Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Medicina Experimental y Salud Publica
versión impresa ISSN 1726-4634versión On-line ISSN 1726-4642
Rev. perú. med. exp. salud publica vol.40 no.4 Lima oct./dic. 2023 Epub 18-Dic-2023
http://dx.doi.org/10.17843/rpmesp.2023.404.12977
Original article
Association between pre-bronchoscopy time of illness and post-bronchoscopy discharge time in pediatric patients with foreign body aspiration: retrospective cohort study in a Peruvian referral center, 2014-2019
1 Universidad Peruana de Ciencias Aplicadas, Lima, Peru.
2 Pediatric Emergency Hospital, Lima, Peru.
Objective.
To determine the association between pre-bronchoscopy time of illness and post-bronchoscopy discharge time in pediatric patients with foreign body aspiration.
Materials and methods.
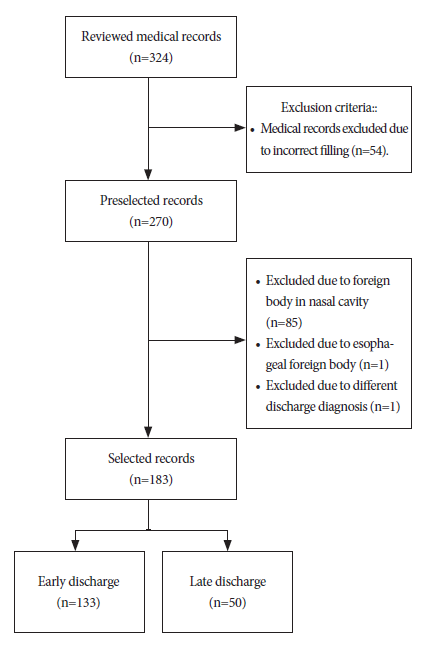
Retrospective cohort study. Medical records were studied and reviewed at the Pediatric Emergency Hospital of Lima, Peru. We reviewed 324 medical records, and selected 183 because they had the diagnosis of foreign body aspiration and complete data. Fisher’s exact test and Mann Whitney U test were used for the bivariate analysis, while Poisson regression was used to calculate the Relative Risk (RR) and its 95% confidence interval (CI).
Results.
We included 183 patients, of whom 65.6% were men with a mean age of 2.4 years. The most frequent location of the foreign body was the right bronchial tree and most of them were made of organic material. The majority (72.7%) of patients were discharged before 24 hours. We found an association between the time of illness prior to bronchoscopy and post-bronchoscopy discharge time (RR: 2.94, 95%CI: 1.72 - 5.01).
Conclusions.
The time of illness prior to bronchoscopy and the length of hospital stay after removal of the foreign body were significantly associated when adjusted for age, sex, type of foreign body and mouth sweep maneuver as a rescue measure. Our findings are relevant because they highlight the importance of early care, timely diagnosis and early management of pediatric patients.
Keywords: Respiratory Aspiration; Airway Management; Pediatrics; Hospitalization; Peru
Motivation for the study. Foreign body aspiration in pediatric patients is an emergency, and its possible complications can be avoided by timely and adequate management.
Main findings. Patients with more than 48 hours between foreign body aspiration and bronchoscopy have approximately three times the risk of late discharge from the hospital. The most frequent location was the right bronchial tree, with predominance of male sex, organic material as foreign body and mean age of 2.4 years.
Implications. This study allows us to recognize the importance of promoting timely care and diagnosis, allowing early management of pediatric patients with foreign body aspiration.
Keywords: Respiratory Aspiration; Airway Management; Pediatrics; Hospitalization; Peru
INTRODUCTION
Foreign body ingestion or aspiration is one of the most common emergencies in pediatric patients 1. Severity depends on factors such as the type of the object: organic such as insects or seeds or inorganic such as toys, metal objects, plastics, etc., as well as the location and the time from aspiration to removal of the foreign body 2. Foreign body aspiration is a frequent cause of morbidity and mortality in children, and it was the cause of 160 deaths and more than 17 thousand emergency department visits in children under 14 years of age in the United States during the year 2000 3. In Spain, the incidence rate peaks at the first two years of life 4. A study in Brazil reported that 50% of cases occur between the first and third year of life, mostly in males 5. Furthermore, this same study showed that most children under three years of age aspirated organic foreign bodies (86%) while those older than three years of age aspirated inorganic foreign bodies more frequently (75%) 5. Similarly, a study in Switzerland reported that 68.3% of patients were between 1 and 3 years old, and 60% presented symptoms in the last 24 hours 6.
The time of removal of the foreign body obstructing the patient’s airway is one of the most important factors to be evaluated 2,7. An article carried out in China 7 described a correlation between the retention time of the foreign body in the airway and the length of hospital stay (r= 0.189; p<0.001), which implies that the longer the removal time, the longer the hospital stay. However, a study by Hidaka et al. showed that there is no association between the time interval from the aspiration episode to the extraction bronchoscopy and a prolonged hospital stay 8.
In Peru, foreign bodies in tracheal and bronchial airways can be extracted by fibrobronchoscopy (flexible bronchoscopy) or rigid bronchoscopy, performed by a physician with experience in pediatric airway management 9 and familiar with pediatric endoscopic equipment. However, the scarcity of human resources (pediatric pulmonologist), materials and infrastructure; added to the characteristics of our referral system 10 represent important limitations in the care of this condition. This medical emergency requires specialized, timely and effective management, since the presence of complications increases as long as the foreign body remains in the airways 2,9. Therefore, this study aimed to determine the association between the time of illness prior to extraction and post-extraction hospital stay.
MATERIALS AND METHODS
Study design and population
This was a retrospective cohort study. The study population were pediatric patients of the Pediatric Emergency Hospital (HEP) of Lima, Peru. We considered everyone younger than 18 years of age according to the definition of pediatric population by the World Health Organization (WHO) 11.
The HEP has been recognized since 2005 as a category III-1 healthcare center and is one of the main centers specialized in the management of pediatric emergencies and urgencies, such as the removal of foreign bodies from the airway 12.
Inclusion criteria
We considered all patients between 0 and 18 years old, who were discharged with the diagnosis code T17 (foreign body in airway) from the International Classification of Diseases 10th (ICD-10), who underwent bronchoscopy (rigid or flexible) and were attended between 2014 and 2019 in the HEP.
Exclusion criteria
Patients with a foreign body located in places other than the larynx, trachea or right or left bronchial tree and those in which the time of illness was longer than 18 days were excluded, considering that longer times would not be pediatric emergencies 13. Patients with absence of foreign bodies and medical records that did not comply with adequate filling were also excluded.
Sample size calculation
We used the article by Tomaske et al. 6 to calculate the sample size. The aforementioned study found that patients who had a time of illness greater than 24 hours (exposed) had a risk of late discharge of 40% and the risk of those who had a time of illness less than 24 hours (unexposed) was 29.1%. We considered the unexposed/exposed ratio of 0.60. With these values, we calculated the sample size in the EPIDAT ® version 4.2 program (Xunta de Galicia, GAL, ESP), obtaining an initial sample size of 183 patients.
Data Collection
Data were obtained by reviewing the medical records of pediatric patients at the HEP. Data collection was performed by requesting permission from the HEP Research and Teaching area. We requested all records that included patients with diagnosis, management and discharge of the patient, in order to identify all patients with a diagnosis of foreign body in the airway. Data collection was performed by two authors (EAHJ and AKL) using a data collection form, which was used to extract all variables included in the study.
Variables
The time of illness prior to bronchoscopy, defined as the time elapsed since the aspiration of the foreign body, was considered as the independent variable. This variable was categorized into two groups (0 to ≤2 days and >2 days) 14. The dependent variable was post-bronchoscopy discharge time, defined as the time elapsed from foreign body removal to patient discharge, and was categorized as early discharge, when it occurred before or at 24 hours, and as late discharge, when it occurred after 24 hours 15.
The covariables were sociodemographic characteristics such as sex (male or female), age (years), origin (Lima or province), previous hospitalization and type of patient (direct or referred). In addition, we considered clinical findings (cough, wheezing, decreased vesicular murmur, abnormal findings on chest X-ray), and rescue maneuvers outside the health facility (mouth sweep, Heimlich maneuver and tracheotomy) 10. Among the characteristics of the bronchoscopy, we considered the location of the foreign body (trachea, right bronchial tree, left bronchial tree or larynx) 6, the type of foreign body (organic and inorganic) 10, the type of bronchoscopy performed for diagnosis (rigid, flexible or both) and extraction (rigid or flexible), as well as the duration of bronchoscopy in minutes (numerical) and the presence of complications (pneumonia, atelectasis, pneumothorax) 10.
Statistical Analysis
We prepared a data base by double digitization in Microsoft Excel 2019 ® (Microsoft Corporation, CA, USA) which was exported to the statistical package STATA 16 ® (Stata Corporation, College Station, Texas, USA). The database was cleaned and incomplete medical records were eliminated for the main and secondary variables of interest.
For the descriptive analysis, we evaluated the numerical variables using the Shapiro Wilk test to verify whether or not they presented a normal distribution. Thus, we proceeded to describe the numerical variables: age and duration of extraction bronchoscopy using medians and interquartile ranges (IQR) because neither of the two variables had normal distribution. Frequencies and percentages were used to describe the categorical variables. Fisher’s exact test was used during the bivariate analysis to determine the difference between the proportions of the categorical variables and the dependent variable, while the Mann-Whitney U test was used for the numerical variables. A p<0.05 value was considered statistically significant.
The Poisson regression model was used during the multivariate analysis to calculate the relative risk (RR) and their respective 95% confidence intervals (CI). We calculated a model adjusted for the following variables: age, gender, type of foreign body and mouth sweep as a rescue maneuver. This last variable was included by statistical criterion. The type of foreign body was considered as a possible confounding variable despite not obtaining a statistically significant value in our study, by virtue of its epidemiological criterion 16.
Ethical Aspects
The study protocol was submitted to the Ethics Committee of the Universidad Peruana de Ciencias Aplicadas and the Teaching and Research Support Office of the Hospital de Emergencias Pediátricas (code FSC-CEI/55-10-20), and data collection only took place when approval was obtained from both entities. No interventions were performed on the study subjects, nor were patients’ personal identification data included. The clinical data collected for our study were entered into a database, to which only the principal researchers had access.
RESULTS
We reviewed 324 medical records of pediatric patients diagnosed with foreign bodies in the airway. These patients underwent extraction by fibrobronchoscopy and/or rigid bronchoscopy at the HEP in the city of Lima, Peru. Of these 324 medical records, 141 were excluded and 183 histories were included in the study (Figure 1).
Of the total number of pediatric patients included in the study, we found that according to their sociodemographic characteristics, 120 (65.6%) patients were male, with a median age of 2.4 years (IQR: 1.3-7). Most patients (80.3%) attended HEP by referral (Table 1). The most frequent symptom, among the clinical and management variables of the patient with a diagnosis of foreign body, was cough (73.2%). Finally, the most frequently used rescue maneuver prior to extraction was sweeping the mouth with the finger (37.2%) (Table 1).
Table 1 Sociodemographic, clinical and intervention characteristics prior to management and treatment of pediatric patients diagnosed with airway foreign body (n=183 patients).
| Characteristics | n | % |
|---|---|---|
| Sex | ||
| Male | 120 | 65.6 |
| Female | 63 | 34.4 |
| Age (years)a | 2,4 | 1.3-7 |
| Origin | ||
| Lima | 65 | 35.5 |
| Provinces | 118 | 64.5 |
| Type of patient | ||
| Direct | 36 | 19.7 |
| Referred | 147 | 80.3 |
| Previous hospitalization | ||
| Yes | 33 | 18.0 |
| No | 150 | 82.0 |
| Clinical findings | ||
| Cough | ||
| Yes | 134 | 73.2 |
| No | 49 | 26.8 |
| Wheezing | ||
| Yes | 53 | 29.0 |
| No | 130 | 71.0 |
| Diminished vesicular murmur | ||
| Yes | 99 | 54.1 |
| No | 84 | 45.9 |
| Chest X-ray | ||
| Normal | 66 | 35.7 |
| Abnormal | 117 | 64.3 |
| Rescue maneuvers outside the facility | ||
| Mouth sweep | ||
| Yes | 68 | 37.2 |
| No | 115 | 62.8 |
| Heimlich maneuver | ||
| Yes | 5 | 2.7 |
| No | 178 | 97.3 |
| Tracheotomy | ||
| Yes | 1 | 0.6 |
| No | 182 | 99.4 |
a Median and interquartile range.
According to the characteristics of the bronchoscopy performed on pediatric patients with a diagnosis of foreign body in the airways, we found that most patients had an illness time prior to bronchoscopy of less than or equal to two days (56.8%). Likewise, the most frequent location of the foreign body was the right bronchial tree (46.6%). The most frequent type of bronchoscopy was flexible bronchoscopy, as the initial technique (53.0%) and as the procedure that removed the foreign body (54.1%). The duration of bronchoscopy had a median of 20 minutes (IQR: 15-30) (Table 2).
Table 2 Bronchoscopy characteristics of pediatric patients (n=183 patients).
| Characteristics | n | % |
|---|---|---|
| Time of illness prior to bronchoscopy | ||
| 0 to 2 days | 104 | 56.8 |
| > 2 days | 79 | 43.2 |
| Location of the foreign body | ||
| Trachea | 27 | 14.8 |
| Right bronchial tree | 78 | 42.6 |
| Left bronchial tree | 52 | 28.4 |
| Larynx | 26 | 14.2 |
| Performed bronchoscopy | ||
| Rigid bronchoscope | 8 | 4.4 |
| Flexible bronchoscope | 97 | 53.0 |
| Both | 78 | 42.6 |
| Extraction bronchoscope | ||
| Rigid bronchoscope | 84 | 45.9 |
| Flexible bronchoscope | 99 | 54.1 |
| Duration of bronchoscopy (in minutes)a | 20 | 15-30 |
a Median and interquartile range.
Regarding the characteristics of the pediatric patients after foreign body removal, most (72.7%) were discharged early (before or equal to 24 hours). The predominant type of foreign body in pediatric patients was organic material (59.6%). As for complications, the most frequent was pneumonia (24.6%), followed by atelectasis (18.0%) and pneumothorax (1.6%), this being the least frequent complication (Table 3).
Table 3 Characteristics of pediatric patients after foreign body removal (n=183 patients).
| Characteristics | n | % |
|---|---|---|
| Post-bronchoscopy discharge time | ||
| Early discharge (≤24 hours) | 133 | 72.7 |
| Late discharge (>24 hours) | 50 | 27.3 |
| Type of foreign body | ||
| Organic | 109 | 59.6 |
| Inorganic | 74 | 40.4 |
| Complications | ||
| Pneumonia | ||
| Yes | 45 | 24.6 |
| No | 138 | 75.4 |
| Atelectasis | ||
| Yes | 33 | 18.0 |
| No | 150 | 82.0 |
| Pneumothorax | ||
| Yes | 3 | 1.6 |
| No | 180 | 98.4 |
We found no differences between median patient age and post-extraction hospitalization time during bivariate analysis. Likewise, there were no differences between the proportions of previous hospitalization of patients with post-extraction hospitalization time. However, differences were found between the proportions of finger sweeping of the mouth as a rescue maneuver and post-extraction hospitalization time (Table 4). Additionally, differences were also found between the proportions of pre-bronchoscopy sick time and post-bronchoscopy discharge time (p<0.001). Finally, differences were found as well between the proportions of the occurrence of pneumonia and post-extraction hospitalization time (p<0.001) (Table 5).
Table 4 Contrast of sociodemographic and clinical variables with the length of time the patient remained in the health center after extraction (n=183 patients).
| Characteristics | Early discharge (≤24 hours) (n = 133) | Late discharge (>24 hours) (n = 50) | p-value | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Sex | |||||
| Male | 90 | 75.0 | 30 | 25.0 | 0.384 |
| Female | 43 | 68.3 | 20 | 31.7 | |
| Age (years)a | 2,6 | 1.3-7.3 | 2,1 | 1.1-5.8 | 0.931b |
| Origin | |||||
| Lima | 53 | 81.5 | 12 | 18.5 | 0.057 |
| Provinces | 80 | 67.8 | 38 | 32.2 | |
| Type of patient | |||||
| Direct | 28 | 77.8 | 8 | 22.2 | 0.534 |
| Referred | 105 | 71.4 | 42 | 28.6 | |
| Previous hospitalization | |||||
| Yes | 20 | 60.6 | 13 | 39.4 | 0.129 |
| No | 113 | 75.3 | 37 | 24.7 | |
| Clinical findings | |||||
| Cough | |||||
| Yes | 96 | 71.6 | 38 | 28.4 | 0.709 |
| No | 37 | 75.5 | 12 | 24.5 | |
| Wheezing | |||||
| Yes | 38 | 71.7 | 15 | 28.3 | 0.856 |
| No | 95 | 73.1 | 35 | 26.9 | |
| Diminished vesicular murmur | |||||
| Yes | 67 | 67.7 | 32 | 32.3 | 0.134 |
| No | 66 | 78.6 | 18 | 21.4 | |
| Chest X-ray | |||||
| Normal | 54 | 83.1 | 11 | 16.9 | 0.024 |
| Anormal | 78 | 66.7 | 39 | 33.3 | |
| Rescue maneuvers outside the facility | |||||
| Mouth sweep | |||||
| Yes | 56 | 82.0 | 12 | 17.7 | 0.026 |
| No | 77 | 67.0 | 38 | 33.0 | |
| Heimlich maneuver | |||||
| Yes | 2 | 40.0 | 3 | 60.0 | 0.127 |
| No | 131 | 73.6 | 47 | 26.4 | |
| Tracheotomy | |||||
| Yes | 0 | 0.0 | 1 | 100.0 | 0.273 |
| No | 133 | 73.1 | 49 | 26.9 | |
a Median and interquartile range; b p-value calculated using the Mann-Whitney U test.
Table 5 Contrast of bronchoscopy variables and pediatric patient complications with the length of hospital stay after foreign body removal (n=183 patients).
| Characteristics | Early discharge (≤24 hours) (n = 133) | Late discharge (>24 hours) (n = 50) | p-value | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Time of illness prior to bronchoscopy | |||||
| 0 to 2 days | 84 | 85.6 | 15 | 14.4 | 0.001 |
| > 2 days | 44 | 55.7 | 35 | 44.3 | |
| Location of the foreign body | |||||
| Trachea | 21 | 77.8 | 6 | 22.2 | 0.941 |
| Right bronchial tree | 56 | 71.8 | 22 | 28.2 | |
| Left bronchial tree | 37 | 71.2 | 15 | 28.9 | |
| Larynx | 19 | 73.1 | 7 | 26.9 | |
| Type of foreign body | |||||
| Organic | 77 | 70.6 | 32 | 29.4 | 0.502 |
| Inorganic | 56 | 75.7 | 18 | 24.3 | |
| Performed bronchoscopy | |||||
| Rigid bronchoscope | 8 | 100.0 | 0 | 0.0 | 0.124 |
| Flexible bronchoscope | 72 | 74.2 | 25 | 25.8 | |
| Both | 53 | 68.0 | 25 | 32.0 | |
| Extraction bronchoscope | |||||
| Rigid bronchoscope | 59 | 70.2 | 25 | 29.8 | 0.510 |
| Flexible bronchoscope | 74 | 74.8 | 25 | 25.2 | |
| Duration of bronchoscopy (in minutes) a | 20 | 15-30 | 25 | 15-35 | 0.169 b |
| Complications | |||||
| Pneumonia | |||||
| Yes | 13 | 28.9 | 32 | 71.1 | 0.001 |
| No | 120 | 87.0 | 18 | 12.0 | |
| Atelectasis | |||||
| Yes | 19 | 57.6 | 14 | 42.4 | 0.050 |
| No | 114 | 76.0 | 38 | 240 | |
| Pneumothorax | |||||
| Yes | 2 | 66.7 | 1 | 33.3 | 1.000 |
| No | 131 | 72.8 | 49 | 27.3 | |
a Median and interquartile range; b p-value calculated using the Mann-Whitney U test.
During the multivariate analysis, the model adjusted for the variables age, sex, type of foreign body and mouth sweeping technique showed that the risk of having late discharge increases by 2.94 times (95% CI: 1.72-5.01; p=0.001) in those patients with more than 48 hours of sick time prior to extraction bronchoscopy (Table 6).
Table 6 Crude and adjusted regression analysis for hospitalization time greater than 24 hours post foreign body removal in pediatric patients at the Pediatric Emergency Hospital (n=183 patients).
| Characteristics | Crude analysis | Adjusted analysis a | ||
|---|---|---|---|---|
| RR (95% CI) | p-value | RR (95% CI) | p-value | |
| Time of illness prior to bronchoscopy | ||||
| 0 to 2 days | Ref. | Ref. | ||
| >2 days | 3.07 (1.81-5.22) | 0.001 | 2.94 (1.72-5.01) | 0.001 |
RR: relative risk; CI: confidence interval.
a Adjusted for age, gender, type of foreign body and mouth sweep.
DISCUSSION
The most frequent location was in the right bronchial tree and the most frequent type of foreign body was organic materials among all 183 included patients. We found that 72.7% of patients were discharged before 24 hours. Our main finding was the association between the time of illness prior to bronchoscopy greater than two days and late discharge.
The moment of aspiration usually occurs while eating or playing, usually under adult supervision 17, which corresponds to the high exposure to new stimuli and foods at early ages, with organic objects being the most frequent 18, particularly food 19. This finding is consistent with another study by Bing Zhong et al. 16. Particularly, in our study, 59.6% of the foreign bodies removed were organic. This finding is relevant when considering that the type of foreign body is associated with the length of hospital stay 8, and that different types of foreign bodies can be associated with different types of injuries, for example, organic bodies are associated with upper respiratory tract injury 20.
Our study shows an association between the time of illness prior to bronchoscopy and the time of hospitalization after foreign body extraction. However, the study by Hidaka et al. 8, found no association between the variables of interest; they described that 74% of the cases underwent removal within two days of foreign body aspiration, while in our study only 53.8% of the cases underwent removal within two days of foreign body aspiration. This difference would indicate that in other contexts such as Japan, the diagnosis and removal of the foreign body is performed in less time compared to our context, thus reducing the risk of complications and hospitalization time. Thus, our findings could be explained by the problems of the medical referral system in Peru and the low availability of specialists 10. Likewise, the study by Hidaka et al. describes a low prevalence of foreign body aspiration in Japan 8, since they only found 77 cases of foreign body aspiration during the 23 years they evaluated (from 1988 to 2011). In contrast, our study considered a time interval of only six years (from 2014 to 2019), finding more than 183 cases. Therefore, these differences could lead to dissimilar results between the two studies.
However, several studies found an association between the time of illness and the time of post-extraction hospitalization 7,21. For example, a study conducted in China 7, reported a correlation between the time of foreign body retention in the airway and the time of hospitalization. Although this correlation was low (r=0.189), it was statistically significant (p<0.001). In our study, 56.8% of the participants had an illness time prior to bronchoscopy less than or equal to two days, a result similar to that reported in the study conducted in Chinese population, where 68.5% had a time of three days or less, which would mean that both studies found a relationship between both variables. However, it was not possible for the authors of the Chinese study to establish a cut-off point for the time of illness prior to bronchoscopy, as they considered this variable to be numerical. Additionally, another study performed in Spanish pediatric population showed a similar result to ours, where the authors report that there was a significant association between diagnostic delay and the appearance of long-term complications, without addressing intraoperative adverse events 21.
Prolonged illness prior to bronchoscopy doubles the risk of post-extraction hospitalization. Although asphyxia and cardiorespiratory arrest are more frequent shortly after aspiration, they can also occur in later days 22. Late diagnosis is frequently associated with atelectasis, lung abscesses and increased morbidity and mortality 22-24, due to inflammation occurring at the lower airway level 16. In fact, medical literature describes that foreign body aspiration causes inflammation in the airway, which prolongs pulmonary recovery time 25. The importance of this finding is evidenced in a study by Man Ki Chung et al. where they describe an association between inflammatory findings in the airway prior to foreign body removal and delayed pulmonary recovery 25. This fact can cause the need for extended hospitalization, which in turn, results in a higher risk of acquiring nosocomial infections 26.
The diagnostic or therapeutic delay can be explained by causes associated with the physician, resources, parents or uninformative medical records 20. Regarding the medical records, the condition may occur even without a history of choking or asphyxia in the pediatric population 27. For this reason, our results highlight the importance of timely management and correct evaluation of patients within the first 48 hours. As a complement, in order to ensure timely management and improve prognosis, it is recommended to train child caregivers, streamline referral systems and strengthen programs on the use of rigid and flexible bronchoscopy in pediatric patients. Therefore, in line with our findings, priority should be given to the availability of trained professionals and sufficient resources in health centers for the timely management of pediatric patients with foreign body aspiration, which would reduce complications and improve the prognosis of these patients.
This study has limitations. Patient evolution after discharge from HEP was not evaluated due to the nature of the study design. Although we only evaluated the data from the medical records, post-extraction complications are infrequent 18,21,27,28 and if they had occurred, the patient would have opted to return. Since the data were collected manually by means of a data collection form, information bias may have occurred. In addition, we did not include other variables relevant to this study, such as the activity that the patient was performing at the time of aspiration, since this information is usually not recorded in the medical records. Regarding external validity, since the data were obtained from a single hospital, our results cannot be extrapolated to different populations. However, it should be considered that HEP is one of the main referral institutions for pediatric patients in Lima, Peru, which allows us to determine the association of interest in an exploratory manner. Finally, there is no standardization of the main variables (time of discharge and time of illness prior to bronchoscopy). Nevertheless, our research uses cut-off points described in similar studies 14,15.
According to our results, most foreign body aspiration cases occurred in boys younger than three years old. In addition, patients with an illness time longer than two days between foreign body aspiration and bronchoscopy had 2.94 higher risk of a prolonged hospital stay (more than 24 hours) when adjusting for age, sex, type of foreign body and mouth sweep as a rescue maneuver.
REFERENCES
1. Sjogren PP, Mills TJ, Pollak AD, Muntz HR, Meier JD, Grimmer JF. Predictors of complicated airway foreign body extraction. Laryngoscope. 2018;128(2):490-5. doi: 10.1002/lary.26814. [ Links ]
2. Joao AB, Bueno FG. Foreign body aspiration in children. Pediatric Respiratory Reviews. 2002;3(4):303-7. doi: 10.1016/S1526-0542(02)00265-8. [ Links ]
3. Yanowsky-Reyes G, Aguirre-Jauregui OM, Trujillo Ponce SA, Rodriguez Franco E, Monroy Martín Y, Pérez Liñán JA, et al. Ingestión de sustencias químicas en esófago, análisis de las complciaciones tempranas y tardias en el manejo de los mismos, una revisión de 70 casos. iMedPub. 2013;9(2):1-7. doi: 10.3823/092. [ Links ]
4. Gómez Cervantes M, de la Torre Ramos CA, Jiménez Gómez J, Encinas Hernández JL, Hernández Oliveros F, Dore Reyes M, et al. Sospecha de aspiración de cuerpos extraños en pacientes pediátricos: Nuestra experiencia en 10 años. Cir Pediatr. 2018;31(2):81-4. [ Links ]
5. Cassol V, Marques Pereira A, Zorxela L, Michelin Becker M, Menna Barreto SS. Foreign body in children-s airways. J Pneumologia. 2003;29(3):139-44. doi: 10.1590/S0102-358620030000300005. [ Links ]
6. Tomaske M, Gerber AC, Weiss M. Anesthesia and periinterventional morbidity of rigid bronchoscopy for tracheobronchial foreign body diagnosis and removal. Paediatr Anaesth. 2006;16(2):123-9. doi: 10.1111/j.1460-9592.2005.01714.x. [ Links ]
7. Xu Y, Ren HB, Jiang L, Wang SF, Feng RL, Li Q. Analysis of related factors for the retention time of tracheobronchial foreign bodies in pediatrics. J Surg Res. 2019;233(72):262-7. doi: 10.1016/j.jss.2018.08.024. [ Links ]
8. Hidaka H, Obara T, Kuriyama S, Kurosawa S, Katori Y, Kobayashi T. Logistic regression analysis of risk factors for prolonged pulmonary recovery in children from aspirated foreign body. Int J Pediatr Otorhinolaryngol. 2013;77(10):1677-82. doi: 10.1016/j.ijporl/2013.07.024. [ Links ]
9. Suzen A, Karakus SC, Erturk N. The role of flexible bronchoscopy accomplished through a laryngeal mask airway in the treatment of tracheobronchial foreign bodies in children. Int J Pediatr Otorhinolaryngol. 2019;117:194-7. doi: 10.1016/j.ijporl.2018.12.006. [ Links ]
10. Llanos Zavalaga L, Orellana Vasquez A, Aguado Taquire HF. Evaluación inicial del Sistena de Referencia y Contrareferencia ambulatoria en la DIRIS Lima Norte. Rev Med Hered. 2021;32(2):91-102. doi: 10.20453/rmvh.v32i3.3982. [ Links ]
11. Organización Mundial de la Salud. Módulos Nuevos [Internet]. OMS; 2018 [citado el 5 de septiembre de 2023]. Disponible en: https://www.paho.org/es/documentos/oms-programa-orientacion-salud-adolescente-para-proveedores-salud. [ Links ]
12. Hospital de Emergencias Pediátricas [Internet]. Lima: HEP; 2023 [citado el 5 de septiembre de 2023]. Disponible en: http://www.hep.gob.pe. [ Links ]
13. Liu B, Ding F, An Y, Li Y, Pan Z, Wang G, et al. Occult foreign body aspirations in pediatric patients: 20-years of experience. BMC Pulm Med. 2020;20(1):320. doi: 10.1186/s12890-020-01356-8. [ Links ]
14. Chung MK, Jeong HS, Ahn KM, Park SH, Cho JK, Son YI, et al. Pulmonary recovery after rigid bronchoscopic retrieval of airway foreign body. Laryngoscope. 2007;117(2):303-7. doi: 10.1097/01.mlg.0000250788.93900.ef. [ Links ]
15. Cevik M, Gókdemir MT, Boleken ME, Sogut O, Kurkcuoglu C. The characteristics and outcomes of foreign body ingestion and aspiration in children due to lodged foreign body in the aerodigestive tract. Pediatr Emerg Care. 2013;29(1):53-7. doi: 10.1097/PEC.0b013e31827b5374. [ Links ]
16. Zhong B, Sun SL, Du JT, Deng D, Liu F, Liu YF, et al. Risk factors for lower respiratory tract infection in children with tracheobronchial foreign body aspiration. Medicine (Baltimore). 2019;98(10):e14655. doi:10.1097/MD.0000000000014655. [ Links ]
17. Göktas O, Snidero S, Jahnke V, Passali D, Gregori D. Foreign body aspiration in children: Field report of a German hospital. Pediatr Int. 2010;52:100-3. doi: 10.1111.j.1442-200X.2009.02913.x. [ Links ]
18. Boufersaoui A, Smati L, Benhalla KN, Boukari R, Smail S, Anik K, et al. Foreign body aspiration in children: Experience from 2624 patients. Int J Pediatr Otorhinolaryngol. 2014;77(10):1683-8. doi: 10.1016/j/ijporl/2013.07.026. [ Links ]
19. Shlizerman L, Mazzawi S, Rakover Y, Ashkenazi D. Foreign body aspiration in children: the effects of delayed diagnosis. Am J Otolaryngol. 2010; 31:320-24. doi: 10.1016/j.amjoto/2009.03.007. [ Links ]
20. He S, Zuo ZL. Different anatomical sites of the foreign body injury with 2999 children during 2012-2016. Chin J Traumatol. 2018;21(6):333-337. doi: 10.1016/j.cjtee.2018.07.004. [ Links ]
21. Antón-Pacheco JL, Martín-Alelú R, López M, Morante R, Merino-Mateo L, Barrero S, et al. Foreign body aspiration in children: Treatment timing and related complications. Int J Pediatr Otorhinolaryngol. 2021;15(5) 144:110690. doi: 10.1016/j.ijporl.2021.110690. [ Links ]
22. Pan H, Lu Y, Shi L, Pan X, Li L, Wu Z. Similarities and differences in aspirated tracheobronchial foreign bodies in patients under the age of 3 years. Int J Pediatr Otorhinolaryngol. 2012;16(4):911-4. doi: 10.1016/j.ijporl/2012.02.002. [ Links ]
23. Cutorone C, Pedruzzi B, Tava G, Emanuelli E, Barion U, Fischetto D, et al. The complimentary role of diagnostic and therapeutic endoscopy in foreign body aspiration in children. Int J Ped Otorhinolaryngol. 2012;75(12):1481-5. doi: 10.1016/j/ijporl/2011.08.014. [ Links ]
24. Sih T, Bunnag C, Ballali S, Lauriello M, Bellussi L. Nuts and seed: a natural yet dangerous foreign body. Int J Pediatr Otorhinolaryngol. 2012;14(76):S49-52. doi: 10.1016/j.ijporl.2012.02.012. [ Links ]
25. Chung MK, Jeong HS, Ahn KM, Park SH, Cho JK, Son YI, et al. Pulmonary recovery after rigid bronchoscopic retrieval of airway foreign body. Laryngoscope. 2007;117(2):303-7. doi: 10.1097/01.mlg.0000250788.93900.ef. [ Links ]
26. Nguyen DK, Friedlander S, Fleischman RJ, Zangwill KM. Length of Stay and Complications Associated with Febrile Infants <90 Days of Age Hospitalized in the United States, 2000-2012. Hosp Pediatr. 2018;8(12):746-752. doi: 10.1542/hpeds.2018-0132. [ Links ]
27. Rance A, Mittaine M, Michelet M, Martin Blondel A, Labouret G. Delayed diagnosis of foreign body aspiration in children. Arch Pediatr. 2022;29(6):424-428. doi: 10.1016/j.arcped.2022.05.006. [ Links ]
28. Johnson K, Linnaus M, Notrica D. Airway foreign bodies in pediatric patients: anatomic location of foreign body affects complications and outcomes. Pediatr Surg Int. 2017;33(1):59-64. doi: 10.1007/s00383-016-3988-9. [ Links ]
Cite as: Huarhua Jimenez EA, Kruchinsky Lozada A, Galdos-Bejar M, Carreazo NY. Association between pre-bronchoscopy time of illness and post-bronchoscopy discharge time in pediatric patients with foreign body aspiration: retrospective cohort study in a Peruvian referral center, 2014-2019. Rev Peru Med Exp Salud Publica. 2023;40(4):423-31. doi: 10.17843/rpmesp.2023.404.12977.
Received: June 14, 2023; Accepted: November 15, 2023











 texto en
texto en