Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Medicina Experimental y Salud Publica
Print version ISSN 1726-4634On-line version ISSN 1726-4642
Rev. perú. med. exp. salud publica vol.40 no.2 Lima Apr./Jun. 2023 Epub June 30, 2023
http://dx.doi.org/10.17843/rpmesp.2023.402.12170
Original article
Comorbidities associated with COVID-19 mortality in adults in Lima, Peru: a retrospective cohort study
1 Centro Nacional de Epidemiología, Prevención y Control de Enfermedades, Ministerio de Salud. Lima, Peru.
Objectives.
To evaluate comorbidities associated with mortality in adult patients hospitalized due to COVID-19 in hospitals in Lima and Callao.
Materials and methods.
In this retrospective cohort study, we analyzed data from adult patients hospitalized due to COVID-19 reported to the National Epidemiological Surveillance System of the Peruvian Ministry of Health from March to October 2020. We estimated relative risks with 95% confidence intervals using Poisson regression models with robust variance to assess comorbidities associated with mortality by age group: young adults (18-29 years), adults (30-59 years) and older adults (≥60 years).
Results.
We included 2366 young adults, 23,781 adults and 25,356 older adults. Older adults had the highest mortality (63.7%) compared to adults (27.1%) and young adults (8.5%). Regardless of age group, the presence of neurological disease, renal disease, liver disease, and cancer was associated with an increased risk of mortality. Additionally, cardiovascular disease was also a risk factor in young adults; obesity, diabetes, cardiovascular disease, chronic lung disease, and immunodeficiency in adults; and obesity and chronic lung disease in the elderly.
Conclusions.
Regardless of age groups, individuals with chronic neurologic disease, renal disease, liver disease, and cancer were at high risk of death from COVID-19.
Keywords: COVID-19; Comorbidity; Prognosis; Hospitalization; Peru
- Motivation for the study. During the COVID-19 pandemic, the mortality rate from this disease was higher in adults and the elderly. Therefore, it is important to identify the factors that were associated with mortality from COVID-19 in adults, by age group.
- Main findings. Chronic neurological disease, kidney disease, liver disease, and cancer increased the risk of dying from COVID-19 in the three age groups we analyzed, which were made up of hospitalized patients from Lima and Callao. The risk of mortality associated with comorbidities was higher in patients aged 18 to 29.
- Implications. This study helps to identify the groups of patients with the highest risk of death from COVID-19, according to age group and type of comorbidity.
Keywords: COVID-19; Comorbidity; Prognosis; Hospitalization; Peru
INTRODUCTION
In Peru, the first wave of the 2019 coronavirus disease pandemic (COVID-19) began on March 6, 2020. Since then, Peru has experienced five waves with more than four million people infected, of which almost three hundred thousand required hospitalization 1. COVID-19 took the Peruvian health system by surprise and caused the collapse of hospitals right at the beginning of the pandemic. Nationally, there were only about one hundred intensive care beds and oxygen volume production was limited 2. The government responded to this situation with several measures, including restricting mobilization and reinforcing the health system 3. Within four months, the number of intensive care beds was increased to almost 1000 2. However, the number of cases increased again in November, triggering a second wave, with almost two million cumulative cases and almost 200,000 deaths 1.
The clinical spectrum of SARS-CoV-2 infection ranges from asymptomatic infection to severe disease; the highest percentage of cases are asymptomatic, mild or moderate, but there is a group of patients who develop severe disease, require hospital management and have a higher risk of death 4. Studies in different populations, have shown that the following are risk factors for mortality from COVID-19: older age, male sex, comorbidities such as obesity, cardiovascular disease, cancer, chronic kidney disease, immunosuppression, as well as clinical factors such as oxygen saturation at hospital admission, elevated creatinine and lactate dehydrogenase (LDH) levels 5-8. In addition, the collapse of the healthcare system also played a crucial role in mortality.
Understanding the main factors that increase the risk of death is crucial to improve the health system response. Few studies have investigated the factors associated with mortality in different age groups. In this study, we sought to evaluate comorbidities associated with mortality in adult patients hospitalized in the provinces of Lima and Callao during the first wave of COVID-19 in Peru.
MATERIALS AND METHODS
Study design and data sources
We conducted a retrospective cohort study, using data from the National Epidemiological Surveillance System of the Peruvian Ministry of Health (NotiWeb) 11, which collects clinical and epidemiological data on different notifiable infectious diseases, and from the National Mortality Agency (SINADEF) database, which collects data from death certificates 12. The national identity document (DNI) or immigration card (CE) was used as a unique identifier to unite the two databases, once consolidated, the data was encrypted using a process developed by the General Office of Information Technologies (OGTI) of the Ministry of health. Subsequently, the nominal data was eliminated, leaving only a generated identifier. The person in charge of carrying out this process was JPVR (author). For the analysis, only the consolidated database with the encrypted identifiers was shared.
Study population
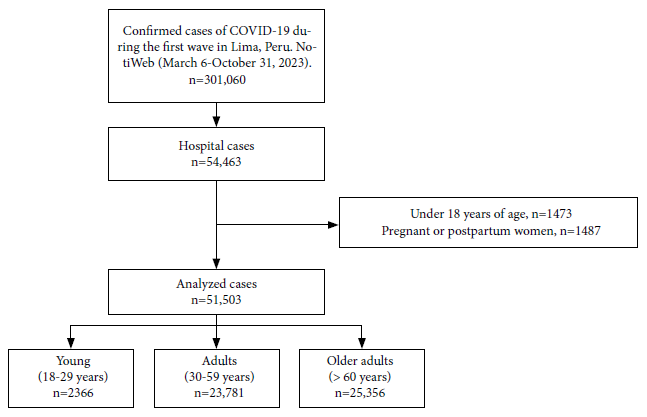
We analyzed all cases reported during the first wave of the COVID-19 pandemic in Peru (from March 6 to October 31, 2020). We included patients older than 18 years with a confirmed diagnosis of COVID-19 (positive molecular PCR or reactive IgM/IgG rapid test) 9, who were hospitalized in a health facility. Pregnant and postpartum women were excluded from the analysis.
Dependent and independent variable
Mortality was the dependent variable. Deceased patients were considered as those who were registered in the SINADEF database from March 6 to September 10, 2021 and whose cause of death was one of the following ICD-10 codes: B972 (coronavirus as cause of diseases classified in other chapters), U071 (acute respiratory illness due to the new coronavirus) or U072 (COVID-19, unidentified virus). If the case did not meet this criterion, it was defined as a survivor. The independent variables were the comorbidities registered in the epidemiological record. These included obesity, diabetes, cardiovascular disease, chronic neurological disease, kidney disease, chronic lung disease, asthma, liver disease, immunodeficiency, and cancer.
Covariates
We also included other variables from the epidemiological records. The demographic variables included age in years, sex (male, female), and health worker status (no, yes). We defined the age groups according to the classification of the Ministry of Health: youth (18-29 years), adults (30-59 years) and older adults (≥60 years) 10. Other variables were admission to the intensive care unit (ICU), the need for mechanical ventilation support and the type of health facility (EESS) with four categories: Ministry of Health (MINSA), Social Health Security (EsSalud), Armed Forces and National Police (FFAA/PNP) and private institutions. The time in which the case was reported was divided into four periods (March/April, May/June, July/August, September/October).
Statistical analysis
Categorical variables are displayed using absolute and relative frequencies.
We used chi-square tests to compare characteristics between age groups, as well as to compare the characteristics between deceased and survivors in each of the age groups. To assess comorbidities associated with mortality, we estimated crude and adjusted relative risks (RR) with their confidence intervals (95% CI) using Poisson regression with robust variance. The regression analyzes were performed while stratifying by age group. The adjusted model included the following variables: age in years, sex, being a health worker, admission to intensive care, need for mechanical ventilation, type of health facility, and the period in which the case was reported, based on epidemiological criteria. A value of p<0.05 was considered statistically significant. Data was cleaned and analyzed in R, version 4.0.3 (R Foundation for Statistical Computing).
Ethical aspects
This study used secondary databases of the National Epidemiological Surveillance System of the Ministry of Health of Peru; the databases we used were completely anonymized. This study was approved by the CDC - Peru for its publication (file No. 21-145573-001). The study was also registered on the Health Research Projects Registry (PRISA) portal, with the code: EI00000002704.
RESULTS
Population characteristics
We included 51,503 confirmed cases of COVID-19 that were reported to the epidemiological surveillance system as hospitalized in the provinces of Lima and Callao during the first wave of the COVID-19 pandemic in Peru, who met the inclusion criteria described in Figure 1. Most of the cases were adults (46.2%) or older adults (49.2%); 60.4% were male and most were hospitalized in MINSA (39.5%) or EsSalud (40.4%) health establishments. Comorbidities were reported in 29.2% of the patients. The most frequent comorbidities were cardiovascular disease (15.6%), diabetes (11.1%), and obesity (5.14%); 7.9% were admitted to intensive care and 6.6% used mechanical ventilation. When comparing by age groups, we found that comorbidities were present in 8.8%, 21.9%, and 37.9% of the young, adult, and older adult cases, respectively (p<0.001). The prevalence of comorbidities increased in relation to the age groups (p<0.050), with the exception of obesity, asthma and immunodeficiencies, which were more frequent among the adult population. Older adults died more frequently (63.7%) compared to adults (27.1%) and young people (8.5%, p<0.001). The frequency of ICU admission and use of mechanical ventilation also increased with age (Table 1).
Table 1 General and clinical characteristics of patients with confirmed COVID-19 who were hospitalized in health facilities in Lima, Peru. March to October 2020.
| Factors | Total N=51,503 | Age groups | p-value a | ||
|---|---|---|---|---|---|
| Young (18-29) | Adults (30-59) | Older adults (≥60) | |||
| n=2366 (4.6%) | n=23,781 (46.2%) | n=25,356 (49.2%) | |||
| n (%) | n (%) | n (%) | n (%) | ||
| Sex | <0.001 | ||||
| Male | 31,104 (60.4) | 939 (39.7) | 15,099 (63.5) | 15,066 (59.4) | |
| Female | 20,399 (39.6) | 1427 (60.3) | 8682 (36.5) | 10,290 (40.6) | |
| Healthcare worker | <0.001 | ||||
| No | 46,601 (90.5) | 2132 (90.1) | 21,144 (88.9) | 23,325 (92.0) | |
| Yes | 4902 (9.5) | 234 (9.9) | 2637 (11.1) | 2031 (8.0) | |
| Comorbidities | 15,026 (29.2) | 208 (8.8) | 5219 (21.9) | 9599 (37.9) | <0.001 |
| Obesity | 2649 (5.1) | 95 (4.0) | 1570 (6.6) | 984 (3.9) | <0.001 |
| Diabetes | 5737 (11.1) | 30 (1.3) | 1944 (8.2) | 3763 (14.8) | <0.001 |
| Cardiovascular disease | 8059 (15.6) | 26 (1.1) | 1814 (7.6) | 6219 (24.5) | <0.001 |
| Chronic neurological disease | 536 (1.0) | 12 (0.5) | 138 (0.6) | 386 (1.5) | <0.001 |
| Kidney disease | 1144 (2.2) | 19 (0.8) | 324 (1.4) | 801 (3.2) | <0.001 |
| Chronic pulmonary disease | 847 (1.6) | 16 (0.7) | 244 (1.03) | 587 (2.3) | <0.001 |
| Asthma | 637 (1.2) | 31 (1.3) | 351 (1.5) | 255 (1.0) | 0.001 |
| Liver disease | 279 (0.5) | 6 (0.3) | 89 (0.4) | 184 (0.7) | <0.001 |
| Immunodeficiency | 157 (0.3) | 8 (0.3) | 98 (0.4) | 51 (0.2) | 0.004 |
| Cancer | 757 (1.5) | 15 (0.6) | 243 (1.0) | 499 (2.0) | <0.001 |
| Type of health establishment | <0.001 | ||||
| MINSA | 20,353 (39.5) | 1471 (62.2) | 9584 (40.3) | 9298 (36.7) | |
| EsSalud | 20,830 (40.4) | 454 (19.2) | 8260 (34.7) | 12,116 (47.8) | |
| FFAA/PNP | 3368 (6.6) | 122 (5.1) | 1649 (7.0) | 1597 (6.3) | |
| Private | 6952 (13.5) | 319 (13.5) | 4288 (18.0) | 2345 (9.2) | |
| Admission to ICU | 3403 (6.6) | 58 (2.5) | 1748 (7.4) | 1597 (6.3) | <0.001 |
| Use of mechanical ventilation | 4073 (7.9) | 83 (3.5) | 2152 (9.1) | 1838 (7.2) | <0.001 |
| Infection period | <0.001 | ||||
| March/April, 2020 | 5911 (11.5) | 204 (8.6) | 3072 (12.9) | 2635 (10.4) | |
| June/July, 2020 | 19,580 (38.0) | 899 (38.0) | 9033 (38.0) | 9648 (38.0) | |
| August/September, 2020 | 19,027 (36.9) | 816 (34.5) | 8688 (36.5) | 9523 (37.6) | |
| October/November, 2020 | 6985 (13.6) | 447 (18.9) | 2988 (12.6) | 3550 (14.0) | |
| Deceased | 22,787 (44.2) | 200 (8.5) | 6445 (27.1) | 16,142 (63.7) | <0.001 |
a p-value calculated with the chi-square test.
MINSA: Ministry of Health; EsSalud: Peruvian Social Health Insurance; FFAA/PNP: Armed Forces and National Police; ICU: intensive care unit.
Characteristics according to age group and mortality
Males died more frequently than females (p<0.001). Mortality was significantly lower in cases hospitalized in a private establishment compared to establishments linked to public services (p<0.001). Mortality was lower in adults who were health workers (23.1%) compared to those who were not (27.6%, p<0.001). Mortality was higher in cases with comorbidities, especially among young people. Young people with some comorbidity had three times (7.2% vs. 21.6%) the probability of dying than those young patients without comorbidities (p<0.001). Adult and older adult patients with comorbidities also died more frequently than those without comorbidities, but the difference was smaller than in younger patients. Both in the group of young people, adults and the elderly, cases with cardiovascular disease, chronic neurological disease, kidney disease, liver disease or cancer had a higher frequency of mortality compared to those without these conditions (p<0.05) (Table 2).
Table 2 Comparison of characteristics between deceased and survivor patients with confirmed 2019 coronavirus disease admitted to hospitalization in health facilities in Lima, Peru. March to October 2020.
| Factors | Young (18-29) | p-value a | Adults (30-59) | p-value a | Older adults (≥60) | p-value a | |||
|---|---|---|---|---|---|---|---|---|---|
| Survivors n=2166 | Deceased n=200 | Survivors n=17,336 | Deceased n=6445 | Survivors n=9214 | Deceased n=16,142 | ||||
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||||
| Sex | <0.001 | <0.001 | <0.001 | ||||||
| Female | 1347 (94.4) | 80 (5.6) | 6682 (77.0) | 2000 (23.0) | 4144 (40.3) | 6146 (59.7) | |||
| Male | 819 (87.2) | 120 (12.8) | 10 654 (70.6) | 4445 (29.4) | 5070 (33.7) | 9996 (66.3) | |||
| Health worker | 0.417 | <0.001 | 0.756 | ||||||
| No | 1948 (91.4) | 184 (8.6) | 15 308 (72.4) | 5836 (27.6) | 8469 (36.3) | 14 856 (63.7) | |||
| Yes | 218 (93.2) | 16 (6.8) | 2028 (76.9) | 609 (23.1) | 745 (36.7) | 1286 (63.3) | |||
| Comorbidities | <0.001 | <0.001 | <0.001 | ||||||
| No | 2003 (92.8) | 155 (7.2) | 14 022 (75.5) | 4540 (24.5) | 5935 (37.7) | 9822 (62.3) | |||
| Yes | 163 (78.4) | 45 (21.6) | 3314 (63.5) | 1905 (36.5) | 3279 (34.2) | 6320 (65.8) | |||
| Obesity | 0.192 | <0.001 | 0.018 | ||||||
| No | 2083 (91.7) | 188 (8.3) | 16,387 (73.8) | 5824 (26.2) | 8892 (36.5) | 15,480 (63.5) | |||
| Yes | 83 (87.4) | 12 (12.6) | 949 (60.4) | 621 (39.6) | 322 (32.7) | 662 (67.3) | |||
| Diabetes | 0.036 | <0.001 | 0.684 | ||||||
| No | 2142 (91.7) | 194 (8.3) | 16,072 (73.6) | 5765 (26.4) | 7835 (36.3) | 13,758 (63.7) | |||
| Yes | 24 (80.0) | 6 (20.0) | 1264 (65.0) | 680 (35.0) | 1379 (36.6) | 2384 (63.4) | |||
| Cardiovascular disease | <0.001 | <0.001 | <0.001 | ||||||
| No | 2150 (91.9) | 190 (8.1) | 16,173 (73.6) | 5794 (26.4) | 7089 (37.0) | 12,048 (63.0) | |||
| Yes | 16 (61.5) | 10 (38.5) | 1163 (64.1) | 651 (35.9) | 2125 (34.2) | 4094 (65.8) | |||
| Chronic neurological disease | <0.001 | <0.001 | <0.001 | ||||||
| No | 2160 (91.8) | 194 (8.2) | 17,255 (73.0) | 6388 (27.0) | 9120 (36.5) | 15,850 (63.5) | |||
| Yes | 6 (50.0) | 6 (50.0) | 81 (58.7) | 57 (41.3) | 94 (24.4) | 292 (75.6) | |||
| Kidney disease | <0.001 | <0.001 | <0.001 | ||||||
| No | 2157 (91.9) | 190 (8.1) | 17,188 (73.3) | 6269 (26.7) | 9006 (36.7) | 15,549 (63.3) | |||
| Yes | 9 (47.4) | 10 (52.6) | 148 (45.7) | 176 (54.3) | 208 (26.0) | 593 (74.0) | |||
| Chronic lung disease | 0.640 | <0.001 | <0.001 | ||||||
| No | 2152 (91.6) | 198 (8.4) | 17,188 (73.0) | 6349 (27.0) | 9066 (36.6) | 15,703 (63.4) | |||
| Yes | 14 (87.5) | 2 (12.5) | 148 (60.7) | 96 (39.3) | 148 (25.2) | 439 (74.8) | |||
| Asthma | 0.742 | 0.199 | 0.305 | ||||||
| No | 2138 (91.6) | 197 (8.4) | 17,069 (72.9) | 6361 (27.1) | 9113 (36.3) | 15,988 (63.7) | |||
| Yes | 28 (90.3) | 3 (9.7) | 267 (76.1) | 84 (23.9) | 101 (39.6) | 154 (60.4) | |||
| Liver disease | 0.085 | <0.001 | 0.005 | ||||||
| No | 2162 (91.6) | 198 (8.4) | 17,287 (73.0) | 6405 (27.0) | 9166 (36.4) | 16,006 (63.6) | |||
| Yes | 4 (66.7) | 2 (33.3) | 49 (55.1) | 40 (44.9) | 48 (26.1) | 136 (73.9) | |||
| Immunodeficiency | 0.507 | <0.001 | 0.554 | ||||||
| No | 2159 (91.6) | 199 (8.4) | 17,291 (73.0) | 6392 (27.0) | 9198 (36.3) | 16,107 (63.7) | |||
| Yes | 7 (87.5) | 1 (12.5) | 45 (45.9) | 53 (54.1) | 16 (31.4) | 35 (68.6) | |||
| Cancer | <0.001 | <0.001 | <0.001 | ||||||
| No | 2162 (92.0) | 189 (8.0) | 17,234 (73.2) | 6304 (26.8) | 9098 (36.6) | 15,759 (63.4) | |||
| Yes | 4 (26.7) | 11 (73.3) | 102 (42.0) | 141 (58.0) | 116 (23.2) | 383 (76.8) | |||
| Type of health facility | <0.001 | <0.001 | <0.001 | ||||||
| MINSA | 1353 (92.0) | 118 (8.02) | 6237 (65.1) | 3347 (34.9) | 3088 (33.2) | 6210 (66.8) | |||
| EsSalud | 392 (86.3) | 62 (13.7) | 5891 (71.3) | 2369 (28.7) | 4113 (33.9) | 8003 (66.1) | |||
| FFAA/PNP | 109 (89.3) | 13 (10.7) | 1259 (76.3) | 390 (23.7) | 533 (33.4) | 1064 (66.6) | |||
| Private | 312 (97.8) | 7 (2.2) | 3949 (92.1) | 339 (7.9) | 1480 (63.1) | 865 (36.9) | |||
| Admission to ICU | <0.001 | <0.001 | <0.001 | ||||||
| No | 2134 (92.5) | 174 (7.5) | 16,679 (75.7) | 5354 (24.3) | 8930 (37.6) | 14,829 (62.4) | |||
| Yes | 32 (55.2) | 26 (44.8) | 657 (37.6) | 1091 (62.4) | 284 (17.8) | 1313 (82.2) | |||
| Use of mechanical ventilation | <0.001 | 0.000 | <0.001 | ||||||
| No | 2122 (92.9) | 161 (7.1) | 16,563 (76.6) | 5066 (23.4) | 8900 (37.8) | 14,618 (62.2) | |||
| Yes | 44 (53.0) | 39 (47.0) | 773 (35.9) | 1379 (64.1) | 314 (17.1) | 1524 (82.9) | |||
| Diagnostic period | 0.182 | <0.001 | <0.001 | ||||||
| March/April, 2020 | 179 (87.7) | 25 (12.3) | 2242 (73.0) | 830 (27.0) | 990 (37.6) | 1645 (62.4) | |||
| June/July, 2020 | 821 (91.3) | 78 (8.7) | 6307 (69.8) | 2726 (30.2) | 3150 (32.6) | 6498 (67.4) | |||
| August/September,2020 | 754 (92.4) | 62 (7.6) | 6361 (73.2) | 2327 (26.8) | 3558 (37.4) | 5965 (62.6) | |||
| October/November, 2020 | 412 (92.2) | 35 (7.8) | 2426 (81.2) | 562 (18.8) | 1516 (42.7) | 2034 (57.3) | |||
a p-value calculated with the chi-square test.
MINSA: Ministry of Health; EsSalud: Peruvian Social Health Insurance; FFAA/PNP: Armed Forces and National Police; ICU: intensive care unit.
Comorbidities associated with mortality
In the adjusted regression analysis, we found that neurological disease, kidney disease, liver disease, and cancer were associated with a higher risk of mortality regardless of age group. Additionally, cardiovascular disease (RR=2.16; 95% CI: 1.24-3.74) was associated with a higher risk of mortality in young patients. In adults, obesity (RR=1.30; 95% CI: 1.22-1.39), diabetes (RR=1.12; 95% CI: 1.06-1.20), cardiovascular disease (RR=1.14; 95% CI: 1.07-1.21), chronic lung disease (RR=1.30; 95% CI: 1.1-1.51) and immunodeficiency (RR=2 .18; 95% CI: 1.77-2.69) were also comorbidities associated with mortality. Obesity (RR=1.12; 95% CI: 1.07-1.17) and chronic lung disease (RR=1.13; 95% CI: 1.07-1.18) were also associated with mortality in older patients. Asthma was not associated with an increased risk of mortality in the bivariate or multivariate analysis for any of the age groups (Table 3).
Table 3 Poisson regression analysis with robust variance for comorbidities associated with in-hospital mortality in patients with COVID-19 admitted to hospitalization in Lima, Peru. March to October 2020.
| Comorbidities | Crude model | Adjusted model a | ||||
|---|---|---|---|---|---|---|
| RR | 95% CI | p-value | RR | 95% CI | p-value | |
| Age 18-29 years (n=2366) | ||||||
| Obesity | 1.53 | 0.88-2.63 | 0.130 | 0.75 | 0.45-1.26 | 0.282 |
| Diabetes | 2.41 | 1.16-4.99 | 0.018 | 1.46 | 0.72-2.96 | 0.296 |
| Cardiovascular disease | 4.74 | 2.86-7.85 | <0.001 | 2.16 | 1.24-3.74 | 0.006 |
| Chronic neurological disease | 6.07 | 3.39-10.85 | <0.001 | 5.03 | 2.60-9.74 | <0.001 |
| Renal disease | 6.50 | 4.15-10.17 | <0.001 | 5.01 | 2.88-8.71 | <0.001 |
| Chronic lung disease | 1.48 | 0.40-5.46 | 0.553 | 0.86 | 0.31-2.40 | 0.777 |
| Asthma | 1.15 | 0.39-3.39 | 0.804 | 0.51 | 0.24-1.10 | 0.087 |
| Liver disease | 3.97 | 1.27-12.42 | 0.018 | 3.82 | 1.16-12.55 | 0.027 |
| Immunodeficiency | 1.48 | 0.24-9.31 | 0.675 | 1.02 | 0.16-6.61 | 0.986 |
| Cancer | 9.12 | 6.53-12.74 | <0.001 | 7.29 | 4.56-11.64 | <0.001 |
| Age 30-59 years (n=23,781) | ||||||
| Obesity | 1.51 | 1.41-1.61 | <0.001 | 1.30 | 1.22-1.39 | <0.001 |
| Diabetes | 1.32 | 1.24-1.41 | <0.001 | 1.12 | 1.06-1.20 | <0.001 |
| Cardiovascular disease | 1.36 | 1.27-1.45 | <0.001 | 1.14 | 1.07-1.21 | <0.001 |
| Chronic neurological disease | 1.53 | 1.25-1.87 | <0.001 | 1.36 | 1.12-1.65 | 0.002 |
| Kidney disease | 2.03 | 1.84-2.25 | <0.001 | 1.87 | 1.68-2.09 | <0.001 |
| Chronic lung disease | 1.46 | 1.25-1.71 | <0.001 | 1.30 | 1.11-1.51 | 0.001 |
| Asthma | 0.88 | 0.73-1.06 | 0.188 | 0.92 | 0.77-1.10 | 0.378 |
| Liver disease | 1.66 | 1.32-2.09 | <0.001 | 1.55 | 1.21-1.99 | 0.001 |
| Immunodeficiency | 2.00 | 1.67-2.41 | <0.001 | 2.18 | 1.77-2.69 | <0.001 |
| Cancer | 2.17 | 1.94-2.42 | <0.001 | 2.38 | 2.10-2.70 | <0.001 |
| Age >60 years (n=25,356) | ||||||
| Obesity | 1.06 | 1.01-1.11 | 0.011 | 1.12 | 1.07-1.17 | <0.001 |
| Diabetes | 0.99 | 0.97-1.02 | 0.672 | 1.00 | 0.98-1.03 | 0.859 |
| Cardiovascular disease | 1.05 | 1.02-1.07 | <0.001 | 0.99 | 0.96-1.01 | 0.179 |
| Chronic neurological disease | 1.19 | 1.13-1.26 | <0.001 | 1.10 | 1.03-1.16 | 0.002 |
| Kidney disease | 1.17 | 1.12-1.22 | <0.001 | 1.10 | 1.06-1.15 | <0.001 |
| Chronic lung disease | 1.18 | 1.12-1.24 | <0.001 | 1.13 | 1.07-1.18 | <0.001 |
| Asthma | 0.95 | 0.86-1.05 | 0.296 | 0.98 | 0.89-1.07 | 0.613 |
| Liver disease | 1.16 | 1.07-1.27 | 0.001 | 1.20 | 1.10-1.31 | <0.001 |
| Immunodeficiency | 1.08 | 0.90-1.30 | 0.427 | 1.14 | 0.96-1.37 | 0.144 |
| Cancer | 1.21 | 1.15-1.27 | <0.001 | 1.23 | 1.17-1.29 | <0.001 |
a Adjusted for age, sex in years, being health personnel, admission to intensive care, need for mechanical ventilation, type of health facility and the period in which the case was reported. RR: relative risk, 95% CI: 95% confidence interval.
DISCUSSION
In this study, we analyzed data from adult patients with COVID-19 who were hospitalized during the first wave of the pandemic in Lima, Peru. We found that the frequency of comorbidities and mortality increased with age. Chronic neurological disease, kidney disease, liver disease, and cancer were associated with mortality, regardless of the age group. The risk of mortality associated with comorbidities was higher in young adults compared to adults and older adults. To our knowledge, this is the first study to assess comorbidities associated with mortality in different age groups. Previous studies in Peru have reported that oxygen saturation on admission 6,13, being over 65 years of age, lactate dehydrogenase greater than 720 U/L 13 and the use of mechanical ventilation or admission to the ICU 14 were factors associated with mortality.
The mortality rate in Lima and Callao was higher compared to the world average, estimated at 15% by a systematic review 15, but similar to other Latin American countries such as Colombia (40%) (16. Different factors can explain why Peru has one of the highest mortality rates in the world. A contributing factor could be the collapse of the health system due to the rapid occupation of hospitalization and critical care beds, the lack of oxygen and mechanical ventilation equipment 17 and the high rates of self-medication with antibiotics or anti-inflammatories among the general population, which was estimated to be around 39% among the residents of Lima 18.
Patients older than 59 years had a mortality rate 20-times higher than those aged 18 to 29 years. Young adults had a mortality rate similar to what was reported by a study in the United States 19. Older adults had higher mortality rates compared to other high-income countries (35.5%) 20, but similar to studies conducted in Latin American countries such as Brazil (64%) 21 and Mexico (69%). 22. Age is one of the independent risk factors for mortality, identified since the beginning of the pandemic 23. Older people have a lower functional reserve and higher levels of angiotensin-converting enzyme 2 (ACE2), which may play a key role in the multiorgan involvement caused by SARS-CoV-2 24. Interestingly, we found that the risk of mortality associated with comorbidities was higher in young patients (18-29 years) compared to older patients. Younger patients with comorbidities died three times more than young patients without comorbidities, a difference much greater than what was found in older patients. Regression models showed greater association between comorbidities and mortality in younger patients than in older patients. One potential explanation is that young patients may have more severe or complex comorbidities than older patients leading to a worse prognosis when contracting COVID-19 and suggests that young people with comorbidities may require particularly close monitoring as high-risk group.
Chronic neurological disease, kidney disease, liver disease, and cancer were associated with mortality, regardless of age group. This finding is consistent with previous research. For example, a study in Spain found that patients with pre-existing neurological comorbidities were 1.76 times more likely to die, regardless of bed occupancy or the type of treatment 25. This could be explained by the baseline health status of these patients; patients with chronic neurological disease have greater frailty and less reserve than people without chronic neurological disease. Neurological manifestations during acute illness have also been associated with a worse prognosis 26. A systematic review showed that patients with chronic kidney disease are seven times more likely to die than patients without pre-existing disease 27. Patients with kidney disease are in a proinflammatory state and have functional defects in innate and acquired immune cells, which increases vulnerability to infection and also worsens the prognosis 28. Several studies have also shown that patients with chronic kidney disease are at increased risk of pneumonia and severe pneumonia 29. Liver disease has also been associated with severity and mortality 30. Obesity was also a risk factor for the group of patients over 30 years of age, which is consistent with a meta-analysis that reported that obese patients had up to four times more mortality 31. We found no association regarding cases between 18 and 29 years of age. We did not find an association between asthma and an increased risk of mortality. This result also agrees with previous articles. The WHO conducted a systematic review that concluded that the role of asthma as a risk factor for death from COVID-19 remains unclear 32. Another review found that the risk of infection was lower in people with asthma compared to non-asthmatics, but found no difference in terms of hospitalization, intensive care admission, ventilator use, or mortality 33.
Our study has some limitations. First, this is a retrospective analysis of secondary data (mainly from the epidemiological surveillance system) that was not designed to estimate risk factors. For this reason, we could not include as many clinical details as an electronic medical record would. We found a lower prevalence of obesity 34, chronic obstructive pulmonary disease 35 and kidney disease 36 than studies with specialized tests, which could be due to the lack of standardized epidemiological definitions of comorbidities. We were also unable to explore the severity of comorbidities, which may modify the effect on mortality. Our findings should be cautiously applied to other populations due to the unique chaotic situation experienced during the first wave of the pandemic in Peru, which may not reflect the reality of all hospitalized COVID-19 patients. We do not have data on variables such as oxygen saturation on admission or the treatment received during hospitalization, which could play an important role in the mortality rates. Some patients were diagnosed only with rapid serological tests. These tests have a lower diagnostic performance than molecular tests, so it is possible that some patients had false positives and false negatives. On the other hand, this study has the strength of analyzing a broad and representative sample of hospitalized patients. Previous studies in local settings have not explored comorbidities associated with mortality, so our results complement the study of COVID-19 in Peru. Furthermore, this is the first study to evaluate associated comorbidities by age group. Our multivariate analysis considered possible confounding factors, such as hospital ICU bed occupancy, type of health facility, and time from symptom onset to hospitalization.
In conclusion, in this retrospective cohort of hospitalized patients with COVID-19, we found evidence that chronic neurological disease, kidney disease, liver disease, and cancer were comorbidities associated with mortality regardless of age group. Furthermore, despite the fact that patients older than 60 years had higher mortality compared with younger patients, the risk of mortality associated with comorbidities was higher in young adults.
REFERENCES
1. Ministerio de Salud. Sala Situacional - COVID 19 en el Perú [Internet]. [citado el 30 de julio de 2020]. Disponible en: https://covid19.minsa.gob.pe/sala_situacional.asp. [ Links ]
2. Acciones del Gobierno frente al COVID-19 (08/05/2020) [Internet]. [citado el 18 de mayo de 2020]. Disponible en: https://www.gob.pe/institucion/pcm/informes-publicaciones/563660-acciones-del-gobierno-frente-al-covid-19-08-05-2020. [ Links ]
3. Ministerio de Salud (MINSA). Resolución Ministerial N° 184-2020-MINSA. Creación de el Grupo de Trabajo de innovación de tecnologías sanitarias [Internet]. 2020 [citado el 10 de mayo de 2020]. Disponible en: https://www.gob.pe/institucion/minsa/normas-legales/473513-184-2020-minsa. [ Links ]
4. Díaz-Vélez C, Urrunaga-Pastor D, Romero-Cerdán A, Peña-Sánchez ER, Fernández Mogollon JL, Cossio Chafloque JD, et al. Risk factors for mortality in hospitalized patients with COVID-19 from three hospitals in Peru: a retrospective cohort study. F1000Res. 2021;10:224. doi:10.12688/f1000research.51474.1. [ Links ]
5. Parohan M, Yaghoubi S, Seraji A, Javanbakht MH, Sarraf P, Djalali M. Risk factors for mortality in patients with Coronavirus disease 2019 (COVID-19) infection: a systematic review and meta-analysis of observational studies. The Aging Male. 2020;23(5):1416-24. doi: 10.1080/13685538.2020.1774748. [ Links ]
6. Mejía F, Medina C, Cornejo E, Morello E, Vásquez S, Alave J, et al. Oxygen saturation as a predictor of mortality in hospitalized adult patients with COVID-19 in a public hospital in Lima, Peru. PLOS ONE. 2020;15(12):e0244171. doi: 10.1371/journal.pone.0244171. [ Links ]
7. Gesesew HA, Koye DN, Fetene DM, Woldegiorgis M, Kinfu Y, Geleto AB, et al. Risk factors for COVID-19 infection, disease severity and related deaths in Africa: a systematic review. BMJ Open. 2021;11(2):e044618. doi:10.1136/bmjopen-2020-044618. [ Links ]
8. Gao Y, Chen Y, Liu M, Shi S, Tian J. Impacts of immunosuppression and immunodeficiency on COVID-19: A systematic review and meta-analysis. Journal of Infection. 2020;81(2):e93-5. doi: 10.1016/j.jinf.2020.05.017. [ Links ]
9. Ministerio de Salud (MINSA). Alertas epidemiologicas 2020 [Internet]. [citado el 10 de mayo de 2020]. Disponible en: https://www.dge.gob.pe/portal/includes/boletin/alertas2020.html. [ Links ]
10. Ministerio de Salud del Perú. Documento Técnico: Modelo de Cuidado Integral de Salud por Curso de Vida [Internet]. [citado el 20 de marzo de 2023]. Disponible en: https://cdn.www.gob.pe/uploads/document/file/496394/resolucion-ministerial-030-2020-MINSA.pdf. [ Links ]
11. Centro Nacional de Epidemiología, Prevención y Control de Enfermedades. NotiWeb [Internet]. [citado el 22 de septiembre de 2021]. Disponible en: https://app7.dge.gob.pe/notiWeb/index.php/index/login#no-back-button. [ Links ]
12. Vargas-Herrera J, Ruiz KP, Nuñez GG, Ohno JM, Pérez-Lu JE, Huarcaya WV, et al. Resultados preliminares del fortalecimiento del sistema informático nacional de defunciones. Revista Peruana de Medicina Experimental y Salud Pública. 2018;35(3):505-14. doi: 10.17843/rpmesp.2018.353.3913. [ Links ]
13. Hueda-Zavaleta M, Copaja-Corzo C, Bardales-Silva F, Flores-Palacios R, Barreto-Rocchetti L, Benites-Zapata VA. Factores asociados a la muerte por COVID-19 en pacientes admitidos en un hospital público en Tacna, Perú. Revista Peruana de Medicina Experimental y Salud Pública [Internet]. 2021 [citado el 30 de junio de 2021];38(2). doi: 10.17843/rpmesp.2021.382.7158. [ Links ]
14. Vences MA, Pareja-Ramos JJ, Otero P, Veramendi-Espinoza LE, Vega-Villafana M, Mogollón-Lavi J, et al. Factors associated with mortality in patients hospitalized with COVID-19: A prospective cohort in a Peruvian national referral hospital. Medwave. 2021;21(06):e8231-e8231. doi: 10.5867/medwave.2021.06.8231. [ Links ]
15. Abate SM, Checkol YA, Mantefardo B. Global prevalence and determinants of mortality among patients with COVID-19: A systematic review and meta-analysis. Annals of Medicine and Surgery. 2021;64:102204. doi: 10.1016/j.amsu.2021.102204. [ Links ]
16. Nuñez-Ramos JA, Forero Illera E, Quintero Barrios JL, Macareno Arroyo HA, Larios Sanjuan DJ, Manzur Barbur MC, et al. Prognostic Factors in Hospitalized COVID-19 Patients at the Start of the Pandemic in Colombia: A Retrospective Cohort Study. Cureus. 13(5):e14865. doi: 10.7759/cureus.14865. [ Links ]
17. Sistema de Salud en el Perú y el COVID-19 [Internet]. Escuela de Gobierno y Políticas Públicas. [citado el 23 de septiembre de 2021]. Disponible en: https://escuela.pucp.edu.pe/gobierno. [ Links ]
18. Navarrete-Mejía PJ, Velasco-Guerrero JC, Loro-Chero L. Automedicación en época de pandemia: Covid-19. Rev Cuerpo Méd Hosp Nac Almanzor Aguinaga Asenjo. 2020;350-5. [ Links ]
19. Richardson S, Gitlin J, Kozel Z, Levy S, Rahman H, Hirsch JS, et al. In-Hospital 30-Day Survival Among Young Adults With Coronavirus Disease 2019: A Cohort Study. Open Forum Infect Dis. 2021;8(6):ofab233. doi: 10.1093/ofid/ofab233. [ Links ]
20. Becerra-Muñoz VM, Núñez-Gil IJ, Eid CM, García Aguado M, Romero R, Huang J, et al. Clinical profile and predictors of in-hospital mortality among older patients hospitalised for COVID-19. Age and Ageing. 2021;50(2):326-34. doi: 10.1093/ageing/afaa258. [ Links ]
21. Santos MM, Lucena EES, Bonfada D, Santos AC, Vechi HT, Lima KC. Brazilian Older People Hospitalized by COVID-19: Characteristics and Prognostic Factors in a Retrospective Cohort Study. J Appl Gerontol. 2021;40(6):571-81. doi: 10.1177/0733464820983976. [ Links ]
22. Sánchez-Ríos CP, Barreto-Rodríguez JO, Centeno-Sáenz GI, Vázquez-Rojas H. COVID-19 in older adults Mexican, descriptive analysis. Neumol Cir Torax. 2021;79(4):224-9. [ Links ]
23. Levin AT, Hanage WP, Owusu-Boaitey N, Cochran KB, Walsh SP, Meyerowitz-Katz G. Assessing the age specificity of infection fatality rates for COVID-19: systematic review, meta-analysis, and public policy implications. Eur J Epidemiol. 2020;35(12):1123-38. doi: 10.1007/s10654-020-00698-1. [ Links ]
24. Wallentin L, Lindbäck J, Eriksson N, Hijazi Z, Eikelboom JW, Ezekowitz MD, et al. Angiotensin-converting enzyme 2 (ACE2) levels in relation to risk factors for COVID-19 in two large cohorts of patients with atrial fibrillation. European Heart Journal. 2020;41(41):4037-46. doi: 10.1093/eurheartj/ehaa697. [ Links ]
25. García-Azorín D, Martínez-Pías E, Trigo J, Hernández-Pérez I, Valle-Peñacoba G, Talavera B, et al. Neurological Comorbidity Is a Predictor of Death in COVID-19 Disease: A Cohort Study on 576 Patients. Frontiers in Neurology. 2020;11:781. doi: 10.3389/fneur.2020.00781. [ Links ]
26. Eskandar EN, Altschul DJ, Ramos R de la G, Cezayirli P, Unda SR, Benton J, et al. Neurologic Syndromes Predict Higher In-Hospital Mortality in COVID-19. Neurology. 2021;96(11):e1527-38. doi: 10.1212/WNL.0000000000011356. [ Links ]
27. Menon T, Gandhi SAQ, Tariq W, Sharma R, Sardar S, Arshad AM, et al. Impact of Chronic Kidney Disease on Severity and Mortality in COVID-19 Patients: A Systematic Review and Meta-analysis. Cureus. 2021;13(4):e14279. doi: 10.7759/cureus.14279. [ Links ]
28. Betjes MGH. Immune cell dysfunction and inflammation in end-stage renal disease. Nat Rev Nephrol. 2013;9(5):255-65. doi: 10.1038/nrneph.2013.44. [ Links ]
29. Chou C-Y, Wang S-M, Liang C-C, Chang C-T, Liu J-H, Wang I-K, et al. Risk of Pneumonia Among Patients With Chronic Kidney Disease in Outpatient and Inpatient Settings: A Nationwide Population-Based Study. Medicine. 2014;93(27):e174. doi: 10.1097/MD.0000000000000174. [ Links ]
30. Nagarajan R, Krishnamoorthy Y, Rajaa S, Hariharan VS. COVID-19 Severity and Mortality Among Chronic Liver Disease Patients: A Systematic Review and Meta-Analysis. Prev Chronic Dis. 2022;19:E53. doi: 10.5888/pcd19.210228. [ Links ]
31. Hussain A, Mahawar K, Xia Z, Yang W, EL-Hasani S. Obesity and mortality of COVID-19. Meta-analysis. Obes Res Clin Pract. 2020;14(4):295-300. doi: 10.1016/j.orcp.2020.07.002. [ Links ]
32. Asthma and COVID-19 - studies from WHO/Europe [Internet]. [citado el 24 de septiembre de 2021]. Disponible en: https://www.euro.who.int/en/countries/belgium/news/news/2021/8/asthma-and-covid-19-studies-from-whoeurope. [ Links ]
33. Sunjaya AP, Allida SM, Di Tanna GL, Jenkins CR. Asthma and COVID-19 risk: a systematic review and meta-analysis. Eur Respir J. 2022;59(3):2101209. doi: 10.1183/13993003.01209-2021. [ Links ]
34. Chávez V EJ. Prevalencia de sobrepeso y obesidad en el Perú. Revista Peruana de Ginecología y Obstetricia. 2017;63(4):593-8. [ Links ]
35. Jaganath D, Miranda JJ, Gilman RH, Wise RA, Diette GB, Miele CH, et al. Prevalence of chronic obstructive pulmonary disease and variation in risk factors across four geographically diverse resource-limited settings in Peru. Respir Res. 2015;16:40. doi: 10.1186/s12931-015-0198-2. [ Links ]
36. Herrera-Añazco P, Pacheco-Mendoza J, Taype-Rondan A. La enfermedad renal crónica en el Perú: Una revisión narrativa de los artículos científicos publicados. Acta Médica Peruana. 2016;33(2):130-7. [ Links ]
Cite as: Soto-Cabezas MG, Reyes-Vega MF, Soriano-Moreno AN, Ordoñez-Ibargüen L, Martel KS, Flores-Jaime N, et al. Comorbidities associated with COVID-19 mortality in adults in Lima, Peru: a retrospective cohort study. Rev Peru Med Exp Salud Publica. 2023;40(2):132-40. doi: 10.17843/rpmesp.2023.402.12170.
Received: September 28, 2022; Accepted: May 03, 2023











 text in
text in