Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Horizonte Médico (Lima)
versão impressa ISSN 1727-558X
Horiz. Med. vol.23 no.2 Lima abr./jun. 2023 Epub 30-Maio-2023
http://dx.doi.org/10.24265/horizmed.2023.v23n2.04
Original article
Functionality of lower limb with exposed bone using VAC® negative pressure wound therapy vs. medial calf flap
1 Sociedad Peruana de Cirugía Plástica Reconstructiva (Peruvian Society of Plastic, Reconstructive and Aesthetic Surgery), full member. Lima, Peru.
2 Clínica Stella Maris. Lima, Peru.
Objective:
To compare two reconstructive surgery techniques for lower limb injury with exposed bone and demonstrate that the VAC® (vacuum-assisted closure) negative pressure wound therapy is an alternative for potential recovery showing no significant changes that could lead to functional compromise.
Materials and methods:
An analytical, prospective, quantitative and longitudinal study conducted with all the patients of Clínica Stella Maris with traumatic injuries of the lower limb and exposure of the middle third of the tibia treated with the VAC® system and the medial calf flap in 2019.
Results:
The measurement obtained with the functional ambulation categories (FAC) scale showed better results among the patients treated with the VAC® technique (since 50 % got grade V) than those who underwent the flap technique (50 % got grade IV), being the differences statistically significant (p < 0.05). It was observed that the time to closure was longer with the VAC® technique due to the progressive regeneration process consisting of the complete filling or coverage of the lesion area. On the other hand, the difference in the postoperative pain intensity between the two techniques was evident, being moderate to severe with the flap technique and mild, for the most part, with the VAC® technique.
Conclusions:
The VAC® suction system is effective for bone coverage in traumatic defects of the anterior middle third of the tibia. It is an alternative for potential recovery that does not change the anatomical structures because it provides better functional results and fewer complications. It is a useful and safe option that stimulates wound closure and minimizes the need for surgical treatment.
Keywords: Wound Healing; Lower Extremity; Rehabilitation; Therapeutics
Introduction
Nowadays, many work activities involving multiple risks are carried out, which leads to an increase in the number of accidents such as lower limb injuries with exposed bone, among others. These accidents frequently cause traumatic injuries that can worsen in some cases since there are no soft tissues—such as muscles—that protect the pretibial surface, as in the posterior compartments of the leg. Therefore, the recovery or regeneration of tissues in this area may be slow, which demands and prolongs healing time, involving the potential risk of infection due to the exposed bone surface 1,2.
In order to recover the function of the affected area, there are different surgical techniques to cover the exposed lower limb bone that end up in long recovery processes with variable grade of functional limitation, which even lead to temporary or permanent disability of the affected extremity.
There is a therapeutic possibility of lower risk of infection since it is a closed vacuum system: the VAC® technique achieves motor recovery without muscle structure displacements that may cause temporary or permanent functional limitation because it provides coverage in the event of soft tissue loss with pretibial exposed bone 3-5. The negative pressure wound therapy (NPWT) is a mechanical treatment used as an adjuvant in wound healing. It can be administered in a continuous or intermittent basis, for both acute and chronic lesions, and is an alternative to the traditional healing methods since it is quick, effective and easy to use 6-8.
The VAC® technique prepares the wound bed for closure, reduces edema, promotes granulation tissue formation, reduces the bacterial load, keeps hydration (by removing exudate and reducing the bruise surface area), improves healing rates and reduces the hospital stay. The technique is carried out by placing a dressing—which can be of gaze or polyurethane foam—in the injury, sealing it with a semiocclusive dressing and applying subatmospheric pressure through a drainage tube connected to a computerized pump, which is useful to promote wound healing 9-12.
Several international studies on the VAC® technique conducted in the last twenty years satisfactorily agree with the results obtained with NPWT, a technique that is more frequently used in private hospitals 16. Clinical cases with complicated lesions were successfully treated with this method in complex areas of exposed tissue—particularly the lower extremities—with good functional results, which allowed patients to return to their daily activities in less time and without secondary complications compared to other treatments that cause functionality problems 13-15.
De Juan Pérez, in his study conducted in 2010, used the VAC® therapy in lower limb complex trauma, resulting in the reduction of infection and acceleration of lesion granulation, which helped to improve the prognosis of risk of lower limb amputation and be of benefit to serious open fractures 1.
Materials and methods
Study design and population
Out of all the patients with traumatic lower limb injuries with exposure of the medial third of the tibia treated at Clínica Stella Maris during 2019, ten were treated with the VAC® technique and eight with the medial calf flap technique. The study sample consisted of 18 patients, with ages that ranged between 19 and 65 years, most of whom were males. The research included patients diagnosed with traumatic lower limb injuries with exposed bone and without osteomyelitis.
Medical records were used as study tool, and the data thereof were included in a data collection sheet created for that purpose. Said sheet consisted of the demographic characteristics of the patients such as age and sex, percent distribution of insurance type by technique, time of treatment administration, presence of infection, complications and adverse effects, as well as the functionality of lower limbs assessed with the functional ambulation categories (FAC) test, a questionnaire about the ability to perform daily activities. Patients were evaluated by a third party to avoid bias.
The functional assessment was conducted using the FAC test, designed to evaluate the patients’ ambulation ability, determine their progression and establish the treatment guidelines. The test score is as follows:
Score 0 (no ambulation): patients cannot walk, even with external assistance.
Score 1 (basic ambulation): patients are dependent ambulators who require permanent assistance from another person.
Score 2 (ambulation at home): patients are able to walk only indoors on level and horizontal surfaces, generally within a known and controlled area like home.
Score 3 (ambulation in home surroundings): patients are able to walk both indoors and outdoors on irregular surfaces and go up an occasional step or stairs.
Score 4 (independent ambulation in the community): patients are able to walk on all kinds of irregular surfaces; they can go up and down stairs, ramps, curbs, etc.
Score 5 (normal ambulation): walking is totally normal regarding distance and surface appearance, both at home and outdoors, with unlimited distance; there is no aesthetic anomaly or lameness 19.
Variables and measurements
This was an observational study since it was limited to the measurement of the study variables by the researcher. According to the scope, this was an analytical study because it demonstrated a relationship between the variables by comparing the functionality of lower limbs through two techniques. Moreover, this was a longitudinal study since the wound closure was followed-up at several times. Regarding the time of data collection, this was a prospective study because it was conducted from the exposure to the techniques to the wound closure.
Statistical analysis
IBM SPSS Statistics V23 was used for data processing; the demographic variables were analyzed using descriptive statistics and the results were shown in a frequency table according to the Vancouver style. The mean and standard deviation of the numerical data and the percentage of the qualitative data were calculated. As statistical test to differentiate ratios, the chi-square test for the comparison of independent ratios at a confidence level of 100 % was used. The Mann-Whitney U test was used to compare changes in the mean values.
Ethical considerations
This research work complied with the ethical principles of respect for individuals, assistance and fairness. The confidentiality of personal data and photographs collected was ensured; likewise, patients confirmed their participation before surgery by signing an informed consent form.
The research had the permission of the clinic’s ethics committee. Permission from the pertinent leadership, i.e., the director and the head of the Plastic Surgery Department of Clínica Stella Maris, was requested to conduct the study.
Results
The results confirmed the objective of the study. The functional grade was evaluated with the VAC® system technique and the medial calf muscle flap coverage technique.
The research was conducted in patients with traumatic lower limb injuries, where vacuum therapy was confirmed as a useful and safe option. The VAC® method is a mechanical closure system that applies sustained negative force to the whole wound, thus avoiding its retraction and promoting the constant reduction of its diameter. This eliminates interstitial fluid, which may contribute to reduce edema. As a result, there is an enhanced blood flow to the wound (Figure 1).
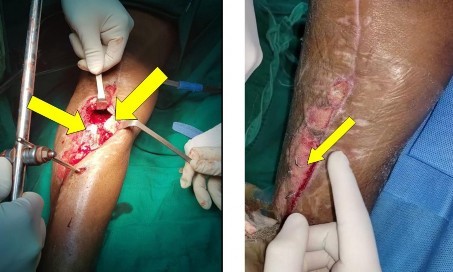
Figure 1 Lower right limb with exposed bone before starting the VAC® technique and (solved) areas with exposed bone covered by granulation tissue after using the vacuum therapy
Source: researcher’s photographs.
The main immediate complications from the two techniques were determined, finding more complications in the patients treated with the flap technique compared to those treated with the VAC® technique (37.5 % and 10 %, respectively); such differences were statistically significant (p < 0.05) (Table 1).
Table 1 Distribution of complications by technique
| Patient | Age - sex | Technique type | Complications |
|---|---|---|---|
| 1 | 30 years - male | VAC® | NO |
| 2 | 19 years - male | VAC® | NO |
| 3 | 31 years - female | VAC® | NO |
| 4 | 37 years - male | VAC® | BLEEDING |
| 5 | 60 years - female | VAC® | NO |
| 6 | 59 years - male | VAC® | NO |
| 7 | 39 years - male | VAC® | NO |
| 8 | 33 years - female | VAC® | NO |
| 9 | 48 years - male | VAC® | NO |
| 10 | 35 years - male | VAC® | NO |
| 1 | 61 years - male | Medial calf flap | NO |
| 2 | 59 years - female | Medial calf flap | NO |
| 3 | 40 years - male | Medial calf flap | BLEEDING |
| 4 | 39 years - male | Medial calf flap | NO |
| 5 | 47 years - male | Medial calf flap | BLEEDING |
| 6 | 33 years - female | Medial calf flap | BLEEDING |
| 7 | 61 years - female | Medial calf flap | INFECTION |
| 8 | 28 years - male | Medial calf flap | NO |
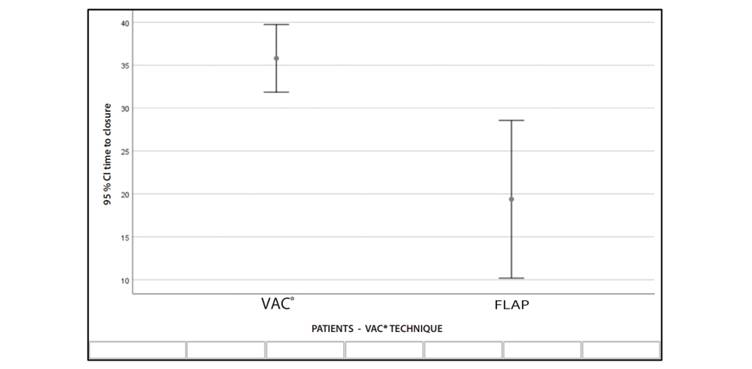
The time to wound closure was longer with the VAC® technique compared to the flap technique, showing significant differences (p < 0.05) (Table 2 and Figure 2).
Table 2 Mann-Whitney U test results
| Variable | Technique | N | Mean | Standard deviation | Z | p |
|---|---|---|---|---|---|---|
| Time to closure in days | VAC® | 10 | 35.80 | 5.514 | 4.14 | 0.01 |
| FLAP | 8 | 19.38 | 10.993 |
Moderate to severe pain was reported: pain was higher in patients who underwent the flap technique compared to those who underwent the VAC® technique (0 % and 100 %, respectively), being the differences statistically significant (p < 0.05) (Table 3).
Table 3 Distribution of pain intensity by technique
| Patients | Technique type | VAS: Pain intensity: Mild (0-3) Moderate (4-6) Severe (7-10) |
|---|---|---|
| 1 | VAC® | MILD 2/10 |
| 2 | VAC® | MILD 2/10 |
| 3 | VAC® | MILD 3/10 |
| 4 | VAC® | MILD 2/10 |
| 5 | VAC® | MILD 1/10 |
| 6 | VAC® | MILD 2/10 |
| 7 | VAC® | MILD 3/10 |
| 8 | VAC® | MILD 1/10 |
| 9 | VAC® | MILD 2/10 |
| 10 | VAC® | MILD 2/10 |
| 1 | Medial calf flap | MODERATE 5/10 |
| 2 | Medial calf flap | MODERATE 4/10 |
| 3 | Medial calf flap | MODERATE 4/10 |
| 4 | Medial calf flap | SEVERE 7/10 |
| 5 | Medial calf flap | MODERATE 4/10 |
| 6 | Medial calf flap | MODERATE 5/10 |
| 7 | Medial calf flap | MODERATE 5/10 |
| 8 | Medial calf flap | MODERATE 4/10 |
The attending physician should periodically examine the wounds treated with the VAC® NPWT. The dressings were changed every 48 to 72 hours: dressing change intervals were established by continuous wound evaluation (Table 4).
Table 4 Number of changes with the VAC® system
| Variable | Technique | N | Mean | Deviation |
|---|---|---|---|---|
| Number of changes | VAC® | 10 | 4.7 | 1.059 |
| Sample | Number of changes with the VAC® technique | |||
| Time to wound closure | ||||
| 1 Patient | 25 days | |||
| 2 Patient | 37 days | |||
| 3 Patient | 37 days | |||
| 4 Patient | 36 days | |||
| 5 Patient | 43 days | |||
| 6 Patient | 31 days | |||
| 7 Patient | 43 days | |||
| 8 Patient | 37 days | |||
| 9 Patient | 36 days | |||
| 10 Patient | 31 days |
The average number of changes with the VAC® technique is 4.70 with a variability of 1.06 changes.
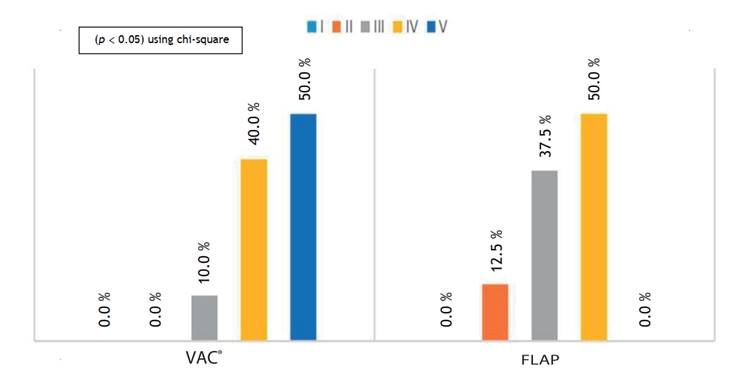
The results of the FAC scale revealed that the patients were satisfied with the VAC® technique, with prevalence of functional grade V (50 %), compared to the medial calf muscle flap coverage technique, which showed a prevalence of functional grade IV (50 %). Statistically significant differences were found in the overall results (p < 0.05) (Figure 3).
Discussion
Regarding the functional grade, the research showed a positive relationship between the coverage of lower limb injuries with exposed bone and the VAC® system technique, which was effective compared with the medial calf muscle flap technique in patients treated at Clínica Stella Maris during 2019 17-19. The results showed the significance of the functional measurement, with higher FAC scale scores, in patients who underwent the VAC® technique.
Our study agrees with the one conducted by BernalMartínez et al. 17 (Mexico), who treated with surgical debridement cases of full-thickness burns with exposed bone that caused coverage defects because of the limited availability of tissues to reconstruct these defects. The results stood out the complete wound closure after the total bone coverage with granulation tissue and subsequent skin graft. Therefore, it is concluded that the vacuum therapy is a useful and safe option that stimulates wound closure and minimizes the need for surgical treatment for full-thickness burns with exposed bone 17-19.
Additionally, De Juan Pérez 1 (Spain) conducted an analytic observational study in order to use the VAC® therapy in case of a serious left leg trauma. The results of NPWT with this system demonstrated that it reduced the risk of infection of serious fractures, which notably accelerated wound granulation. After admission to the hospital, a good granulation tissue over a large part of the surface could be observed since the first VAC® dressing change. This fact significantly improved the appearance and prognosis of risk of leg amputation. If compared with the results of this research, the VAC® system poses a milestone for acute or chronic complex injury treatment since it is an important therapeutic tool to treat serious open fractures of lower limbs. The relationship between the time to closure or coverage and the results shows that the VAC® system technique is effective 20-22.
In 2018, Maitret-Velázquez et al. 29 (Mexico) claimed that NPWT accelerated wound healing, which facilitated intrahospital treatment: pain and function of lower limb injuries were controlled and infections were prevented, which helped wound closure in medically compromised patients. This agrees with the present study on the evaluation of the functional grade using the VAC® system technique. Their study analyzed 93 patients who underwent NPWT. Surgical wound infection and vascular exposure were observed in 40.9 % and 22.6 % of the patients, respectively. NPWT or VAC® system accelerated wound healing, thereby facilitating the intrahospital treatment and controlling pain and infection; such results also agree with the present study and the difference was statistically significant.
In 2020, Goyo et al. 14 (Venezuela) observed the complete clinical improvement of all the characteristics of the wound. Moreover, their analysis also showed acceleration of the healing process, infection control and reduction of hospital stay. This demonstrated that no complications were found with the use of the VAC® system, which agrees with our results.
According to different research studies reviewed and the results of this study, it was possible to analyze and determine that NPWT is a non-invasive treatment that nowadays is included in general surgery. It is used to treat chronic, acute and complex wounds, in order to reduce the number of wound healing procedures and the time required to perform them, as well as avoid surgeries involving an elevated morbidity for the patient. The VAC® system allows reducing the number of weekly wound healing procedures and the time required to perform them, so patients recover their functionality and are able to walk independently during their rehabilitation 23-25.
In conclusion, according to the FAC scale, patients who underwent the VAC® technique showed a better recovery than those who underwent the medial calf muscle flap coverage technique since 50 % of the VAC® group got grade V functionality and 50 % of the flap group got grade IV functionality. The differences were statistically significant in the overall results 26-27. Also, the main immediate complications from the two techniques—i.e., bleeding and infection—were determined, finding more complications in the patients treated with the flap technique compared to those treated with the VAC® technique (37.5 % and 10 %, respectively); such differences were statistically significant 28-29.
On the other hand, the difference in the postoperative pain intensity between the two techniques was evident, being moderate to severe in patients who underwent the flap technique and mostly mild among those who underwent the VAC® technique. The difference was statistically significant (p < 0.05).
Regarding the vacuum therapy, this is a useful and safe option that stimulates wound closure and minimizes the need for wide surgical treatment in wounds with exposed bone. This has a positive impact on patients’ financial situation because it avoids expensive treatments. Moreover, it helps workers to resume their daily and social activities.
The VAC® technique or NPWT is an alternative that should be preferred over the flap technique since the principles of reconstructive surgery include protecting limb motor function, which is one of the most important objectives.
REFERENCES
1. De Juan Perez FJ. Terapia VAC en traumatismo grave de pierna izquierda. Cir plast ibero-latinoam [Internet]. 2010;36(3):247-54. Disponible en: doi: 10.4321/s0376-78922010000300007 [ Links ]
2. Navarro Cecilia J, Leon Llerena C, Luque Lopez C. Uso de Terapia VAC en paciente pediatrico con exposicion osea postamputacion tras purpura fulminans. Cir plast ibero-latinoam [Internet]. 2011;37(1):S59-S63. Disponible en: doi: 10.4321/s0376-78922011000500009 [ Links ]
3. Rotella JM. Colgajos musculares locales en heridas graves de pierna. Rev Asoc Arg Ortop y Traumatol [Internet]. 2000;61(2):157-68. Disponible en: https://www.aaot.org.ar/revista/1993_2002/1996/1996_2/610203.pdf [ Links ]
4. Pichardo Leon N, Puente Alvarez A, Basulto Gomez M, Puig Rodriguez A. Colgajo fasciomuscular del gastrocnemio medial: presentacion de un caso. Arch med Camaguey [Internet]. 2011;15(5):873-81. Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1025-02552011000500011 [ Links ]
5. Marquez Zevallos C, Alcocer Cordero P, Bermudez Farias W, Navarrete Quiroz L. Reconstruccion de rodilla con doble colgajo de gemelo. Cir plast ibero-latinoam [Internet]. 2011;37(2):143-46. Disponible en: doi: 10.4321/s0376-78922011000200006 [ Links ]
6. Iheozor-Ejiofor Z, Newton K, Dumville JC, Costa ML, Norman G, Bruce J. Negative pressure wound therapy for open traumatic wounds. Cochrane Database Syst Rev [Internet]. 2018;7:CD012522. Disponible en: doi: 10.1002/14651858.CD012522.pub2 [ Links ]
7. Najarro Cid F, Garcia Ruano AA, Luanco Gracia M, Jimenez Martin A, Sicre Gonzalez M. Terapia por presion negativa en el manejo de heridas complejas en traumatologia: Innovacion e indicacion. Rev S And Traum y Ort [Internet]. 2014;31(2):17-23. [ Links ]
8. Rotella PS, Valero Barg FR. Tratamiento de defectos de cobertura en los miembros con el sistema de presion negativa en pacientes con cultivo positivo. Rev Asoc Argent Ortop Traumatol [Internet]. 2011;76(1):52-9. Disponible en: http://www.scielo.org.ar/scielo.php?script=sci_arttext&pid=S1852-74342011000100008 [ Links ]
9. Calixto Ballesteros LF, Villegas Gonzalez M. Aplicacion de sistemas topicos de presion negativa en heridas y defectos de cobertura en extremidades traumatizadas. Rev Col Or Tra [Internet] 2013;27(1):48-55. Disponible en: https://www.sccot.org.co/pdf/RevistaDigital/2701-2013/08PresionNegativa.pdf [ Links ]
10. Webster J, Liu Z, Norman G, Dumville JC, Chiverton L, Scuffham P, et al. Negative pressure wound therapy for surgical wounds healing by primary closure. Cochrane Database Syst Rev [Internet]. 2019 Mar 26;3(3):CD009261. [ Links ]
11. Perilla Escorcia C. Uso de sistema de presion negativa (VAC) para tratamiento de herida compleja en dorso de mano y antebrazo derecho [tesis de grado]. Colombia: Universidad Simon Bolivar; 2021. Recuperado a partir de: https://bonga.unisimon.edu.co/bitstream/handle/20.500.12442/7168/Uso_Sistema_Presi%c3%b2n_Negativa_VAC_Resumen.pdf?sequence=1&isAllowed=y [ Links ]
12. Chau Ramos EA. Sistema de aspiracion a presion negativa en ulceras traumaticas, Clinica Stella Maris 2015-2016 [tesis de grado]. Peru: Universidad de San Martin de Porres; 2017. Recuperado a partir de: https://repositorio.usmp.edu.pe/handle/20.500.12727/3385 [ Links ]
13. Felemovicius Hemangus J, Lopez Konschot RC. Uso de la terapia de presion negativa en el tratamiento de heridas complejas. An Med (Mex) [Internet]. 2015;60(2):141-7. Disponible en: https://www.medigraphic.com/pdfs/abc/bc-2015/bc152k.pdf [ Links ]
14. Goyo B, Lanzotti M, Torrealba A, De Felice LG. Aplicacion de terapia de presion negativa en el manejo de pacientes con heridas complejas. JONNPR [Internet]. 2020;5(12):1490-503. Disponible en: https://revistas.proeditio.com/jonnpr/article/view/3827 [ Links ]
15. Gomez Lopez BE. Uso de la Terapia de Presion Negativa en el manejo de las Ulceras por Presion [tesis de pregrado]. Espana: Universidad de Murcia; 2020. Recuperado a partir de: https://repositorio.ucam.edu/bitstream/handle/10952/4981/Bel%C3%A9n%20Encarnaci%C3%B3n%20G%C3%B3mez%20L%C3%B3pez.pdf?sequence=1&isAllowed=y [ Links ]
16. Guevara Moraga LS. Experiencia en el uso de sistema de cierre asistido por vacio en abdomen abierto, pacientes ingresados en el Hospital Escuela Antonio Lenin Fonseca, noviembre 2015 a enero 2017 [tesis de grado]. Nicaragua: Universidad Nacional Autonoma de Nicaragua UNAM-Managua; 2017. Recuperado a partir de: https://repositorio.unan.edu.ni/4454/1/96911.pdf [ Links ]
17. Bernal-Martinez AJ, Lopez-Cabrera P, Sampietro de Luis JM, Puertas-Pena J, Agullo-Domingo A. La terapia de vacio como alternativa terapeutica en quemaduras con exposicion osea. Cir plast ibero-latinoam [Internet]. 2016;42(4):355-60. Disponible en: https://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S0376-78922016000400007 [ Links ]
18. Viosca E, Martinez JL, Almagro PL, Gracia A, Gonzalez C. Proposal and validation of a new functional ambulation classification scale for clinical use. Arch Phys Med Rehabil [Internet]. 2005;86(6):1234-8. Disponible en: https://pubmed.ncbi.nlm.nih.gov/15954065/ [ Links ]
19. Rosanna Chau MW, Chan SP, Wong YW, Lau MYP. Reliability and validity of the Modified Functional Ambulation Classification in patients with hip fracture. Hong Kong Physiother J [Internet]. 2013;31(1):41-4. Disponible en: doi: 10.1016/j.hkpj.2013.01.041 [ Links ]
20. Allende C, Fernandez Savoy I, Allende BL, Ruchelli L, Gutierrez N. Lesiones combinadas complejas postraumaticas en la pierna: Tratamiento temprano frente a tratamiento diferido. Rev Asoc Argent Ortop Traumatol [Internet]. 2015;80(3):196-206. Disponible en: http://www.scielo.org.ar/scielo.php?script=sci_arttext&pid=S1852-74342015000300009 [ Links ]
21. Anghel EL, Kim PJ. Negative-Pressure Wound Therapy: A Comprehensive Review of the Evidence. Plast Reconstr Surg [Internet]. 2016;138(3 Suppl):129S-137S. Disponible en: https://pubmed.ncbi.nlm.nih.gov/27556753/ [ Links ]
22. Flores-Alvarez E, Sanchez-Miranda G, Fernandez-Sanchez AK. Uso del sistema VAC en el manejo de pacientes con gangrena de Fournier. Cir Gen [Internet]. 2019;41(4):270-5. Disponible en: https://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S1405-00992019000400270 [ Links ]
23. Sanchez Neila N, Hermosa Gelbard A, Miguel Gomez L, Vano Galvan S. Protocolo diagnostico de las ulceras cutaneas. Medicine [Internet]. 2014;11(47):2800-5. Disponible en: doi: 10.1016/s0304-5412(14)70700-0 [ Links ]
24. Kucharzewski M, Mieszczanski P, Wilemska-Kucharzewska K, Taradaj J, Kuropatnicki A, Sliwinski Z. The application of negative pressure wound therapy in the treatment of chronic venous leg ulceration: authors experience. Biomed Res Int [Internet]. 2014;2014:297230. Disponible en: https://pubmed.ncbi.nlm.nih.gov/24696847/ [ Links ]
25. Buendia Perez J, Vila Sobral A, Gomez Ruiz R, Qiu Shao SS, Marre Medina D, Romeo M, et al. Tratamiento de heridas complejas con terapia de presion negativa: Experiencia en los ultimos 6 anos en la Clinica Universitaria de Navarra, Pamplona (Espana). Cir plast ibero-latinoam [Internet]. 2011;37:S65-71. Disponible en: https://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S0376-78922011000500010 [ Links ]
26. Peinemann F, Labeit A. Negative pressure wound therapy: A systematic review of randomized controlled trials from 2000 to 2017. J Evid Based Med [Internet]. 2019;12(2):125-32. Disponible en: doi: 10.1111/jebm.12324 [ Links ]
27. Hernadez Barrios D. Escala de Evaluacion para la Capacidad de marcha, segun Funcional Ambulatory Classificator [Internet]. Medicina de rehabilitacion biomecanica. Disponible en: http://www.sld.cu/sitios/rehabilitacion-bio/temas.php?idv=21600. [ Links ]
28. Instituto Nacional de Salud; Sistema de terapia de presion negativa para el tratamiento de heridas [Internet]. Lima (Peru): Instituto Nacional de Salud; 2019. Disponible en: https://web.ins.gob.pe/sites/default/files/Archivos/authenticated%2C%20administrator%2C%20editor/publicaciones/2019-12-24/ETS%200023%20-%20Terapia%20de%20presi%C3%B3n%20negativa%20VF.pdf [ Links ]
29. Maitret-Velazquez RM, Bizueto-Rosas H, Gomez-Calvo CD, PerezGonzalez HA, Moreno-Ramirez CI, Hernandez-Vazquez JI. Uso de terapia de presion negativa para manejo de heridas complejas. Rev Mex Angiol [Internet]. 2018;46(1):9-18. Disponible en: https://www.medigraphic.com/cgi-bin/new/resumen.cgi?IDARTICULO=80557 [ Links ]
Received: January 17, 2023; Revised: January 26, 2023; Accepted: February 07, 2023











 texto em
texto em