated 22. Although the most common germs are from the vaginal flora 12 , 20, resulting in as many as 71.1% positive cultures 20, there is often sterile chorioamnionitis, induced in conditions of stress, damage or cell death, such as placental detachment or additional infections 3 , 20 , 23.
Regardless of the bacteriological risk, a powerful immune response is triggered in both, mother and fetus. In the mother, the production of prostaglandins and cytokines (IL-1β, IL-6, IL-8, TNF-α) that induce premature labor are activated 6 , 13, and in the fetus, systemic inflammatory response syndrome is triggered, which correlates with increases of IL-6 in cord blood 5 , 19 and with the increase of MMP-8 in amniotic fluid 3 , 20 , 24. It has already been reported that the use of steroids in the prenatal period could reduce various postnatal effects regarding inflammatory response ( 25. The possible beneficial effect that would tend to lower the frequency of HCA should be handled with caution and be subject to future analysis. However, the effect of CA on brain injury, specifically on the frequency of cerebral palsy 21, and the potential deleterious effects on neurodevelopment are under discussion 26.
In brain tissue, cytokines have the capacity to permeability alter the BBB and produce tissue disruption when exposed to hypoxia 6, ischemia 2 , 7, sepsis 27 or necrotizing enterocolitis 6. During this ischemic and inflammatory process, cells of the microglia 12 , 19 and astroglia can be activated, producing free radicals and a greater amount of cytokines (IL-α, ILβ, IL-6 and IL-8) that directly damage the pre-oligodendrocytes 19 and induce apoptosis through the caspase pathway 6. In this regard, Volpe explains that vulnerability of preoligodendrocytes and subplate neurons develops between 24 and 32 weeks of gestation 7 , 27.
Since CA is based on clinical criteria that can lead to false positives or negatives 3 , 5 , 24, we used an analysis model that relates HCA to neurological damage by age. Surprisingly, 42% of placentas examined presented HCA, a frequency that is at the upper limit of national and international reports 3 , 28. Although most of the affected placentas showed early stage infiltration 3 , 20 when the chorion and amnion were affected simultaneously, the risk of neurological damage doubled or tripled both in the first week of life and between 7 and 30 days, with different patterns of associated brain damage, rarely described in the literature.
The brain lesions often were hemorrhagic, ischemic and affected white matter. Except for meningitis, all were identified by brain ultrasound, a method chosen for its great accessibility and efficiency in determining the type and extent of brain injury 20. The noteworthy SLV frequency, a type of white matter lesion related to inflammatory processes, was followed by IVH, as already described in our setting 8.
The adjusted analysis by HCA subtypes, excluding confounding factors, and according to age allowed us to determine the association with some brain injuries. Only the concurrent condition of having both, chorion and amnion affection, was related to risk of damage. For IVH, the risk doubled during the first week, possibly due to the association of the inflammatory component with capillary fragility 29, independent from other factors 2. In contrast, the risk for PVL and SLV type white substance lesions tripled between 7 and 30 days of age, possibly due to the inflammatory and ischemic mechanisms described above 7 , 19.
However, at 40 weeks of corrected age no association was found despite controlling for the confounding effects of preceding injuries and concurrent systemic diseases. We consider that cerebral hypoplasia and other injuries were the effect of multiple combined processes among which malnutrition, metabolic disorders (hypoglycemia, hyperbilirubinemia), bronchopulmonary dysplasia, pneumonia, late sepsis and necrotizing enterocolitis stand out, among these the inflammatory effect of HCA itself is diminished ( 7 , 20 , 26. Other very small or diffuse brain lesions that would have improved the analysis were not identified due to lack of magnetic resonance imaging 29 , 31.
This study has shown that various inflammatory mechanisms contribute to brain damage. The main one was placental infection that leads to sepsis; since there is no evidence that meningitis plays a fundamental role in brain damage, we consider that the inflammatory factor derived from the sepsis itself would be responsible for the long-term harmful effect 26 , 29. Other infectious and inflammatory processes, such as pneumonia, necrotizing enterocolitis, persistent ductus arteriosus and hyaline membrane disease, were associated with greater neurological damage, especially between 7 and 30 days of life 29, which opens up a series of possibilities for the management and control of cerebral lesions by age, which require further analysis in the future.
However, recent studies have concluded that there is insufficient evidence to justify the association between HCA and brain injury in preterm infants 30 , 32. Only the study by Pappas et al. 29 found a correlation between severe IVH and HCA. None of the studies after 2005 found any association with PVL, the best-known type of lesion. However, the hypothesis remains in question because these clinical studies differ in methodology and conversely there is adequate experimental support. Shi et al 21, based on a systematic review and meta-analysis, noted that HCA is associated with risk of cerebral palsy when studies are prospective and start from the presence or absence of chorioamnionitis. Others emphasize analyzing amnion involvement 32. On the long-term effects, Ylijoki et al. showed that HCA was associated with lower cognitive performance, memory and learning skills at 5 years of age 26.
The effects on lower gestational age premature infants was of particular interest. These infants are more frequently and extensively brain damaged, at the expense of white matter; and are likely to have smaller cranium size. These findings have long been described 7 , 19 and generally translate into severe disabilities in early childhood 16. However, there are many related factors, in which the role of HCA has not been clearly defined 23 , 26.
Based on current knowledge, future projects should take into account types (acute and chronic) and grades of CA, germs, umbilical cord clamping, fetal inflammatory response (funisitis and amnion), maternal inflammatory response, circulation of deleterious and protective cytokines, use of prenatal and postnatal steroids, head circumference monitoring, MRI findings and neurodevelopmental examinations 3 , 6 , 30.
One of the strengths of the study is that the anatomopathological examinations of the placenta were available, and neurological diagnoses were performed by neurologists trained in brain ultrasound. Likewise, an analysis model by age was carried out, understanding the importance of the physiopathology of brain injuries in premature infants. Also, a multivariate analysis was performed, which allowed considering confounding factors. As a limitation, it should be mentioned that the time of umbilical cord clamping was not recorded. Late sepsis, which could be a confounding variable on the effect at 40 weeks, was also not differentiated, and no membrane culture or amniotic fluid culture was obtained that could better explain the germ’s virulence factor.
In conclusion, HCA was found in almost half of all preterm births under 34 weeks. Premature rupture of membranes was the main cause of neonatal sepsis, and in turn sepsis was associated with neurological damage. Chorioamnionitis caused brain damage in preterm infants aged 0-7 days and 7-30 days. The most frequent injuries were IVH and damage to white matter (SLV and PLV). At 40 weeks of corrected age, extreme preterm infants with HCA had more extensive brain damage.
Acknowledgement:
To Dr. Rodrigo Carrillo for editing and contributing to the development of the manuscript and promoting publication of research papers by the Alberto Hurtado School of Medicine of Universidad Peruana Cayetano Heredia. To the assistant doctors, residents, medical interns and obstetrics graduates of the Neonatology and Obstetrics wards of Hospital Cayetano Heredia.
REFERENCES
1. Eastman NJ, De Leon M. The etiology of cerebral palsy. Am J Obstet Gynecol. 1955; 69:950-61. doi: 10.1016/0002-9378(55)90094-6. [ Links ]
2. Kaukola T, Herva R, Perhomaa M, Paakko E. Population Cohort Associating Chorioamnionitis, Cord Inflammatory Cytokines and Neurologic Outcome in Very Preterm, Extremely Low Birth Weight Infants. Pediatr Res. 2006;59:478-83. [ Links ]
3. Kim C, Romero R, Chaemsaithong P, Chaiyasit N, Yoon B, Kim Y. Acute chorioamnionitis and funisitis: definition, pathologic features, and clinical significance. Am J Obstet Gynecol. 2015;213(4):S29-S52. doi: 10.1016/j.ajog.2015.08.040. [ Links ]
4. Ministerio de Salud. Análisis de la situación de salud de la provincia de Lima 2011 [Internet]. Lima: Dirección General de Epidemiologia, MINSA; 2011. Disponible en: http://bvs.minsa.gob.pe/local%20/MINSA/1778.pdf. [ Links ]
5. Edwards RK. Corioamnionitis y parto. Clinic Obstet Ginecol Norteam. 2005;32:287-96. [ Links ]
6. McAdams RM, Juul SE. The Role of Cytokines and Inflammatory Cells in Perinatal Brain Injury. Neurol Res Int. 2012:1-15. doi: 10.1155/2012/561494. [ Links ]
7. Volpe JJ. Neurology of the Newborn. Sixth Edition. Elsevier Health Ed; 2018. [ Links ]
8. Guillén D. Diagnóstico de las Lesiones Cerebrales de los Prematuros Menores de 34 semanas: Incidencia, Factores asociados y Pronóstico [tesis doctoral]. Lima: Universidad Peruana Cayetano Heredia; 2004. [ Links ]
9. Gaudet LM, Smith GN. Cerebral Palsy and chorioamnionitis: The inflammatory cytokine link. Obstet Gynecol Surve. 2001;56(7):433-36. [ Links ]
10. Graham EM, Holcroft CJ, Rai KK, Donohue PK, Allen MC. Neonatal cerebral white matter injury in preterm infants is associated with culture positive infections and only rarely with metabolic acidosis. Am J Obstet Gynecol. 2004;191:1305-10. [ Links ]
11. Hagberg H , Mallard C , Ferriero DM , Vannucci SJ , Levison SW , Vexler ZS , et al. The role of inflammation in perinatal brain injury. Nat Rev Neurol. 2015;11(4):192-208. doi: 10.1038/nrneurol.2015.13. [ Links ]
12. Dammann O, Leviton A. Infection remote from the brain, neonatal white matter damage, and cerebral palsy in the preterm infant. Seminar Pediatr Neurol. 1998;5(3):190-201. [ Links ]
13. Harry GJ, Lawler C, Brunseen SH. Maternal infection and white matter toxicity. Neurotoxicology. 2006; 27: 658-70. [ Links ]
14. Chau V, Poskitt KJ, McFadden D, Bowen-Roberts T, Synnes A, Brant R. Effect of Chorioamnionitis on Brain Development and Injury in Premature Newborns. Ann Neurol. 2009; 66:155-64. doi: 10.1002/ana.21713. [ Links ]
15. Ylijoki M, Ekholm E, Haataja L, Lehtonen L. Is chorioamnionitis harmful for the brain of preterm infants? A clinical overview. Acta Obstet Gynecol Scand. 2012;91(4):403-19. doi: 10.1111/j.1600-0412.2012.01349.x. [ Links ]
16. Medina-Alva P, Duque KR, Zea-Vera A, Bellomo S, Cárcamo C, Guillén-Pinto D, et al. Combined predictors of neurodevelopment in very low birth weight preterm infants. Early Hum Dev. 2019;130:109-15. doi: 10.1016/j.earlhumdev.2019.01.019. [ Links ]
17. Zea-Vera A, Turin CG, Ochoa TJ. Unificar los criterios de sepsis neonatal tardía: propuesta de un algoritmo de vigilancia diagnóstica. Rev Peru Med Exp Salud Publica. 2014;31(2):358-63. [ Links ]
18. Norma técnica para la atención integral de salud neonatal. Resolución N° 828-2013/MINSA [Internet]. Ministerio de Salud; 2015. Disponible en: http://bvs.minsa.gob.pe/local/minsa/3281.pdf. [ Links ]
19. Volpe JJ. Brain Injury in premature infants: a complex amalgam of destructive and developmental disturbances. Lancet Neurol. 2009; 8:110-24. doi: 10.1016/S1474-4422(08)70294-1. [ Links ]
20. Maisonneuve E, Ancel P, Foix-L'Hélias L, Marret S, Kayem G. Impact of clinical and/or histological chorioamnionitis on neurodevelopmental outcomes in preterm infants: A literature review. J Gynecol Obstet Hum Reprod. 2017;46(4):307-316. doi: 10.1016/j.jogoh.2017.02.007. [ Links ]
21. Shi Z, Ma L, Luo K, Bajaj M, Chawla S, Natarajan G, et al. Chorioamnionitis in the Development of Cerebral Palsy: A Meta-analysis and Systematic Review. Pediatrics 2017;139(6):e20163781. doi: 10.1542/peds.2016-3781. [ Links ]
22. Rincón I, Magdaleno F, Sancha N, Omeñaca F, González A. Corioamnionitis histológica y morbimortalidad neonatal: Aproximación al síndrome de respuesta inflamatoria fetal. Rev Chil Obstet Ginecol. 2010;75(3):172-8. [ Links ]
23. Pugni L, Pietrasanta C, Acaia B, Merlo D, Ronchi A, Ossola M, et al. Chorioamnionitis and neonatal outcome in preterm infants: a clinical overview. J Matern Fetal Neonatal Med. 2016;29(9):1525-29. doi: 10.3109/14767058.2015.1053862. [ Links ]
24. Chaiyasit N, Romero R, Chaemsaithong P, Docheva N, Bhatti G, Kusanovic JP, et al. Clinical chorioamnionitis at term VIII: a rapid MMP-8 test for the identification of intra-amniotic inflammation. J Perinat Med. 2017: 26;45(5):539-550. doi: 10.1515/jpm-2016-0344. [ Links ]
25. Amiya RM, Mlunde LB, Ota E, Swa T, Oladapo OT, Mori R. Antenatal Corticosteroids for Reducing Adverse Maternal and Child Outcomes in Special Populations of Women at Risk of Imminent Preterm Birth: A Systematic Review and Meta-Analysis. PLoS One. 2016;11(2):e0147604. doi: 10.1371/journal.pone.0147604. [ Links ]
26. Ylijoki M, Lehtonen L, Lind A, Ekholm E, Lapinleimu H, Kujari H, et al. Chorioamnionitis and Five-Year Neurodevelopmental Outcome in Preterm Infants. Neonatology. 2016;110(4):286-295. [ Links ]
27. Khwaja O, Volpe JJ. Pathogenesis of Cerebral White matter injury of prematurity. Arch Dis Child Fetal Neonatal Ed. 2008;2:153-61. doi: 10.1136/adc.2006.108837. [ Links ]
28. Instituto Nacional de Estadística e Informática. Encuesta Demográfica y de Salud Familiar 2015 [Internet]. Lima: INEI; 2015. Disponible en: https://www.inei.gob.pe/media/MenuRecursivo/publicaciones_digitales/Est/Lib1356/. [ Links ]
29. Pappas A, Kendrick D, Shankaran S, Stoll B, Bell E, Laptook A, et al. Chorioamnionitis and Early Childhood Outcomes Among Extremely Low-Gestational-Age Neonates. JAMA Pediatrics. 2014;168(2):137-47. [ Links ]
30. Chau V, McFadden D, Poskitt KJ, Miller SP. Chorioamnionitis in the Pathogenesis of Brain Injury in Preterm Infants. Clin Perinatol. 2014;41:83-103. doi: 10.1016/j.clp.2013.10.009. [ Links ]
31. Anblagan D, Pataky R, Evans MJ, Telford EJ, Serag A, Sparrow S, et al. Association between preterm brain injury and exposure to choriamnionitis during fetal life. Sci Rep. 2016;6:37932. doi: 10.1038/srep37932. [ Links ]
32. Rocha G, Proenca E, Quintas C, Rodrigues T, Guimaraes H. Chorioamnionitis and brain damage in preterm Newborn. J Matern Fetal Neonatal Med. 2007;20(10):745-9. doi: 10.1080/14767050701580515. [ Links ]
Citation: Guillén N, Llerena C, Samalvides S, Vila J, Juárez T, Cáceres J, et al. Risk of brain damage in premature infants under 34 weeks of gestational age exposed to histological chorioamnionitis Lima, Peru. Rev Peru Med Exp Salud Publica. 2020;37(2):229-38. doi: https://doi.org/10.17843/rpmesp.2020.372.4779.
Received: September 03, 2019; Accepted: April 29, 2020











 texto en
texto en