Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Medicina Experimental y Salud Publica
Print version ISSN 1726-4634
Rev. perú. med. exp. salud publica vol.38 no.1 Lima Jan-Mar 2021 Epub Feb 14, 2021
http://dx.doi.org/10.17843/rpmesp.2021.381.6182
Brief report
Microbiological and molecular characterization of antimicrobial resistance in uropathogenic Escherichia coli from peruvian public hospitals
1 Laboratorio de Investigación en Biología Molecular, EP Medicina Humana, Universidad Peruana Unión, Lima, Perú.
2 Laboratorio de Genómica Microbiana, Universidad Peruana Cayetano Heredia, Lima, Perú.
3 Laboratorio de Microbiología, Hospital Antonio Lorena, Cuzco, Perú.
4 Servicio de Microbiología, Laboratorio de Referencia Regional Salud Pública San Martín, Tarapoto, Perú.
5 Servicio de Microbiología, Laboratorio de Referencia Regional de Salud Pública Tumbes, Tumbes, Perú.
6 Servicio de Microbiología, Laboratorio de Referencia Regional Salud Pública, La Libertad, Trujillo, Perú.
7 Área de Microbiología, IPRESS Jorge Chávez, Madre de Dios, Perú.
8 Servicio de Microbiología, Hospital Regional de Loreto, Iquitos, Perú.
9 Área de Microbiología, Clínica Adventista Ana Stahl, Iquitos, Perú.
10 Servicio de Microbiología, Laboratorio de Referencia Regional de Salud Pública Huancavelica, Huancavelica, Perú.
11 Área de Microbiología, Clínica Americana Juliaca, Juliaca, Perú.
12 Laboratorio de Microbiología, Hospital Carlos Monge Medrano, Juliaca, Perú.
INTRODUCTION
Urinary tract infections (UTI) have a high incidence worldwide and cause high treatment costs for healthcare systems ( 1. Escherichia coli is the etiological agent most frequently found in UTIs and is mainly treated with antimicrobials. However, the lack of regulation of these treatments favored the emergence of multidrug-resistant (MDR) strains worldwide 2 ) and the emergence of extended-spectrum beta-lactamase (ESBL)-producing E. coli strains with the ability to hydrolyze penicillins, cephalosporins and monobactams. Genes encoding ESBL production are frequently found in plasmids and are usually accompanied by other genes for resistance to cephalosporins, sulfonamides, fluoroquinolones and aminoglycosides ( 3. There are several genes coding for ESBL, the most frequent being those of the TEM, SHV and CTX-M families 4 , 5. More than 400 types of these enzymes have been reported and CTX-M are the most frequent worldwide 6.
In Peru, the detection of antimicrobial resistance in bacteria causing UTI is not included in the epidemiological surveillance system and no updated data are available 7. Knowing the levels of resistance and genes associated with ESBL production in E. coli isolates of UTI will allow the establishment of effective empirical therapies and control programs. Therefore, the aim of this study was to characterize by phenotypic and molecular tests the antimicrobial resistance and prevalence of ESBL in E. coli isolates from patients with UTI from eight public hospitals in different departments of Peru.
KEY MESSAGES
Motivation for the study: It is important to update data on levels and patterns of antimicrobial resistance in uropathogenic Escherichia coli. Determining which are the resistance patterns allows guiding adequate therapeutics for this type of infections.
Main findings: High levels of resistance were detected for ampicillin, ciprofloxacin, trimethoprim/ sulfamethoxazole, cefepime and cefuroxime. We identified 55.7% of isolates as extended spectrum beta-lactamase (ESBL) producers with the presence of bla TEM, bla CTX-M and bla SHV genes.
Implications: The high frequency of multidrug-resistant ESBL-producing E. coli strains is alarming and should raise awareness about the appropriate use of antimicrobials in the treatment of urinary tract infections.
THE STUDY
A descriptive study was conducted, based on obtaining bacterial isolates from eight public hospitals located in the departments of Cusco, Huancavelica, La Libertad, Loreto, Madre de Dios, Puno, San Martín and Tumbes. A total of 70 E. coli isolates obtained from outpatients with clinical diagnosis compatible with UTI collected during 2018 were used.
The isolates were characterized at the Molecular Biology Research Laboratory of the Universidad Peruana Unión. Species confirmation and determination of resistance profiles was carried out using the MicroScan® automated system (AutoScan-4) and gram-negative panels (Dade MicroScan®) following the manufacturer’s instructions. Fifteen antimicrobials from different families were included: ampicillin (AMP), ampicillin with sulbactam (AMP/SUL), amoxicillin with clavulanic acid (AMC), piperacillin with tazobactam (PIP/ TZ), aztreonam (ATM), cefepime (FEP), cefuroxime (CFX), ceftazidime (CAZ), cefotaxime (FOX), tobramycin (TOB), gentamicin (GEN), ciprofloxacin (CIP), trimethoprim/sulfamethoxazole (SXT), colistin (COL) and tigecycline (TIG). In addition, we detected the presence of extended-spectrum beta-lactamase (ESBL)-producing E. coli. The results were interpreted according to Clinical and Laboratory Standards Institute (CLSI) recommendations ( 8.
DNA extraction was carried out with the innuPREP kit following the manufacturer’s instructions (Analytik Jena, Germany). For gene identification, we used a conventional polymerase chain reaction (PCR) designed for each gene bla CTX-M 9, bla TEM 10, bla SHV 11 and bla PER 12. The primer sequences used are detailed in Table 1.
Table 1 Primers used for gene amplification.
| Genes | Amplicon (bp) | Primer | Sequences | Reference |
|---|---|---|---|---|
| bla CTX-M | 544 | CTX/F | TTTGCGATGTGCAGTACCAGTAA | 9 |
| CTX/R | CGATATCGTTGGTGGTGCCAT | |||
| bla TEM | 504 | TEM/F | TTGGGTGCACGAGTGGGTTA | 10 |
| TEM/R | TAATTGTTGCCGGGAAGCTA | |||
| bla SHV | 865 | SHV/F | ATGCGTTATATTCGCCTGTG | 11 |
| SHV/R | GTTAGCGTTGCCAGTGCTCG | |||
| bla PER | 927 | PER/F | ATGAATGTCATCACAAAATG | 12 |
| PER/R | TCAATCCGGACTCACT |
Multidrug resistance was defined as the detection of a resistant phenotype for at least one antimicrobial in three or more classes. The proportion of resistant isolates was stratified according to patient sex. Bivariate analysis was developed using Fisher’s exact test with a 95% confidence level. Data was managed with the Stata 16 statistical package (StataCorp, College Station, Texas, USA).
The study was evaluated and approved by the Ethics Committee of the Universidad Peruana Unión (N2019-CEUPeU-0001) and by the Dirección Universitaria de Investigación, Ciencia y Tecnología of the Universidad Peruana Cayetano Heredia.
FINDINGS
Seventy Escherichia coli isolates were obtained from outpatients with diagnosis compatible with urinary tract infection (UTI) from public hospitals in Huancavelica (n=15), Loreto (n=14), Tumbes (n=13), Madre de Dios (n=12), La Libertad (n=8), Puno (n=4), Cusco (n=3) and San Martín (n=1). The mean age was 38.8 years and 80% (n=56) of the patients were female. Of the isolates, 65.7% (46/70) had a multidrug-resistant (MDR) phenotype, which was more frequent in male patients (78.6%, 11/14) compared to female patients (62.5%, 35/56). A total of 39/70 (55.7%) isolates were identified as extended-spectrum beta-lactamase (ESBL) producers, with a higher frequency in male patients (64.3%, 9/14) compared to female patients (53.6%, 30/56). However, these differences were not statistically significant (p>0.05). Of the isolates identified as ESBL producers, 92.3% (36/39) had an MDR phenotype including resistance to aminoglycosides, fluoroquinolones, beta-lactams and sulfonamides.
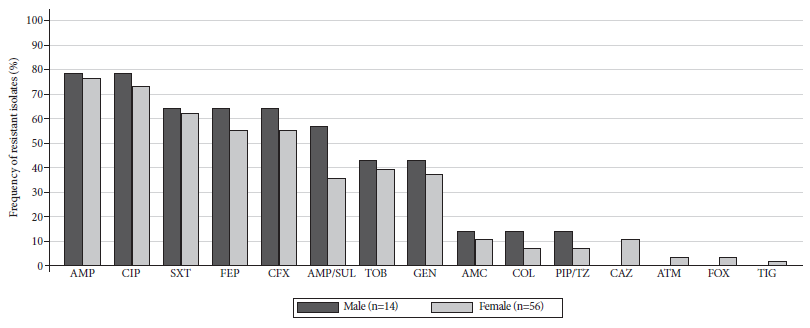
High percentages of resistance were detected against ampicillin (77.1%), ciprofloxacin (74.3%), trimethoprim/sulfamethoxazole (62.9%), cefepime (57.1%), cefuroxime (57.1%) and ampicillin with sulbactam (40%). Isolates from male patients had the highest levels of resistance (Figure 1). However, only isolates from female patients showed resistance to ceftazidime (10.7%, n=6), aztreonam (3.6%, n=2), cefotaxime (3.6%, n=2), tigecycline (1.8%, n=1). These differences were not statistically significant (p>0.05). No isolates resistant to amikacin, ertapenem, imipenem and meropenem were detected.
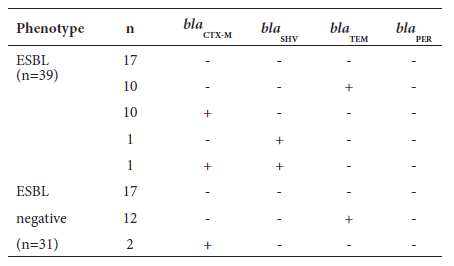
The bla TEM gene family was detected by PCR in 31.4% (22/70), followed by bla CTX-M (18.6%, n=13) and bla SHV (2.9%, n=2), in both ESBL-producing and non-ESBL-producing isolates. Of the total ESBL isolates, 56.4% (22/39) were positive for at least one of the genes evaluated. The bla CTX-M gene was the most common (28.2%, 11/39), and only one isolate presented it in combination with the bla SHV gene. The bla TEM gene was found in 25.6% (10/39) of the ESBL-producing isolates. There was no evidence of the joint presence of the bla CTX-M and bla TEM genes. Of the total non-ESBL-producing isolates, 54.8% (17/31) did not present any of the genes evaluated; 38% (12/31) had the bla TEM gene and only 6.5% (n=2) had the bla CTX-M gene. Of the total number of ESBL-producing and non-ESBL-producing isolates, we did not detect the presence of the bla PER gene (Table 2).
DISCUSSION
E. coli isolates from patients with UTI had high levels of resistance to clinically important antimicrobials. More than 50% of the isolates were classified as MDR and ESBL-producing. Isolates were mostly resistant to ampicillin, ciprofloxacin and trimethoprim/sulfamethoxazole, which are antimicrobials frequently used for the treatment of UTI 13. In addition, we found isolates resistant to colistin, a drug of last resort used in complicated UTI caused by MDR bacteria, 14. Isolates resistant to imipenem, meropenem, and ertapenem were not detected. However, the detection of ESBL-producing uropathogenic E. coli isolates represents a potential risk of resistance development, due to their ability to carry resistance genes to other antimicrobials 15.
Isolates from male patients showed higher levels of resistance to ampicillin, ciprofloxacin, trimethoprim/sulfamethoxazole, cefepime, cefuroxime, ampicillin with sulbactam, tobramycin, gentamicin, amoxicillin with clavulanic acid, colistin and piperacillin with tazobactam. The differences found according to the sex of the patients were not significant, so we cannot evidence that being a male patient would be an indicator for the empirical selection of antimicrobials for the treatment of UTIs. However, our results show a high prevalence of E. coli resistant to several commonly used antimicrobials in these infections. Greater care should be considered in the selection of therapeutic options by treating physicians to avoid selective pressure leading to the emergence of MDR strains.
The bla TEM gene family was the most frequent, followed by bla CTX-M and bla SHV. These results contrast with those found by other authors, where the bla CTX-M gene was found to be the most frequent in patients with UTI in Peru 16 - 18. A total of 17 ESBL-producing isolates were negative for all the genes evaluated. Even the presence of bla CTX-M (n=2) and bla TEM (n=12) genes was detected in isolates identified as non-ESBL producers. The differences observed in the detection of ESBL isolates by phenotypic and genotypic methods reflect the low sensitivity of the phenotypic method and the possible influence of external factors in the occurrence of resistance. Possibly, many isolates did not produce ESBL at levels detectable by the phenotypic method, which could explain the presence of ESBL-negative isolates, but with genes related to the production of these enzymes. In contrast to the phenotypic method, gene detection by PCR amplification has better levels of specificity and sensitivity. However, these values are closely correlated to the quality and design of primers. Even non-ESBL variants of bla TEM or bla SHV genes have been described, so sequencing methods are essential for their identification and characterization 19.
In conclusion, the results show high levels of resistance in E. coli isolates carrying bla TEM, bla CTX-M and bla SHV genes recovered from outpatients diagnosed with UTI in different regions of Peru. Peruvian public hospitals conduct antimicrobial resistance monitoring using mainly phenotypic methods and to a lesser extent, molecular methods. However, these methodologies may not correctly reflect the status of antimicrobial resistance in UTIs and other types of infections. Therefore, the implementation of cutting-edge methods for genomic surveillance of antimicrobial resistance in hospitals is necessary.
The results obtained correspond to a first phase of the study. We will use whole genome sequencing methods and bioinformatic analysis for the study of antimicrobial resistance in these bacterial isolates. The information generated will serve as an epidemiological tool to determine the distribution of resistance genes and also as a guide to evaluate the trend and possible changes in therapeutic schemes by treating physicians.
Acknowledgments:
To the staff of the School of Human Medicine of the Universidad Peruana Union (Salomon Huancahuire and Miguel Otiniano), the staff of the Microbial Genomics Laboratory of the Universidad Peruana Cayetano Heredia (Brenda Ayzanoa, Janet Huancachoque and Camila Castillo) and Marco Galarza of the Biotechnology and Molecular Biology Laboratory of the National Institute of Health for their support in the collection of isolates.
REFERENCES
.Stamm WE, Norrby SR. Urinary tract infections: disease panorama and challenges. J Infect Dis. 2001;183 Suppl 1: S1-4. doi:10.1086/318850. [ Links ]
. Pitout JD. Extraintestinal Pathogenic Escherichia coli: A Combination of Virulence with Antibiotic Resistance. Front Microbiol. 2012;3:9. doi: 10.3389/fmicb.2012.00009. [ Links ]
. Lee SY, Kotapati S, Kuti JL, Nightingale CH, Nicolau DP. Impact of extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella species on clinical outcomes and hospital costs: a matched cohort study. Infect Control Hosp Epidemiol. 2006;27(11):1226-32. doi: 10.1086/507962. [ Links ]
. D'Andrea MM, Arena F, Pallecchi L, Rossolini GM. CTX-M-type ß-lactamases: a successful story of antibiotic resistance. Int J Med Microbiol. 2013;303(6-7):305-17. doi: 10.1016/j.ijmm.2013.02.008. [ Links ]
. Pitout JD, Hossain A, Hanson ND. Phenotypic and molecular detection of CTX-M-beta-lactamases produced by Escherichia coli and Klebsiella spp. J Clin Microbiol. 2004;42(12):5715-21. doi: 10.1128/JCM.42.12.5715-5721.2004. [ Links ]
. Woerther PL, Burdet C, Chachaty E, Andremont A. Trends in human fecal carriage of extended-spectrum ß-lactamases in the community: toward the globalization of CTX-M. Clin Microbiol Rev. 2013;26(4):744-58. doi: 10.1128/CMR.00023-13. [ Links ]
. Astete S, Madrid L, Fukuda F, Buckley A, Meritens D, Menchola JV. Sensibilidad antibiótica de los gérmenes causantes de infecciones urinarias en pacientes ambulatorios en el Hospital Nacional Arzobispo Loayza. Rev Soc Per Med Inter. 2004;17(1): 5-8. [ Links ]
. Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing [Internet]. 30th ed; 2020 [citado el 12 de febrero de 2020]; Disponible en: https://clsi.org/standards/products/microbiology/documents/m100/. [ Links ]
. Edelstein M, Pimkin M, Palagin I, Edelstein I, Stratchounski L. Prevalence and molecular epidemiology of CTX-M extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae in Russian hospitals. Antimicrob Agents Chemother. 2003;47(12):3724-32. doi: 10.1128/aac.47.12.3724-3732.2003. [ Links ]
. Arlet G, Philippon A. Construction by polymerase chain reaction and intragenic DNA probes for three main types of transferable Î2-lactamases (TEM, SHV, CARB). FEMS Microbiol Lett. 1991;68(1):125. doi:10.1111/j.1574-6968.1991.tb04833.x. [ Links ]
. Essack SY, Hall LM, Pillay DG, McFadyen ML, Livermore DM. Complexity and diversity of Klebsiella pneumoniae strains with extended-spectrum beta-lactamases isolated in 1994 and 1996 at a teaching hospital in Durban, South Africa. Antimicrob Agents Chemother. 2001;45(1):88-95. doi: 10.1128/AAC.45.1.88-95.2001. [ Links ]
. Kiratisin P, Apisarnthanarak A, Laesripa C, Saifon P. Molecular characterization and epidemiology of extended-spectrum-beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae isolates causing health care-associated infection in Thailand, where the CTX-M family is endemic. Antimicrob Agents Chemother. 2008;52(8):2818-24. doi: 10.1128/AAC.00171-08. [ Links ]
. Huang ES, Stafford RS. National patterns in the treatment of urinary tract infections in women by ambulatory care physicians. Arch Intern Med. 2002;162(1):41-7. doi: 10.1001/archinte.162.1.41. [ Links ]
. Cui P, Niu H, Shi W, Zhang S, Zhang H, Margolick J, et al. Disruption of Membrane by Colistin Kills Uropathogenic Escherichia coli Persisters and Enhances Killing of Other Antibiotics. Antimicrob Agents Chemother. 2016;60(11):6867-6871. doi: 10.1128/AAC.01481-16. [ Links ]
. Carattoli A. Plasmids in Gram negatives: molecular typing of resistance plasmids. Int J Med Microbiol. 2011;301(8):654-8. doi: 10.1016/j.ijmm.2011.09.003. [ Links ]
. Galván F, Agapito J, Bravo N, Lagos J, Tamariz J. Caracterización fenotípica y molecular de Escherichia coli productoras de ß-Lactamasas de espectro extendido en pacientes ambulatorios de Lima, Perú. Rev Medica Hered. 2016;27:22. doi:10.20453/rmh.v27i1.2780. [ Links ]
. Salles MJ, Zurita J, Mejía C, Villegas MV; Latin America Working Group on Bacterial Resistance. Resistant gram-negative infections in the outpatient setting in Latin America. Epidemiol Infect. 2013;141(12):2459-72. doi: 10.1017/S095026881300191X. [ Links ]
. Miranda J, Pinto J, Faustino M, Sánchez-Jacinto B, Ramirez F. Antimicrobial resistance of uropathogens in older adults in a private clinic in Lima, Peru. Rev Peru Med Exp Salud Publica. 2019;36(1):87-92. doi: 10.17843/rpmesp.2019.361.3765. [ Links ]
. Pitout JD, Laupland KB. Extended-spectrum beta-lactamase-producing Enterobacteriaceae: an emerging public-health concern. Lancet Infect Dis. 2008;8(3):159-66. doi: 10.1016/S1473-3099(08)70041-0. [ Links ]
Funding: The work was possible thanks to the support provided by the Professional School of Human Medicine, Faculty of Health Sciences, Universidad Peruana Unión (Resolution No 0935-2018-UPEU-FCS-CF), Lima-Peru.
Cite as: Marcos-Carbajal P, Salvatierra G, Yareta J, Pino J, Vásquez N, Diaz P, et al. Microbiological and molecular characterization of antimicrobial resistance in uropathogenic escherichia coli from peruvian public hospitals. Rev Peru Med Exp Salud Publica. 2021;38(1):119-23. doi: https://doi.org/10.17843/rpmesp.2021.381.6182.
Received: July 19, 2020; Accepted: October 28, 2020











 text in
text in