Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Medicina Experimental y Salud Publica
versión impresa ISSN 1726-4634
Rev. perú. med. exp. salud publica vol.38 no.4 Lima oct./dic 2021 Epub 21-Dic-2021
http://dx.doi.org/10.17843/rpmesp.2021.384.9288
Original articles
Association between the need for palliative care and chronic diseases in patients treated in a peruvian hospital
1 Grupo de Investigación Neurociencia, Efectividad y Salud Pública, Universidad Científica del Sur, Lima, Perú.
2 Sociedad Científica de San Fernando, Universidad Nacional Mayor de San Marcos, Lima, Perú.
3 Red de Eficacia Clínica y Sanitaria, REDECS, Lima, Perú.
4 Escuela de Medicina, Universidad Peruana de Ciencias Aplicadas, Lima, Perú.
5 Servicio de Anestesiología Cardiovascular, Instituto Nacional Cardiovascular INCOR- EsSalud, Lima, Perú.
Objectives.
To assess the association between chronic disease (CD) and the need for palliative care (NPC).
Materials and methods.
An analytical cross-sectional study was carried out in a Peruvian hospital during 2019. Patients hospitalized with CD were included, and pregnant women and those hospitalized in critical units were excluded. The SPICT-ESTM instrument was used to assess the NPC; sociodemographic and clinical characteristics were also evaluated. The strength of association was calculated with Poisson regressions with robust variance to estimate crude prevalence ratios (PR) and adjusted prevalence ratios (aPR) by confounders.
Results.
A total of 172 patients were evaluated, the mean age was 61 years, where 54.7% were male and 123 patients had NPC. In the crude model, we found an association with having cerebrovascular disease (PR: 1.23; p=0.028), any type of cancer (PR: 1.38; p<0.001), heart disease (PR: 1.29; p=0.007), nephropathy (PR: 1.42, p<0.001) and Alzheimer’s disease (PR: 1.42; p<0.001). The association was maintained for most of the evaluated CDs in the adjusted model, except for heart disease (aPR: 1.11; p=0.320). The association strength was lower for diabetes mellitus (PR: 0.78; p=0.044).
Conclusion.
NPC in hospitalized chronically ill patients is high and more frequent in patients with cancer, cerebrovascular disease, renal problems and Alzheimer’s disease. Care programs for patients with diabetes mellitus may decrease NPC.
Keywords: Palliative care; Chronic Disease; Noncommunicable Diseases; Hospitalization; Peru; Neoplasm; Kidney Diseases; Cerebrovascular Disorders; Alzheimer Disease; Diabetes Mellitus
INTRODUCTION
The World Health Organization (WHO) defines palliative care as a “health strategy that improves the quality of life of patients and their families, aimed at life-threatening health problems” 1. However, the importance of implementing palliative care (PC) early and not only in the face of terminal diagnoses is becoming increasingly evident 2 , 3. In patients with chronic diseases (CD) PC improves quality of life; however, late initiation increases health care costs 3 , 4. Therefore, timely mechanisms should be put in place to identify patients in need of this care 5.
The lack of organizational-level national programs, insufficient training of health professionals and inaccessibility to timely service 6 , 7, are challenges that must be overcome. Due to the low development of PC and its insufficient offer in Peru 8, Law 30846 came into effect at the end of 2018, which allowed the creation of the National Palliative Care Plan for Oncologic and Non-Oncologic Diseases expanding these services to patients with other types of conditions other than cancer 9.
The need for palliative care (NPC) is defined as all those health services that seek to alleviate physical and psychological suffering and prevent disease progression 10. Various instruments can be used to measure NPC, such as NECPAL (NECesidades PALiativas), RADPAC (RADboud indicators for PAlliative Care Needs), PALLI (PALLIativey care need) and SPICT (Supportive and Palliative Care Indicators Tool); the latter being one of the most widely used because it is mainly aimed at identifying people who are at risk of functional deterioration or death and who can benefit from PC 5.
Previous studies have identified the NPC in patients with CD. In those with renal failure, the NPC reaches up to 16% 11, while in patients with stage III and IV heart failure, the NPC is as high as 55% 12. In addition, previously reported risk factors for patients with CD in order to require PC include gender, age and family support 13; however, other characteristics such as the number of comorbidities and hospitalizations determine a negative prognosis for such patients 14. Thus, patients with CD are often hospitalized for decompensation and/or disease progression, which is an ideal time for health care providers to assess the NPC 15. Therefore, the aim of this study was to evaluate the association between chronic diseases and the need for palliative care in hospitalized patients in a Peruvian public hospital.
KEY MESSAGES
Motivation for the study: Palliative care improves the quality of life of patients and their families. It is common to assess palliative care in cancer patients, but not in patients with other chronic diseases.
Main findings: The need for palliative care is frequent in patients with chronic diseases hospitalized for any cause; especially in patients with cancer, cerebrovascular disease, renal problems and Alzheimer’s disease.
Implications: Hospitalized chronically ill patients should have an assessment of the need for palliative care prior to discharge. The creation of palliative medicine units in more hospitals in the country is recommended.
MATERIALS AND METHODS
An analytical cross-sectional study was carried out at the Daniel Alcides Carrión National Hospital located in the constitutional province of Callao in Peru. This hospital is the most highly complex in the entire reference area.
The selection criteria were the following: patients over 18 years of age with a diagnosis of a chronic disease who were hospitalized for any cause at the time of data collection, and who gave their consent to participate, either by themselves or by the responsible family member. Pregnant women, patients hospitalized in critical units such as intermediate care units (INCU), intensive care units (ICU) and shock trauma were excluded.
The research team inspected all inpatient beds of the services of Internal Medicine, Clinical Specialty Medicine, General Surgery and Surgical Specialties during the last week of May and first week of June 2019. Some provided data were verified with medical records, as well as information provided by attending physicians. Since all patients hospitalized during the time of data collection were included, sample size was not calculated. The statistical power was 99.9%, based on the NPC in patients with and without diabetes (69.2% and 24%, respectively); Epidat v.4.1 was used for the calculation.
The NPC was measured with the Spanish version of the SPICT (Supportive and Palliative Care Indicators Tool) 16, which is free to download and use. The SPICT-ESTM (SPICT - Spanish version) is a questionnaire containing 27 items with dichotomous responses, with good equivalence, reliability and stability in the Spanish version compared to the original version, and it also has a sensitivity of 70% and a specificity of 87% 17. The items are divided into seven general health indicators (unplanned hospital admission, irreversible functional limitation, dependence on the care of others, need for more than one caregiver, significant weight loss or malnutrition, persistent symptoms despite adequate treatment, and the desire to reduce treatments and focus on quality of life) and 20 clinical indicators of advanced disease (for example: progressive functional and cognitive impairment, dyspnea or chest pain at rest, frequent falls, respiratory failure, need for transplantation, or others). The NPC was established with at least two indicators of general health deterioration associated with an indicator of advanced disease.
A chronic or non-communicable disease was considered to be all conditions that tend to be long-term and can be controlled but not cured. Those included in our study were (all dichotomous variables): diabetes mellitus, any type of cancer, any type of dementia (not including Alzheimer’s disease), Alzheimer’s disease, lung disease, liver disease, heart disease, nephropathy, and cerebrovascular disease; for the latter three, only those not caused by diabetes mellitus were considered. In the case that the patient had more than one chronic disease, for the purposes of the study we considered the main chronic disease to be the one with the longest duration and the others were considered as comorbidities. Chronic diseases were defined as a clinical diagnosis made by a specialist and reported in the clinical history.
Other variables relevant to the study were sociodemographic characteristics (age, sex, religion, number of children, among others); clinical characteristics (hospitalization service, number of hospitalizations in the last year; number of comorbidities and previous hospital-acquired infections) and some intermediate variables between the patient’s chronic disease and NPC called frailty characteristics (all with final values: present/absent), such as: difficulty in expressing oneself (the interviewer needs to repeat questions to clarify the patient’s answers or the patient has a disease that limits his or her ability to speak); urinary and/or fecal incontinence (inability to control urination and/or bowel movements); difficulty eating (need for help from a third person to put food in the mouth or the patient is edentulous); decreased food intake (does not swallow the entire calculated caloric requirement), and persistent symptoms despite treatment (presence of any of the symptoms with which he/she was admitted to hospital).
The information was recorded in a Microsoft Excel data collection spreadsheet. The double entry technique was used to control the data. Statistical analysis was carried out in the Stata v.15.0 program using measures of central tendency (mean) and dispersion (standard deviation) for numerical variables, while absolute and relative frequencies were used for categorical variables. The analysis between categorical and numerical variables was carried out with the Mann-Whitney U test, while the chi-square test or Fisher’s exact test were used for the comparison of proportions between categorical variables, depending on the magnitude of the expected values.
The strength of association between the chronic diseases and the need for palliative care was evaluated using Poisson-type generalized linear models with robust variance to calculate crude (PR) and adjusted prevalence ratios (aPR). For the latter, we included theoretical confounding variables (age, sex, and history of previous hospitalizations) described in the reviewed literature 19 - 21.
The research was approved by the Institutional Research Ethics Committee (CIEI) of the Hospital Nacional Daniel Alcides Carrión, with official letter 4193-2019/HN.DAC-C-DG/OADI. All patients were asked for their voluntary consent to participate in the study; if a patient had any difficulty in expressing their will, consent was given by a responsible family member. In addition, it was clearly stated that current or future care would not be influenced by their decision. To ensure patient confidentiality, the affiliation data were included in a coded database that was accessible only to the main researchers.
RESULTS
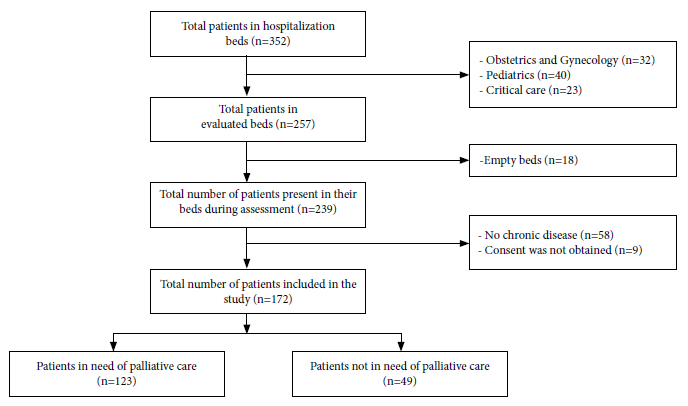
We evaluated a total of 352 hospital beds and 172 patients were included (Figure 1), the mean age was 61 years (SD ± 17.3). More than half of the participants were male (n=94) and had a current partner (n=96), while the vast majority had at least one child (79.1%), some reported a religious belief (96.7%) and only a small group had more than one comorbidity (7.0%). The NPC was associated with age (p=0.035) and history of hospitalizations in the last year (p=0.002) (Table 1).
Table 1 Sociodemographic and clinical characteristics of chronically ill patients hospitalized for any cause in a Peruvian hospital according to their need for palliative care (n=172).
| Characteristics | Total of patients N (%) | Need for palliative care | p-value | |
|---|---|---|---|---|
| Yes (n=125) | No (n=49) | |||
| Sociodemographic characteristics | ||||
| Sex | ||||
| Female | 78 (45.4) | 57 (73.1) | 21 (26.9) | 0.679 |
| Male | 94 (54.7) | 66 (70.2) | 28 (29.8) | |
| Age | ||||
| Years, mean (SD) | 61 (17.3) | 62.8 (17.0) | 56.4 (17.3) | 0.035 a |
| Up to 65 years | 100 ((58.1) | 66 (66.0) | 34 (34.0) | 0.059 |
| Older than 65 years | 72 (41.9) | 57 (79.2) | 15 (20.8) | |
| Marital status | ||||
| No current partner | 76 (44.2) | 58 (76.3) | 18 (23.7) | 0.214 |
| With current partner | 96 (55.8) | 65 (67.7) | 31 (32.3) | |
| Number of children | ||||
| None | 36 (20.9) | 25 (69.4) | 11 (30.6) | 0.757 |
| At least one | 136 (79.1) | 98 (72.1) | 38 (27.9) | |
| Religious belief | ||||
| Atheist | 7 (4.1) | 5 (71.4) | 2 (28.6) | 1.000 b |
| Christian | 159 (92.4) | 114 (71.7) | 45 (28.3) | |
| Other | 6 (3.5) | 4 (66.7) | 4 (33.3) | |
| Clinical characteristics | ||||
| Number of comorbidities | ||||
| Up to one | 160 (93.0) | 115 (71.9) | 45 (28.1) | 0.743 b |
| More than one | 12 (7.0) | 8 (66.7) | 4 (33.3) | |
| Hospitalizations in the last year | ||||
| Up to one | 118 (68.6) | 76 (64.4) | 42 (35.6) | 0.002 |
| More than one | 54 (31.4) | 47 (87.0) | 7 (13.0) | |
| Previous hospital-acquired infection | ||||
| No | 155 (90.1) | 108 (69.7) | 47 (30.3) | 0.157 |
| Yes | 17 (9.9 | 15 (88.2) | 2 (11.8) | |
| Hospital service | ||||
| Internal medicine | 105 (61.1) | 79 (75.2) | 26 (24.8) | 0.395 |
| Surgery | 43 (25.0) | 28 (65.1) | 15 (34.9) | |
| Clinical specialties | 24 (13.9) | 16 (66.7) | 8 (33.3) | |
| Cause for hospitalization | ||||
| Infection | 48 (27.9) | 32 (66.7) | 16 (33.3) | 0.067 |
| Disease decompensation | 73 (42.5) | 57 (78.1) | 16 (21.9) | |
| Evaluation or beginning of treatment | 31 (18.0) | 24 (77.4) | 7 (22.6) | |
| Added disease | 20 (11.6) | 10 (50.0) | 10 (50.0) | |
SD: standard deviation.
a The Mann Whitney U test was used to calculate the p-value.
b Fisher’s exact test was used to calculate the p-value, unlike other evaluations where the p-value was estimated with the chi-square test.
Of a total of 172 chronically ill patients hospitalized for any cause, 123 were in need of palliative care (71.5%). The most frequent major criterion of the SPICT-ESTM tool was unplanned hospital admission (99.2%), followed by dependence on the care of others (74.0%). Regarding the specific frailty characteristics covered by the instrument, we identified the following as the most frequent: patients with persistent symptoms despite treatment (n=111), decreased food intake (n=102), difficulty eating (n=65), urinary and/or fecal incontinence (n=36) and some patients with difficulty speaking or expressing themselves (n=39).
The most frequent chronic diseases found were cerebrovascular disease (n=67) and diabetes mellitus (n=67), the NPC in these was 80.5% and 69.2%, respectively. All hospitalized patients with Alzheimer’s disease or nephropathy had the NPC (Figure 2).
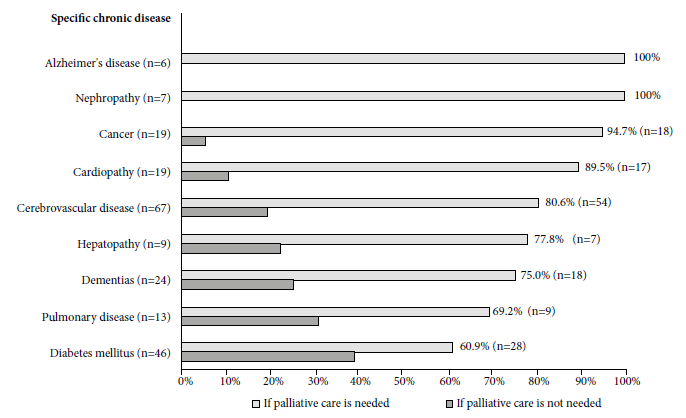
Figure 2 Distribution of the need for palliative care according to specific chronic disease in patiens hospitalized for any cause in a Peruvian hospital between May and June 2019 (N=172).
In the crude model, the NPC showed significant association in patients with cerebrovascular disease (PR: 1.23; p=0.028), patients with any type of cancer (PR: 1.38, p<0.001), heart disease (PR: 1.29; p=0.007), nephropathy (PR: 1.42; p<0.001) and Alzheimer’s disease (PR: 1.09; p<0.001). Whereas in the adjusted model, the probability of NPC was 21%, 39%, 43%, 43%, 28% higher in those with cerebrovascular disease (aPR: 1.21, p=0.038), cancer (aPR: 1.39, p<0.001), nephropathy (aPR: 1.43, p<0.001), Alzheimer’s disease (aPR: 1.28, p=0.008), respectively; compared to those without such conditions, adjusted for age, sex and history of more than one previous hospitalization; furthermore, we observed that patients with diabetes mellitus were 22% less likely to have the NPC compared to non-diabetic patients (RP: 0.78; p=0.044) (Table 2).
Table 2 Regression model to estimate the strength of association between chronic diseases and the need for palliative care in a hospital in Peru (n=172).
| Chronic disease a | Crude model | Adjusted model | ||||
|---|---|---|---|---|---|---|
| RP | 95% CI | p-value b | aRP | 95% CI | p-value b | |
| Cerebrovascular disease | 1.23 | 1.02 - 1.47 | 0.028 | 1.21 | 1.01 - 1.44 | 0.038 |
| Diabetes mellitus | 0.81 | 0.63 - 1.04 | 0.097 | 0.78 | 0.61 - 0.99 | 0.044 |
| Cancer | 1.38 | 1.19 - 1.61 | <0.001 | 1.39 | 1.20 - 1.62 | <0.001 |
| Dementias | 1.06 | 0.82 - 1.36 | 0.668 | 1.01 | 0.80 - 1.27 | 0.944 |
| Cardiopathies | 1.29 | 1.07 - 1.56 | 0.007 | 1.11 | 0.90 - 1.38 | 0.320 |
| Pulmonary disease | 0.97 | 0.66 - 1.41 | 0.855 | 0.90 | 0.64 - 1.27 | 0.564 |
| Nephropathy | 1.42 | 1.29 - 1.57 | <0.001 | 1.43 | 1.25 - 1.64 | <0.001 |
| Alzheimer’s disease | 1.42 | 1.28 - 1.57 | <0.001 | 1.28 | 1.06 - 1.53 | 0.008 |
| Hepatopathy | 1.09 | 0.76 - 1.57 | 0.632 | 1.01 | 0.70 - 1.47 | 0.934 |
PR: crude prevalence ratio, aPR: prevalence ratio adjusted for confounders (age, sex and history of more than one previous hospitalization), 95% CI: 95% confidence interval.
a The need for palliative care for patients with any of these diseases was established using the SPICT-ES questionnaire.
b The p-value was calculated using a Poisson-type generalized linear model with robust variance
DISCUSSION
In this study, chronic diseases such as cancer, diabetes, cerebrovascular disease, kidney problems and Alzheimer’s disease were associated with the NPC.
Of patients hospitalized for any cause with some type of chronic disease, 71.5% required palliative care; this is a higher proportion than previously reported by studies such as the one by Hamano et al. 21 ) where they found that the NPC in ambulatory patients in 17 primary care centers was 17.3%; Piers et al. reported 59.3% of NPC in geriatric patients in cardiology units 22 and Lunardi et al. reported 16% of NPC in patients with renal failure 11. SPICT was used in all these studies; and with another instrument such as the NECPAL the NPC reached 55% in patients with stage III and IV heart failure 12. The lower frequencies reported by other authors could be explained by the different health systems; in other regions patients do not enter hospitalization with great functional deterioration as can be seen in Peru. In addition, several of those studies were conducted on primary care, so it is expected that the patient is in better condition, unlike our study which was carried out in a general referral hospital that covers an entire province of the country.
PC is considered a therapeutic option for oncological patients 4 or in those with diseases that cause severe cognitive impairment 23. However, patients with chronic diseases can also have the NPC, which often goes unnoticed. Our study identified that patients with a history of cerebrovascular disease, renal disease, and Alzheimer’s disease have a higher probability of having the NPC compared with those without these conditions; moreover, this trend was statistically associated after adjusting for confounding variables. These findings coincide with those reported by other authors 24 - 26, where chronic diseases (other than cancer) deteriorate the functional capacity of the patient, making them subject to PC. In the case of patients with diabetes mellitus the probability of having the NPC was 22% lower compared to those without this disease (PR: 0.78; p=0.044), this could be due to the fact that all noncommunicable disease control programs of the Peruvian Ministry of Health include this disease, resulting in earlier tertiary prevention.
Some variables associated with the NPC were age and having more than one hospitalization in the last year. The deterioration of functional capacity as age increases may explain these associations 18 , 20, although the speed of progression varies according to the patient’s lifestyle and the family support received. No association was found between the NPC and having more than one comorbidity, this can be explained by the small number of patients with this characteristic (n=12) and the fact that multiple comorbidities are more frequent in the older adult population; in our study 58.1% of the patients were younger than 65 years of age.
The NPC is a set of conditions that increase the probability of decompensation and the need for medical care, among them are some frailty characteristics that were reported in this study. The persistence of symptoms despite treatment was the most frequent (n=111), 71.5% of these patients presented the NPC, which is similar to findings by other authors 27. We believe that this finding is important because unlike urinary incontinence, poor appetite or walking difficulty, these are not characteristics commonly associated in clinical practice with the NPC; cohort studies should assess whether this variable is a prognostic factor for adverse outcomes.
Our study has some limitations such as: 1) since it has a cross-sectional design, it is based on a single measurement and important outcomes such as length of hospital stay, mortality or quality of life at discharge could not be assessed; however, we believe that our results are a fundamental contribution for future research in this field of study. 2) Other important factors such as socioeconomic status, the degree of healthcare received or nutritional status were not evaluated; these factors are important for health assessment. 3) The NPC was not assessed with other instruments, as has been reported by other studies 24 , 28, in this regard, most instruments focus on identifying the NPC in patients with irreversible functional deterioration or with prognosis of death 6 and do not consider individuals with chronic diseases that could improve their quality of life with the implementation of palliative care ( 29 , 30. The SPICT-ES instrument was chosen because it is the most suitable for patients with chronic disease and its main strength is that it has an official version validated in Spanish. 4) Patient enrollment for the study was during the winter season, which may have overrepresented chronic pathologies, such as cerebrovascular disease and diabetes mellitus which are complicated by respiratory diseases that are more frequent at low temperatures. 5) We did not find studies that reported the frequency of the NPC in patients with the evaluated chronic diseases, therefore sample size was not calculate; however, the statistical power obtained based on the most prevalent chronic disease (diabetes) confirms that type 2 error was less than 20%.
In conclusion, the frequency of the NPC in hospitalized patients with chronic diseases is high and is associated with cancer, cerebrovascular disease, renal problems and Alzheimer’s disease. Healthcare strategies in patients with diabetes mellitus may decrease this need. Since hospitalization is an ideal period for a complete patient evaluation, we recommend screening before discharge and referral to specialized services, as well as the creation of palliative medicine units in more hospitals in the country.
We recommended that future research should include patients from various healthcare levels, especially primary care centers. In addition, patients should be actively followed and important outcomes such as frailty, quality of life and mortality should be assessed. From the clinical point of view, it is important that treating physicians assess the NPC not only in terminally ill patients but also in patients with chronic diseases, where the appropriate implementation of PC could improve their quality of life.
REFERENCES
1. Organización Mundial de la Salud [Internet]. Cuidados Paliativos. OMS; 2020. [citado el 22 de Setiembre del 2020]. Disponible en: https://www.who.int/es/news-room/fact-sheets/detail/palliative-care. [ Links ]
2. Organizacion Panamericana de la Salud. Mejora de los cuidados crónicos a través de las redes integradas de servicios de salud [Internet]. Washington: OPS; 2012 [citado el 22 de setiembre del 2020]. Disponible en: https://iris.paho.org/bitstream/handle/10665.2/3186/PAHO-Factsheet-Chronic-care-2012-es.pdf?sequence=1&isAllowed=y. [ Links ]
3. Dalgaard KM, Bergenholtz H, Espenhain Nielsen ME, Timm H. Early integration of palliative care in hospitals: A systematic review on methods, barriers, and outcome. Palliat SupportCare, 2014; 12: 495-513. doi: 10.1017/s1478951513001338. [ Links ]
4. Gómez-Batiste X, Murray S, Thomas K, Blay C, Boyd K, Moine S, et al. Comprehensive and Integrated Palliative Care for People With Advanced Chronic Conditions: An Update From Several European Initiatives and Recommendations for Policy. J Pain Symptom Manage. 2017; 53(3). doi: 10.1016/j.jpainsymman.2016.10.361. [ Links ]
5. ElMokhallalati Y, Bradley SH, Chapman E, Ziegler L, Murtagh F, Johnson M, et al. Identification of patients with potential palliative care needs: A systematic review of screening tools in primary care. Palliat Med. 2020; 34 (8): 989-1005. doi: 10.1177/0269216320929552. [ Links ]
6. Hawley P. Barriers to Access to Palliative Care. Palliat Care. 2017; doi: 10:1178224216688887. [ Links ]
7. Abu-Odah H, Molassiotis A, Liu J. Challenges on the provision of palliative care for patients with cancer in low- and middle-income countries: a systematic review of reviews. BMC Palliat Care. 2020;19(1):55. doi: 10.1186/s12904-020-00558-5. [ Links ]
8. Runzer-Colmenares F, Parodi J, Perez-Agüero C, Echegaray K, Samamé JC. Las personas con enfermedad terminal y la necesidad de cuidados paliativos: una deuda pendiente de los servicios de salud. Acta Med Peru. 2019; 36(2):134-44. [ Links ]
9. Ley que crea el plan nacional de cuidados paliativos para enfermedades oncológicas y no oncológicas, Ley No. 30846 [Internet]. Diario El Peruano. 24 agosto 2018. Disponible en: https://busquedas.elperuano.pe/download/url/ley-que-crea-el-plan-nacional-de-cuidados-paliativos-para-en-ley-n-30846-1693156-1. [ Links ]
10. Chan KS. Palliative care: the need of the modern era. Hong Kong Med J. 2018;24(4):391-399. doi: 10.12809/hkmj187310. [ Links ]
11. Lunardi L, Hill K, Crail S, Esterman A, Leu RL, Drummond C. 'Supportive and Palliative Care Indicators Tool (SPICT) improves renal nurses' confidence in recognising patients approaching end of life'. BMJ Support Palliat Care. 2020: bmjspcare-2020-002496. doi: 10.1136/bmjspcare-2020-002496. [ Links ]
12. Orzechowski R, Galvão AL, Nunes TDS, Campos LS. Palliative care need in patients with advanced heart failure hospitalized in a tertiary hospital. Rev Esc Enferm USP. 2019;53:e03413. doi: 10.1590/S1980-220X2018015403413. [ Links ]
13. Washington KT, Pike KC, Demiris G, Parker Oliver D, Albright DL, Lewis AM. Gender Differences in Caregiving at End of Life: Implications for Hospice Teams. J Palliat Med. 2015; 18(12):1048-1053. doi: 10.1089/jpm.2015.0214. [ Links ]
14. Legler A, Bradley EH, Carlson MD. The effect of comorbidity burden on health care utilization for patients with cancer using hospice. J Palliat Med. 2011;14(6):751-756. doi: 10.1089/jpm.2010.0504. [ Links ]
15. May P, Garrido MM, Cassel JB, Kelley AS, Meier DE, Normand C, et al. Palliative Care Teams' Cost-Saving Effect Is Larger For Cancer Patients With Higher Numbers Of Comorbidities. Health Aff (Millwood). 2016; 35(1):44-53. doi: 10.1377/hlthaff.2015.0752. [ Links ]
16. Highet G, Crawford D, Murray S, Boyd K. Development and evaluation of the Supportive and Palliative Care Indicators Tool (SPICT): a mixed-methods study. BMJ Support Palliat Care. 2014; 4(3): 285-90. doi: 10.1136/bmjspcare-2013-000488. [ Links ]
17. Alonso-Fachado A, Sansó-Martínez N, Martín-Roselló M, Ventosa-Rial J, Benito-Oliver E, Gómez-García R, et al. Spanish adaptation and validation of the supportive & palliative care indicators tool - SPICT-ESTM. Rev Saude Publica. 2018; 52:3. doi: 10.11606/s1518-8787.2018052000398. [ Links ]
18. Prasad S, Sung B, Aggarwal B. Las enfermedades crónicas asociadas a la edad requieren una medicina antigua: papel de la inflamación crónica. Prev Med. 2012; 54 Suppl (Suppl): S29-S37. doi: 10.1016/j.ypmed.2011.11.011. [ Links ]
19. Gubbels M. Sex, the aging immune system, and chronic disease. Cellular Immunology. 2015; 294 (2): 102-110. doi: 10.1016/j.cellimm.2015.02.002. [ Links ]
20. Rosland AM, Heisler M, Piette JD. The impact of family behaviors and communication patterns on chronic illness outcomes: a systematic review. J Behav Med. 2012;35(2):221-239. doi: 10.1007/s10865-011-9354-4. [ Links ]
21. Hamano J, Oishi A, Kizawa Y. Prevalence and Characteristics of Patients Being at Risk of Deteriorating and Dying in Primary Care. J Pain Symptom Manage. 2019;57(2):266-272.e1. doi: 10.1016/j.jpainsymman.2018.11.006. [ Links ]
22. Piers R, De Brauwer I, Baeyens H, Velghe A, Hens L, Deschepper E, et al. Supportive and Palliative Care Indicators Tool prognostic value in older hospitalised patients: a prospective multicentre study. BMJ Support Palliat Care. 2021:bmjspcare-2021-003042. doi: 10.1136/bmjspcare-2021-003042. [ Links ]
23. McIlfatrick S. Assessing palliative care needs: views of patients, informal carers and healthcare professionals. J Adv Nurs. 2007; 57(1). doi: 10.1111/j.1365-2648.2006.04062.x. [ Links ]
24. Antonione R, Nodari S, Fieramosca M. Criteri di selezione del malato con scompenso cardiaco da avviare a cure palliative [Selection criteria to palliative care implementation in advanced heart failure]. G Ital Cardiol (Rome). 2020;21(4):272-277. doi: 10.1714/3328.32987. [ Links ]
25. Ganz F, Roeh K, Eid M, Hasin T, Harush C, Gotsman I. The need for palliative and support care services for heart failure patients in the community. Eur J Cardiovasc Nurs. 2020. doi: 10.1177/1474515120951970. [ Links ]
26. Boje J, Madsen J, Finderup J. Palliative care needs experienced by Danish patients with end-stage kidney disease. Journal of Renal Care. 2020. doi: 10.1111/jorc.12347. [ Links ]
27. Martinez-Litago E, Martínez-Velasco MC, Muniesa-Zaragozano MP. Palliative care and end-of-life care for polypathological patients. Rev Clin Esp (Barc). 2017; 217(9): 543-552. doi: 10.1016/j.rce.2017.08.005. [ Links ]
28. Downar J, Goldman R, Pinto R, Englesakis M, Adhikari NK. The "surprise question" for predicting death in seriously ill patients: a systematic review and meta-analysis. CMAJ. 2017; 189(13): E484-E493. doi: 10.1503/cmaj.160775. [ Links ]
29. de-la-Rica-Escuín M, García-Barrecheguren A, Monche-Palacín AM. Assessment of the needs for palliative care in advanced chronic patients on discharge. Enferm Clin. 2019 Jan-Feb;29(1):18-26. doi: 10.1016/j.enfcli.2018.07.004. [ Links ]
30. Tripodoro VA, Rynkiewicz MC, Llanos V, Padova S, De Lellis S, De Simone G. Atención paliativa en personas con enfermedades crónicas avanzadas [Palliative care needs in advanced chronic illness]. Medicina (B Aires). 2016;76(3):139-47. [ Links ]
Cite as: Pinedo-Torres I, Intimayta- Escalante C, Jara-Cuadros D, Yañez- Camacho W, Zegarra-Lizana P, Saire-Huamán R. Association between the need for palliative care and chronic diseases in patients treated in a Peruvian hospital. Rev Peru Med Exp Salud Publica. 2021;38(4):569-76. doi: https://doi.org/10.17843/rpmesp.2021.384.9288.
Received: August 12, 2021; Accepted: December 09, 2021











 texto en
texto en