Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista Peruana de Medicina Experimental y Salud Publica
versão impressa ISSN 1726-4634
Rev. perú. med. exp. salud publica vol.37 no.3 Lima jul-sep 2020
http://dx.doi.org/10.17843/rpmesp.2020.373.4787
Original articles
Clinical-epidemiological analysis of HDL2 and HDL3 subfractions in adults from Maracaibo city, Venezuela
1 Centro de Investigaciones Endocrino-Metabólicas «Dr. Félix Gómez», Escuela de Medicina, Universidad del Zulia, Maracaibo, Venezuela.
2 Universidad Simón Bolívar, Facultad de Ciencias de la Salud, Barranquilla, Colombia.
3 Universidad Técnica de Ambato, Ambato, Ecuador.
4 Pulmonary and Critical Care Medicine Department, Brigham and Women’s Hospital, Harvard Medical School, Boston, Massachusetts, Estados Unidos.
INTRODUCTION
High density lipoproteins (HDL) are macromolecular, pseudo-micellar complexes whose most well-known function is to transport cholesterol from peripheral tissues to the liver for metabolism and excretion, a process known as reverse cholesterol transport (RCT). These lipoproteins also have antithrombotic, anti-inflammatory, vasodilatory, immunosuppressive and antioxidant properties 1. This has led to the consideration for years of HDL as protective molecules for cardiovascular disease (CVD), which is considered a global public health problem and the first cause of death worldwide; it caused 17.8 million deaths in 2017 2. In the population of Maracaibo, high prevalence of low levels of high-density lipoprotein cholesterol (HDL-C) has been previously observed 3; however, the coronary risk seems to be lower than in other populations with lower frequency of this type of lipid alteration 4.
Although there is epidemiological evidence that HDL-C is an independent predictor of CVD, clinical pharmacological trials focused on its quantitative improvement have not demonstrated benefit in reducing cardiovascular events or mortality 5. This paradoxical phenomenon has been justified due to the heterogeneity and complexity shown by these molecules, whose functionality is the fundamental characteristic in their role as cardiovascular “protector” 6. In this regard, there seems to be a close relationship between the function and the subfractions or subspecies of HDL-C 7.
De Lalla et al. 8 described for the first time the distribution of HDL-C subfractions and identified two subclasses: HDL2, the least dense (1.063-1.125 g/mL) and richer in lipids; and HDL3, the most dense (1.125-1.21 g/mL) and relatively rich in proteins. HDL2 and HDL3 seem to have different functions. HDL3 has the ability to receive free cholesterol from the endothelium or macrophages, through the ATP-binding cassette transporter A-1 (ABCA- 1), increasing its size with the decrease of its density, thus transforming into HDL2, which is responsible for the RCT by binding to SR-B1 receptors. Therefore, the role of each subfraction in cardiometabolic health could be different 9.
Epidemiologic findings related to subfractions are diverse and controversial, that is why no international diagnostic and management guidelines for dyslipidemia currently recommend routine evaluation in patients with cardiovascular risk. However, several reports show the potential role that these subfractions would have as markers for HDL functionality, and the modulating effect that drugs would have on CVD 7 , 10.
In Latin America, especially in Venezuela, although low HDL-C is a frequent dyslipidemia, there are few or no reports describing the behavior of HDL subfractions or their relationship to other cardiovascular risk factors. Therefore, the aim of this study was to perform a clinical-epidemiological analysis of HDL2 and HDL3 subfractions in an adult population in the city of Maracaibo, Venezuela.
KEY MESSAGES
Motivation for the study: The epidemiological behavior of HDL-C subfractions and their relationship with other metabolic alterations in Latin American populations, especially in Venezuela, is unknown.
Main findings: The average of HDL-C subfractions was lower in men; differences were only evident in subjects with low HDL-C. Subfractions had variable behavior and lower levels were observed in men and women with clinical and metabolic disorders.
Implications: HDL-C subfractions represent laboratory parameters of potential utility in individuals with low HDL-C. Their measurement in this context would allow early identification of subjects with risk factors, especially in those with intermediate or low cardiovascular risk.
MATERIALS AND METHODS
Population and sample
The data for this investigation came from the “Estudio de Prevalencia de Síndrome Metabólico de la Ciudad de Maracaibo (EPSMM)”, a cross-sectional, descriptive, analytical, multi-stage random sampling study. It included 2,230 adults of both sexes, residents of Maracaibo, and it was designed to identify and evaluate risk factors for metabolic syndrome and cardiovascular disease. The main study sample was calculated on the basis of census estimates from the National Institute of Statistics for the city of Maracaibo in 2007; it included a population of 1,428,043 inhabitants over 18 years; the calculated sample was 2,230 subjects selected randomly and stratified in the 18 parishes that make up the city. The protocol was described above 11.
A sub-analysis with data obtained from EPSMM was performed to study HDL subfractions. Due to the lack of resources to identify subfractions in all subjects with low HDL-C, 359 individuals were randomly selected from the database using the SPSS program’s random number tool, maintaining an equitable distribution by sex, age groups and presence of low HDL-C. For this subsample of individuals, HDL subfraction data were collected and processed as part of the study in 2012.
Procedure
Evaluation of the subjects
Previously trained personnel completed the participants’ medical record with information related to age, sex, race, employment and socioeconomic status, educational level, family, and pathological history of endocrine-metabolic or cardiovascular disease. Socioeconomic status was classified as, stratum I (upper class), stratum II (upper-middle class), stratum III (middle class), stratum IV (working class), and stratum V (extreme poverty). Educational level was classified as, up to primary school (those who did not have any knowledge of reading or writing or those who completed primary education), secondary (all those who completed secondary education), and higher (all those who completed some degree of higher education).
Regarding psychobiological habits, smoking was categorized into 1) current smokers, 2) non-smokers, and 3) ex-smokers (at least one year after quitting). Alcohol consumption was defined as the intake of >1 g/day. Physical activity levels were determined using the long version of the International Physical Activity Questionnaire (IPAQ) and were classified into two large groups: 1) those individuals with MET’s = 0 (none) and 2) those with MET’s > 0 (some degree of physical activity). This last group was later divided into quintiles, resulting in the following classification: Q1 or very low (men: <296.9; women: <230.9), Q2 or low (men: 297.0-791.9; women: 231.0-445.499), Q3 or moderate (men: 792.0-1,532.3; women: 445.5-742.4), Q4 or high (men: 1,532.4- 2,879.9; women: 742.5-1,798.4), Q5 or very high (men: ≥2,880.0; women: ≥1798.5).
Clinical evaluation
A calibrated and validated sphygmomanometer was used to measure the participants’ blood pressure. The criteria proposed in the seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC-7) were used to classify the population into normotensive, prehypertensive, and hypertensive 12.
In addition, an anthropometric evaluation was carried out to determine weight, by using a digital scale (Tanita, TBF-310 GS Body Composition Analyzer, Tokyo-Japan); and height, with a calibrated measuring rod. The body mass index (BMI) was calculated using Quetelec’s formula (weight/height2) and the subjects were classified according to the criteria from the World Health Organization (WHO): underweight (<18.5 kg/m2), normal weight (18.5-24.9 kg/m2), overweight (25.0-29.9 kg/m2), obesity (≥30.0 kg/m2) 13. The abdominal circumference was measured using a metric measuring tape, taking as an anatomical reference an equidistant point between the costal ridge and the anterior superior iliac crest. The values for abdominal obesity were ≥90 cm for men and ≥80 cm for women according to the criteria of the IDF/NHLBIAHA/WHF/IAS/IASO consensus 14, as well as the diagnosis of metabolic syndrome (MS).
Laboratory analysis
After 8 hours of fasting, serum glucose, total cholesterol and triacylglyceride levels were calculated using commercial enzymatic-colorimetric kits (Human Gesellshoft Biochemica and Diagnostica MBH, Hessen, Germany) and specialized computerized equipment. LDL-C levels were calculated using Friedewald’s formula. Serum levels of ultra-sensitive C-reactive protein (us-CRP) were quantified by immunoturbodimetric assays (Human Gesellshoft Biochemica and Diagnostica MBH, Hessen, Germany), using ≥0.765 mg/L as a cut-off point to define elevated levels 15. The basal insulin concentration was determined using a commercial kit based on the ELISA method (DRG International, Inc., USA, New Jersey), with <1 mU/L as a detection limit. On the other hand, the lipoprotein values (Lp(a)) were estimated through the turbidimetric latex method (Human Gesellschaft für Biochemica and Diagnostica, Hessen, Germany). The cut-off point for considering elevated Lp(a) values was ≥30 mg/dL 16. HOMA2-IR values to define insulin resistance (IR) were calculated with software (HOMA-Calculator v2.2.3) supplied by the Oxford Centre for Diabetes Endocrinology and Metabolism, available at http://www.dtu.ox.ac.uk/homacalculator/index.php. The cut-off point used for HOMA2-IR was 2.0, previously established for the study population 17.
HDL we4re isolated according to the sequential ultracentrifugation method, dialyzed against a 0.09M Tris - 0.08M boric acid - EDTANa23Mm, pH=8.35 buffer solution (TBE). Then, polyacrylamide gel gradient electrophoresis under non-denaturing conditions was carried out, with protein markers calibrated for molecular diameter (thyroglobulin 17.0 nm; ferritin 12.2 nm; catalase 10.4 nm; lactate dehydrogenase 8.1 nm, and albumin 7.1 nm; Amersham Pharmacia Biotech, Buckimghamshire, United Kingdom). Total protein was quantified by a modification of Lowry’s method, HDL protein bands were stained with Coomassie blue R-250 and the average diameter was determined by optical densitometry.
Estimation of the relative apolipoprotein content was carried out by polyacrylamide 4-21% gradient electrophoresis of HDL, staining the apolipoproteins with Coomassie blue R-250, then the gel was analyzed by optical densitometry. The results are expressed as the percentage that represents the area under the curve for each apolipoprotein according to the sum of the areas of the HDL apolipoproteins. The Quantolip® HDL (HDL2/HDL3) kit (Technoclone, Vienna, Austria) was used to isolate HDL subfractions. The HDL2/HDL3 index was also calculated to evaluate the relationship between these variables.
Statistical analysis
Nominal and ordinal variables are presented as absolute and relative frequencies. Association between qualitative variables was determined using the Chi-square test, and the normality of the quantitative variables was evaluated with the Kolmogorov-Smirnov Z test. These variables were presented by means ± standard deviation (SD). When comparing averages between groups, the t-Student test was used to compare two groups and the one-factor variance analysis (ANOVA) for more than two groups. A value of p < 0.05 was considered significant, and a statistical analysis was performed with the SPSS 20.0 program (IBM, USA).
Ethical aspects
The ethics committee of the Centro de Investigaciones Endocrino-Metabólicas (CIEM) “Dr. Félix Gómez” of the Universidad del Zulia, Venezuela, approved the study and authorized the use of the database for this sub-analysis. All participants signed an informed consent form prior to any intervention, interrogation, and physical examination.
RESULTS
Characteristics of the population
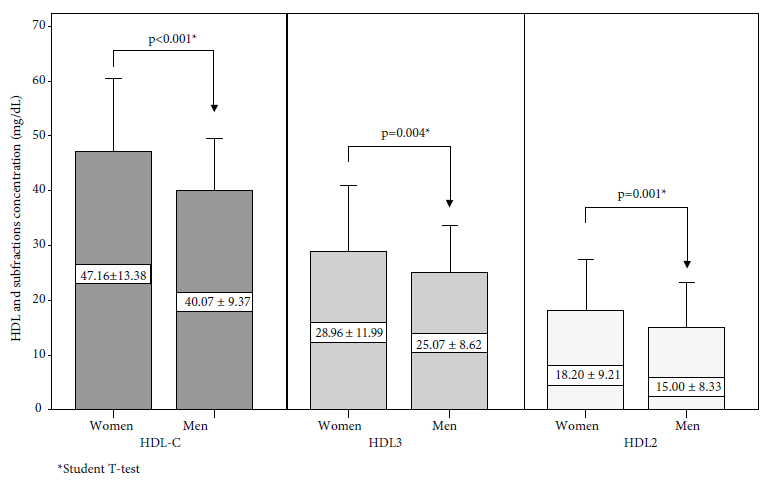
Table 1 shows general characteristics of the studied sample, made up of 359 individuals, of which 51.5% (n = 185) were female. The average age of the population was 39.4 ± 15.2 years. Regarding HDL-C behavior according to sex (Figure 1), it was shown that concentration of this lipoprotein was significantly higher in women than men (47.2 ± 13.4 mg/dL vs. 40.1 ± 9.4 mg/dL; p < 0.001). Also, statistically significant differences were found in the concentration of HDL3 (women: 28.9 ± 11.9 mg/dL vs. men: 25.1 ± 8.6 mg/dL; p = 0.004) and HDL2 (women: 18.2 ± 9.2 mg/dL vs. men: 15.0 ± 8.3 mg/dL; p = 0.001).
Table 1 General characteristics of the studied population
| Characteristics | Women | Men | Total | |||
|---|---|---|---|---|---|---|
| (n = 185) | (n = 174) | (n = 359) | ||||
| n | % | n | % | n | % | |
| Age group (years) | ||||||
| <30 | 54 | 29.2 | 67 | 38.5 | 121 | 33.7 |
| 30-49 | 71 | 38.4 | 63 | 36.2 | 134 | 37.3 |
| ≥50 | 60 | 32.4 | 44 | 25.3 | 104 | 29.0 |
| Marital status | ||||||
| Single | 95 | 51.4 | 82 | 47.1 | 177 | 49.3 |
| Married | 90 | 48.6 | 92 | 52.9 | 182 | 50.7 |
| Employment status | ||||||
| Employed | 81 | 43.8 | 135 | 77.6 | 216 | 60.2 |
| Unemployed | 104 | 56.2 | 39 | 22.4 | 143 | 39.8 |
| Educational level | ||||||
| Up to primary school | 38 | 20.5 | 20 | 11.5 | 58 | 16.2 |
| Secondary | 78 | 42.2 | 88 | 50.6 | 166 | 46.2 |
| Higher | 69 | 37.3 | 66 | 37.9 | 135 | 37.6 |
| Socioeconomic stratum | ||||||
| I-II | 34 | 18.4 | 35 | 20.1 | 69 | 19.2 |
| III | 87 | 47.0 | 77 | 44.3 | 164 | 45.7 |
| IV-V | 64 | 34.6 | 62 | 35.6 | 126 | 35.1 |
| Race | ||||||
| Mestizo | 141 | 76.6 | 134 | 77.0 | 275 | 76.8 |
| White-Hispanic | 24 | 13.0 | 26 | 14.9 | 50 | 14.0 |
| Afro-Venezuelan | 3 | 1.6 | 5 | 2.9 | 8 | 2.2 |
| American Indian | 16 | 8.7 | 9 | 5.2 | 25 | 7.0 |
| Alcohol consumption * | ||||||
| Yes | 33 | 17.8 | 100 | 57.5 | 133 | 37,0 |
| No | 152 | 82.2 | 74 | 42.5 | 226 | 63,0 |
| Tobacco smoking habits | ||||||
| No | 153 | 82.7 | 111 | 63.8 | 264 | 73.5 |
| Smoker | 14 | 7.6 | 26 | 14.9 | 40 | 11.1 |
| Ex-smoker | 18 | 9.7 | 37 | 21.3 | 55 | 15.3 |
| Leisure physical activity | ||||||
| None | 127 | 68.6 | 82 | 47.1 | 209 | 58.2 |
| Extremely low | 7 | 3.8 | 19 | 10.9 | 26 | 7.2 |
| Low | 19 | 10.3 | 15 | 8.6 | 34 | 9.5 |
| Moderate | 11 | 5.9 | 21 | 12.1 | 32 | 8.9 |
| High | 10 | 5.4 | 14 | 8.0 | 24 | 6.7 |
| Extremely high | 11 | 5.9 | 23 | 13.2 | 34 | 9.5 |
| Low HDL-C | ||||||
| No | 86 | 46.5 | 84 | 48.3 | 170 | 47.4 |
| Yes | 99 | 53.5 | 90 | 51.7 | 189 | 52.6 |
AF: actividad física.
*Consumidor >1 g/día
HDL-C subfraction percentiles
Table 2 shows the percentile distribution of HDL-C subfractions by sex. The average HDL3 in women was 26.7 mg/dL (P25-P75: 19.9-36.9); 17.6 mg/dL (P25-P75: 10.7-24.6) for HDL2; and 0.66 (P25-P75: 0.35-1.02) for the HDL2/HDL3 ratio. While the HDL3 average in men was 24.8 mg/dL (P25-P75: 18.9-30.5); 13.8 mg/dL (P25-P75: 9.2-18.1) for HDL2; and 0.56 (P25-P75: 0.35-0.83) for the HDL2/HDL3 ratio.
Table 2 Percentiles of HDL subfractions in the population studied.
| Variable | p25 | p33.3 | Median | p66.6 | p75 | p95 |
|---|---|---|---|---|---|---|
| Women (n = 185) | ||||||
| HDL3 (mg/dL) | 19.9 | 22.7 | 26.7 | 33.1 | 36.9 | 49.8 |
| HDL2 (mg/dL) | 10.7 | 13.0 | 17.6 | 20.8 | 24.6 | 36.0 |
| HDL2/HDL3 | 0.35 | 0.43 | 0.66 | 0.86 | 1.02 | 1.89 |
| Men (n = 174) | ||||||
| HDL3 (mg/dL) | 18.9 | 21.0 | 24.8 | 28.9 | 30.5 | 42.2 |
| HDL2 (mg/dL) | 9.2 | 10.9 | 13.8 | 16.1 | 18.1 | 33.6 |
| HDL2/HDL3 | 0.35 | 0.41 | 0.56 | 0.74 | 0.83 | 2.47 |
p: percentile
HDL-C subfractions according to socio-demographic characteristics and habits
Table 3 shows the behavior of HDL2 and HDL3 in individuals with low HDL-C according to sociodemographic variables. Women from socioeconomic strata IV-V presented significantly lower values of HDL3 compared to those from higher socioeconomic strata (p < 0.001). Likewise, women from strata IV-V 4presented a higher HDL2/HDL3 ratio with respect to those from strata I-II (0.9 ± 0.5 vs. 0.7 ± 0.6, respectively; p = 0.012).
Table 3 HDL subfractions according to sociodemographic characteristics and habits in subjects with low HDL-C.
SD: standard deviation.
§Consumer >1 g/day.
* t-Student test to compare between two categories, or one-factor ANOVA test to compare between three or more categories. In patients with normal HDL, no significant differences were observed between group means.
Regearding race, a higher concentration of HDL2 and a higher HDL2/HDL3 ratio were evidenced in American Indians compared to white-Hispanic individuals (HDL2: 17.8 ± 5.0 mg/dL vs. 9.8 ± 4.2 mg/dL; p = 0.040 and HDL2/HDL3: 1.1 ± 0.45 vs. 0.5 ± 0.3; p = 0.007, respectively). On the contrary, in men with low HDL-C, no significant differences were found in the subfraction averages with respect to the sociodemographic variables.
As for psychobiological habits, non-smoker women presented higher levels of HDL3 with respect to ex-smokers (22.4 ± 6.6 mg/dL vs. 17.1 ± 7.6 mg/dL, respectively, p = 0.034). On the contrary, men with low HDL-C only showed significant differences between the level of leisure physical activity and the HDL2/HDL3 ratio (p = 0.038), without observing important differences between the ratio values for each activity type.
HDL-C subfractions according to clinical-metabolic characteristics
Regarding clinical-metabolic alterations, it was observed (Table 4) that women with low HDL-C and hypertriglyceridemia showed significantly lower HDL3 and HDL2 serum concentrations compared to those with normal triglycerides (TG) (p = 0.033 and p = 0.034, respectively). Similar findings have been reported in women with elevated us-CRP, in whom lower HDL3 concentration and HDL2/HDL3 ratio were observed, compared to those with normal us-CRP (p < 0.001 and p = 0.011, respectively). In men with hypertension a significantly lower concentration of HDL2 (p = 0.031), HDL3 (p = 0.028) and ratio HDL2/HDL3 (p = 0.028) was evidenced. Likewise, these individuals showed a significantly lower concentration of HDL2 in the presence of IR (p = 0.050) and MS (p = 0.003) and men with elevated us-CRP also showed a lower concentration of HDL3 (p = 0.011).
Table 4 HDL Subfractions according to clinical-metabolic characteristics and sex of subjects with low HDL-C
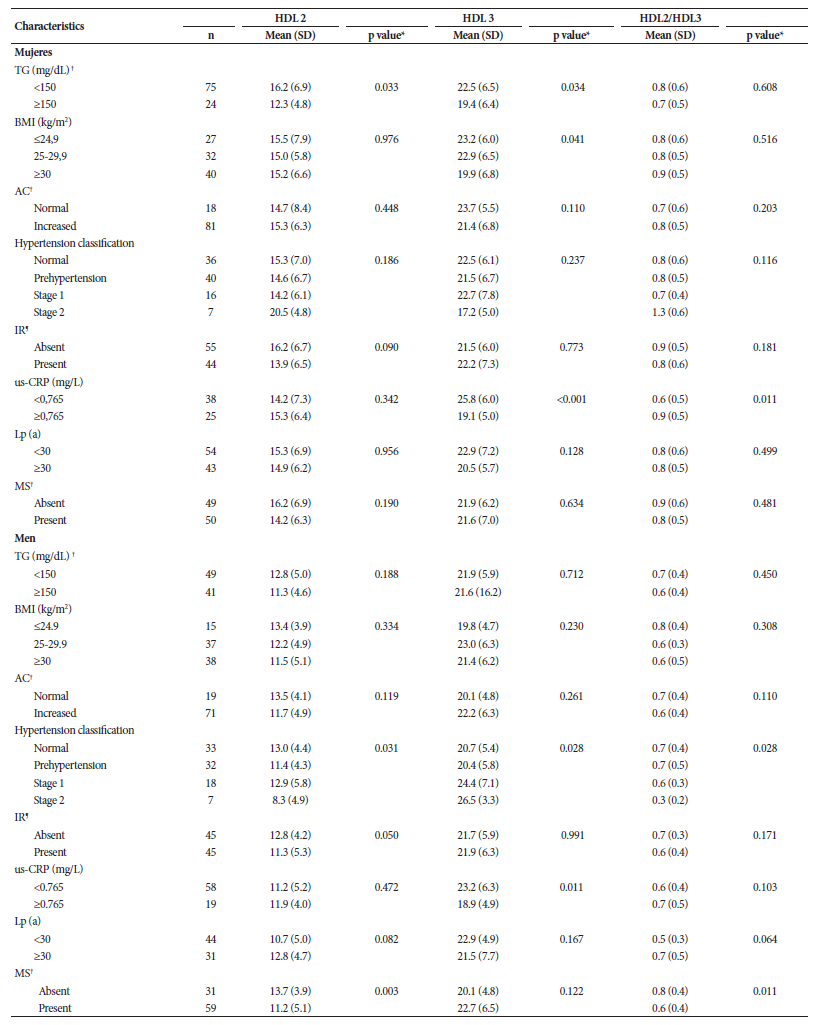
TG: triacylglycerides; BMI: body mass index; AC: abdominal circumference; IR: insulin resistance; us-CRP: ultra-sensitive C-reactive protein; MS: metabolic syndrome.
† Criteria according to IDF/NHLBI/AHA consensus; ¶ Criteria according to EPSMM (HOMA2-IR≥2).
* t-Student test to compare between two categories, or single-factor ANOVA test to compare between three or more categories in patients with normal HDL; no significant differences between group means were observed.
DISCUSSION
HDL are molecules that can exist in multiple isoforms, and heterogeneity is one of their main properties. Although the HDL-C concentration has been inversely correlated to the risk of CVD and atherosclerosis, heterogeneity confers additional effects to its anti-atherogenic properties, which are attributed to the various molecules are part of the HDL-C 6.
For decades it has been suggested that HDL subfractions could be more directly related to the occurrence of cardiovascular events; however, despite positive results, there is no conclusive evidence about which subclass is the most important in this context 10 , 18 , 19. This probably influences the absence of international recommendations for using these biochemical parameters. In fact, HDL subfractions are not mentioned in the most recent North American or European guidelines for diagnosis and management of dyslipidemia.
Given this controversial scenario and the lack of reports evaluating HDL subclasses in Latin American populations, especially in Venezuela, this study describes the main clinical and epidemiological characteristics of HDL subfractions in the population of the city of Maracaibo, the second most important city in Venezuela in terms of population and economy. In fact, during the sample collection period, Maracaibo presented a high frequency of cardiovascular risk factors and deleterious psychobiological habits, such as sedentarism and high consumption of saturated fats 20 , 21.
It is important to show average values and dispersion measures for any epidemiological analysis of a laboratory measurement with scarce reports from a region or country. When comparing the HDL-C subfraction results from this study, with other populations, we found different figures. For example, in a European population, Kim et al. 22 found a higher HDL3 average (women: 49 ± 11 mg/dL and men: 39 ± 11 mg/dL), and the HDL2 average was higher in women (women: 14.7±7.8 mg/dL and men: 8.5±5.3 mg/dL). In a study by Koumaré et al. 23, the HDL3 average in Burkina Faso was the same for men and women (26.2 mg/dL), while the HDL2 average in men was 15.4 mg/dL, and 18.9 mg/dL in women, similar values to those obtained by this research.
It is important to mention that there are differences in the averages of HDL subfractions in subjects with low HDL-C. In relation to the sociodemographic data, American Indians presented higher levels of HDL2 and HDL2/HDL3 compared to white-Hispanic individuals; this data differs from the study carried out by Martin et al. 24, where there was no evident relation between ethnic groups and the different subfractions of HDL-C.
As for the clinical-metabolic characteristics, it has been described that dyslipidemias represent a frequent cardiovascular risk factor and that high levels of triglycerides frequently coexist with low HDL-C and alterations in the subfraction distribution 25. Our findings show that the levels of both subfractions were significantly lower in women with hypertriglyceridemia, which differs from the results of Jia et al. 26, who observed that hyperlipidemic subjects presented lower levels of HDL2 but higher levels of HDL3 when compared with normolipidemic subjects. Similarly, Gou et al. 27 found that HDL2 levels were significantly lower in women with hypertriglyceridemia than in those with normal triglyceride levels, while the HDL3 average was higher in the latter group. Such differences could be explained by the method used for obtaining HDL-C subfractions and by the size of the sample; however, these results suggest an inverse relationship between hypertriglyceridemia and HDL2.
Also, low HDL-C levels have been associated with low-grade inflammation, IR, and visceral obesity. In this regard, the results obtained show decreased HDL3 levels in subjects with elevated us-CRP in both sexes, while those with MS and IR showed lower HDL2 levels in men. These results match with the findings of the ELSA-Brazil study, one of the few Latin American reports that shows characteristics of HDL-C subclasses in our region, in which the concentration of HDL-C and its subfractions were inversely associated with low grade inflammation, IR and MS 27. Similarly, another Brazilian study that evaluated the impact of IR on the metabolism of different lipoproteins showed lower percentages of the largest subfractions (HDL2 and HDL3) in subjects with IR 28, these findings evidence the role that the structure and function of HDL-C would have as cardioprotective lipoproteins.
The molecular mechanisms involved in the inverse relationship between HDL-C subfractions and inflammatory mediators, such as us-CRP, have not yet been clarified. However, the lower HDL3 levels in subjects with elevated us-CRP could be interpreted as a smaller number of nascent lipoproteins available to mobilize and externalize cholesterol from endothelial foam cells, which would lead to the activation and accumulation of the triggers of the inflammatory phenomenon. Another Latin American study shows lower levels of HDL2 and HDL3 specifically in Peruvian diabetic subjects 29, an association that was not significant in our study.
The values observed in this study for the HDL2/HDL3 ratio only showed relation with the socioeconomic status, race, and us-CRP in women; while in men, relations were observed with physical activity, blood pressure and MS. In this regard, Moriyama et al. 30 carried out several investigations in Japanese population and showed that changes in the HDL2/HDL3 ratio correlate inversely with abdominal circumference and IR, and positively with healthy lifestyle habits, which is why it is used as a useful marker for MS and atherogenic conditions in that population.
Regarding the limitations to this study, the sample size does not allow the generalization of the results to the entire population; the cross-sectional design makes it impossible to establish relationships of causality or recommendation of clinical use of HDL-C subfractions, and the socioeconomic changes that affect the study population during recent years could influence the results shown.
In conclusion, HDL-C subfractions have variable clinical-epidemiological behavior in adult individuals of Maracaibo’s population, lower averages in men, differences in socioeconomic levels only in those with low HDL-C, and no predominance of any subclass according to sociodemographic, clinical and biochemical characteristics. Therefore, it is suggested to deepen the study of these lipoproteins in the Latin American population, emphasizing their relationship with different disorders that lead to a higher cardiometabolic risk.
REFERENCES
1. Besler C, Lüscher T, Landmesser U. Molecular mechanisms of vascu lar effects of High-density lipoprotein: alterations in cardiovascular disease. EMBO Molecular Medicine. 2012;4(4):251-268. doi: 10.1002/emmm.201200224. [ Links ]
2. GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736-88. doi: 10.1016/S0140-6736(18)32203-7. [ Links ]
3. Bermudez V, Salazar J, Rojas J, Martínez MS, Bello L, Añez R, et al. Prevalence, Lipid Abnormalities Combinations and Risk Factors Associated with Low HDL-C Levels in Maracaibo City, Venezuela. J J Commun Med. 2015;1(2):009. [ Links ]
4. Bermúdez V, Salazar J, Bello L, Rojas J, Añez R, Roque W, et al. Coronary Risk Estimation According to a Recalibrated Framingham-Wilson Score in the Maracaibo City Metabolic Syndrome Prevalence Study. The Journal for Cardiology. Photon 2014;107:160-170. [ Links ]
5. Salazar J, Cabrera M, Ramos E, Olivar L, Aguirre M, Rojas J, et al. HDL-C y riesgo de aterosclerosis. Diabetes Internacional. 2013;5(2):42-54. [ Links ]
6. Salazar J, Olivar LC, Ramos E, Chávez-Castillo M, Rojas J, Bermudez V. Dysfunctional High-Density Lipoprotein: An Innovative Target for Proteomics and Lipidomics. Cholesterol. 2015;2015:296417. doi: 10.1155/2015/296417. [ Links ]
7. Martin S, Jones S, Toth P. High-density lipoprotein subfractions: current views and clinical practice applications. Trends Endocrinol Metab. 2014;25(7):329-36. doi: 10.1016/j.tem.2014.05.005. [ Links ]
8. De Lalla OF, Gofman JW. Ultracentrifugal analysis of serum lipoproteins. Methods Biochem Anal. 1954;1:459-478. doi: 10.1002/9780470110171.ch16. [ Links ]
9. Pirillo A, Norata G, Catapano A. High-Density Lipoprotein Subfractions - What the Clinicians Need to Know. Cardiology. 2013;124(2):116-125. doi: 10.1159/000346463. [ Links ]
10. Davidson M. The Battle of the HDL Subfractions. Cardiovasc Revasc Med. 2019;20(11):943-944. doi: 10.1016/j.carrev.2019.09.013. [ Links ]
11. Bermúdez V, Marcano R, Cano C, Arráiz N, Amell A, Cabrera M, et al. The Maracaibo City Metabolic Syndrome Prevalence Study: Design and Scope. Am J Ther. 2010;17(3):288-294. doi: 10.1097/MJT.0b013e3181c121bc. [ Links ]
12. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. JAMA. 2003;289:2560-2571. doi: 10.1161/01.HYP.0000107251.49515.c2. [ Links ]
13. World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser [Internet]. WHO; 2000 [citado el 01 de agosto de 2019]. Disponible en: https://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/. [ Links ]
14. Alberti K, Eckecl R, Grundy S, Zimmer PZ, Cleeman JI, Donato KA, et al. Harmonizing the Metabolic Syndrome: A Joint Interim Statement of the International Diabetes Federation Task Force on Epidemiology and Prevention: National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; International Association for the Study of Obesity. Circulation. 2009;120:1640-45. doi: 10.1161/CIRCULATIONAHA.109.192644. [ Links ]
15. Bermúdez V, Cabrera M, Mendoza L, Chávez M, Martínez M, Rojas J, et al. High-sensitivity c-reactive protein epidemiological behavior in adult individuals from Maracaibo, Venezuela. Revista Latinoamericana de Hipertensión. 2013;8(1):22-29. [ Links ]
16. Bermúdez V, Rojas J, Salazar J, Bello L, Áñez R, Toledo A, et al. Variations of Lipoprotein(a) Levels in the Metabolic Syndrome: A Report from the Maracaibo City Metabolic Syndrome Prevalence Study. J Diabetes Res. 2013;2013:416451. doi: 10.1155/2013/416451. [ Links ]
17. Bermúdez V, Rojas J, Martínez M, Apruzzese V, Chávez-Castillo M, Gonzalez R, et al. Epidemiologic Behavior and Estimation of an Op timal Cut-Off Point for Homeostasis Model Assessment-2 Insulin Resistance: A Report from a Venezuelan Population. Int Sch Res Notices. 2014;2014:616271. doi: 10.1155/2014/616271. [ Links ]
18. Williams P. Fifty-three year follow-up of coronary heart disease versus HDL2 and other lipoproteins in Gofman's Livermore Cohort. J Lipid Res. 2012;53(2):266-272. doi: 10.1194/jlr.M019356. [ Links ]
19. Chaudhary R, Kinderyte M, Chaudhary R, Sukhi A, Bliden K, Tantry U, et al. HDL3-C is A Marker of Coronary Artery Disease Severity and Inflammation in Patients on Statin Therapy. Cardiovasc Revasc Med. 2019;20:1001-6. doi: 10.1016/j.carrev.2018.12.019. [ Links ]
20. Bermudez V, Rojas J, Salazar J, Calvo MJ, Morillo J, Torres W, et al. The Maracaibo city metabolic syndrome prevalence study: primary results and agreement level of 3 diagnostic criteria. Revista Latinoamericana de Hipertensión. 2014;9(4):20-31. [ Links ]
21. Souki A, Sandoval M, Sánchez G, Andrade U, García-Rondón D, Cano C, et al. Intake of saturated fatty acids and sensitivity to insulin in obese young adults in Maracaibo. Revista Latinoamericana de Hipertensión. 2007;3(5):159-165. [ Links ]
22. Kim DS, Burt AA, Rosenthal EA, Ranchalis JE, Eintracht JF, Hatsukami TS, et al. HDL-3 is a superior predictor of carotid artery disease in a case-control cohort of 1725 participants. J Am Heart Assoc. 2014;3(3):e000902. doi: 10.1161/JAHA.114.000902. [ Links ]
23. Koumaré AT, Sakandé LP, Kabré E, Sondé I, Simporé J, Sakandé J. Reference ranges of cholesterol sub-fractions in random healthy adults in Ouagadougou, Burkina Faso. PLoS One. 2015;10(1):e011642. doi: 10.1371/journal.pone.0116420. [ Links ]
24. Martin SS, Khokhar AA, May HT, Kulkarni KR, Blaha MJ, Joshi PH, et al. HDL cholesterol subclasses, myocardial infarction, and mortality in secondary prevention: the Lipoprotein Investigators Collaborative. Eur Heart J. 2015;36(1):22-30. doi: 10.1093/eurheartj/ehu264. [ Links ]
25. Quintanilla-Cantú A, Peña-de-la-Sancha P, Flores-Castillo C, Mejía-Domínguez AM, Posadas-Sánchez R, Pérez-Hernández N, et al. Small HDL subclasses become cholesterol-poor during postprandial period after a fat diet intake in subjects with high triglyceridemia increases. Clin Chim Acta. 2017;464:98-105. doi: 10.1016/j.cca.2016.11.018. [ Links ]
26. Jia L, Fu M, Tian Y, Xu Y, Gou L, Tian H, et al. Alterations of high-density lipoprotein subclasses in hypercholesterolemia and combined hyperlipi demia. Int J Cardiol. 2007;120(3):331-7. doi: 10.1016/j.ijcard.2006.10.007. [ Links ]
27. Generoso G, Bensenor IM, Santos RD, Santos IS, Goulart AC, Jones SR, et al. Association between high-density lipoprotein subfractions and low-grade inflammation, insulin resistance, and metabolic syndrome components: The ELSA-Brasil study. J Clin Lipidol. 2018;12(5):1290-1297. doi: 10.1016/j.jacl.2018.05.003. [ Links ]
28. Cartolano FDC, Dias GD, Freitas MCP de, Figueiredo Neto AM, Damasceno NRT. Insulin Resistance Predicts Atherogenic Lipoprotein Profile in Nondiabetic Subjects. J Diabetes Res. 2017;2017:1018796. doi: 10.1155/2017/1018796. [ Links ]
29. Jo N, Garmendia F, Pando R. Sub-clases de lipoproteínas de alta densidad en diabéticos. Rev méd peru. 1994;66(351):68-70. [ Links ]
30. Moriyama K, Takahashi E. HDL2/HDL3 ratio changes, metabolic syndrome markers, and other factors in a Japanese population. J Atheroscler Thromb. 2016;23(6):704-712. doi: 10.5551/jat.32896. [ Links ]
Sources of funding: This study was funded by the Consejo de Desarrollo Científico, Humanístico y Tecnológico CONDES (CC-0437-10-21-09-10) and by Fundacite-Zulia (FZ-0058- 2007).
Received: September 07, 2019; Accepted: July 01, 2020











 texto em
texto em