Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Horizonte Médico (Lima)
versão impressa ISSN 1727-558X
Horiz. Med. vol.23 no.2 Lima abr./jun. 2023 Epub 30-Maio-2023
http://dx.doi.org/10.24265/horizmed.2023.v23n2.09
Case report
Giant hiatal hernia: a clinical case
1 Hospital Regional del Cusco. Cusco, Peru.
2 Universidad Andina del Cusco, Faculty of Health Sciences, School of Human Medicine. Cusco, Peru.
3 Universidad Andina del Cusco, Centro de Investigación en Neurociencias (CENEURO - Neuroscience Research Center). Cusco, Peru.
Giant hiatal hernia (HH) is a condition in which more than 30 % of the stomach is displaced upward toward the thorax, thus producing an abnormal protrusion above the diaphragmatic pinch. This can occur by various mechanisms such as alterations at the gastroesophageal junction or diaphragmatic atrophy that can take place due to a number of reasons, including involutional changes, extensive trauma or damage to the phrenic nerve.
Most cases are usually asymptomatic; however, when clinical manifestations occur, they vary depending on the size of the herniation and range from chest pain (also epigastric pain), nausea, vomiting to abdominal distension. In case of presenting complications such as gastric volvulus or Cameron lesions, the symptoms include Borchardt’s triad, which consists of abdominal pain and distension, violent vomiting and difficulty passing a nasogastric tube.
We present the case of an 82-year-old male patient who was admitted to the emergency room for severe abdominal pain, severe hematemesis and sensory disorder. On physical examination, pale facies and diaphoresis were observed; on palpation, the main indication was abdominal pain in the epigastric area. Emergency endoscopy was requested, finding a deep ulcer with congestive edges and active bleeding in the lower portion of the esophagus, in addition to observing that part of the gastric fundus and the cardias were herniated toward the thorax. This confirmed the diagnosis of a giant HH; however, the treatment was interrupted by the patient when he asked for voluntary discharge after refusing to undergo surgery.
Keywords: Hernia, Hiatal; Abdominal Pain; Endoscopy; Altitude
Introduction
In 1926, the term “hiatal hernia” was coined by Ake Akerlund, who described it as the sliding of parts of the stomach through the esophageal opening 1.
Currently, it refers to the displacement of abdominal contents toward the thorax, thus producing an abnormal protrusion through the esophageal hiatus of the diaphragm 1,2.
This abnormal eventration occurs due to alterations at the gastroesophageal junction, where the diaphragm muscle fibers are replaced by thin fibrous tissue or by diaphragmatic atrophy due to involutional changes, extensive trauma or irreversible damage to the phrenic nerve, which cause loss of elasticity and atony in the diaphragm, thus causing stomach herniation above the diaphragmatic pinch 2.
Hiatal hernias (HHs) are roughly classified into four types:
Type I (sliding): hernias with displacement of the gastroesophageal junction above the diaphragm, where the stomach keeps its position and the fundus stays below the gastroesophageal junction; these are the most frequent ones and account for 95 % of the cases 2.
Type II (paraesophageal): characterized by a herniation caused by an upward movement of the stomach fundus due to defects of the phrenoesophageal membrane, with no alteration of the gastroesophageal junction 2.
Type III (mixed): characterized by presenting elements that are similar to those of type I and II hernias, in which herniation appears through the esophageal hiatus of the gastroesophageal junction and gastric fundus, and is located above the gastroesophageal junction 2.
Type IV (upside-down stomach): caused by a big defect of the phrenoesophageal membrane, where herniation of several elements—such as the small intestine, pancreas, spleen, among others—are observed 2.
Clinical case
An 82-year-old male patient was rushed to the Emergency Room at Hospital Regional del Cusco because of severe hematemesis, melena and sensory disorder. The physical exam revealed that the patient was in poor health status, with a heart rate of 120 bpm and blood pressure of 80/50 mmHg. Moreover, pale facies and diaphoresis were observed. A peripheral line was inserted in both arms to hydrate him with physiological saline solution; then a hemoglobin test was done, resulting in 7.2 g/dl. Therefore, the patient received a transfusion of two units of packed red blood cells to be stabilized. As the hematemesis continued, an emergency endoscopy was performed, showing a deep ulcer with congestive edges in the lower section of the esophagus, at 30-32 cm, and active oozing bleed (Figure 1). The patient was treated with an injection therapy of adrenaline 1/10,000 in four quadrants of the ulcer, and the bleeding was controlled. Likewise, the esophagus and stomach were examined, evidencing that the Z line was 30 cm from the upper dental arch and 40 cm from the diaphragmatic pinch. The gastric evaluation of the retroversion revealed that the cardias and part of the fundus were herniated toward the thorax, with no evidence of other alterations. It was concluded that he had a 10-cm-long giant type I esophageal hernia, complicated with a 2-cm-diameter ulcer with active bleeding, which was controlled by endoscopic treatment.
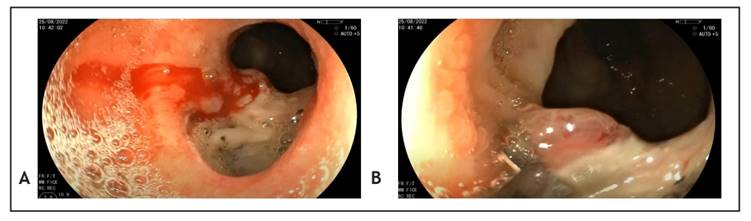
Figure 1 Patient’s endoscopy. (A) Esophageal ulcer with active bleeding. (B) Post-hemostasis esophageal ulcer after administering adrenaline.
Thereafter, when the bleeding was totally controlled and the patient was stable, he was admitted to the Surgery Department for subsequent surgical treatment.
Discussion
There is no standard definition for giant HH: some authors define it as the herniation of more than 30 % and others of more than 50 % of the stomach. In fact, any hernia with more than half the stomach herniated toward the thorax should be considered as a giant HH 3.
The etiology of giant HH can be explained by two mechanisms: (1) gastroesophageal reflux disease (GERD), which causes scarring and shortening of the esophagus, resulting in traction of the gastroesophageal junction and gastric hernia, and (2) chronic positive pressure on the diaphragmatic hiatus combined with propensity for herniation, which leads to gastric displacement toward the thorax, resulting in GERD.
HH is classified by type: type I refers to slipping hernia, type II to paraesophageal hernia (≤ 5 %), type III to mixed slipping and paraesophageal hernia, and type IV to hernia of other organs (e.g., colon, omentum and spleen) 4.
A predisposing factor for HH is age since aging progressively weakens the structures that fix the gastrointestinal junction in place, which causes the widening of hiatal tunnel muscles; hence, there is an increased risk of suffering from this condition.
Many patients are asymptomatic. Sometimes, they may present pyrosis and esophageal discomfort. However, they may also present reflux, regurgitation, dysphagia, nausea, vomiting and hematemesis. In asymptomatic patients, the hernia can grow and cause more alterations to the phrenoesophageal ligament 5.
If complications are found, the symptoms will be characteristic of the Borchardt’s triad, which consists of abdominal pain and distension, violent vomiting or inability to vomit and difficulty passing a nasogastric tube.
HH has been associated with esophagitis in 20 %, duodenal ulcer in 20 %, diverticulosis in 25 % and gallstones in 18 % 6.
Concerning ex novo symptoms, dysphagia and anatomic failures were seen in 18 % and 26.1 % of patients under 65 years of age, respectively, and in 27.8 % of those over 75 years. Moreover, a proton pump inhibitor use of 10 % and a recovery rate of 3 % have been observed. A radiological recurrence of up to 66 % has been reported, but these cases are related to hernias of less than 5 cm, with no clinical consequences. They are considered hernias, but they are often a phrenic ampulla and not a hernia per se 7.
When hernias are small, their progression is usually benign. Sometimes they can cause gastritis, becoming later a gastric ulcer at the herniated site. When hernias are large, they can cause complications such as circulatory and respiratory disorders and injuries to displaced organs, such as gastric volvulus, perforation, gangrene, hemorrhage and shock, which increase mortality 8.
The most frequent complications of HH may include the following:
Intermittent bleeding due to esophagitis.
Cameron lesions, which lead to iron deficiency anemia 9.
The presence of esophagitis in patients with HH is associated with other diseases such GERD, whose incidence rate has been divided according to the symptoms: asymptomatic in 20.47 % and symptomatic in 37.50 % of the cases 10.
Cameron lesions resulted from the constant mechanical erosion of the gastric mucosa every time the stomach passed through the hernia hiatus in each respiratory movement. They were associated with iron deficiency anemia and were found in the mucosal folds located at or near the diaphragmatic hiatus during the endoscopy 11.
Gastric volvulus is a chronic condition in which the stomach undergoes an organoaxial torsion. It is caused by a blunt abdominal trauma and does not present characteristic symptoms. Likewise, total strangulating stomach obstructions may occur, thus causing necrotizing damage. In that event, the only treatment is performing surgery as soon as possible 12.
Also, the case showed a clinical picture that was simple and quick to assess. However, it could trigger complications if not detected promptly. The patient presented GERD as the main symptom, severe anemia as a consequence of the heavy bleeding that caused hematemesis and, finally, melena.
The following imaging tests are recommended for the diagnosis of HH: chest X-ray because it shows hernia as an incidental mediastinal mass; computerized tomography with multiplanar reconstruction to make the differential diagnosis among the different types of hernias and assess whether there is herniation of the surrounding structures; upper GI endoscopy, used less frequently since it is useful to confirm whether there is gastric obstruction and rule out ischemic lesions in the gastric mucosa 13. Because of the patient’s critical condition when he was admitted, the method used was endoscopy, which measured the distance from the phrenoesophageal ligament to the stomach folds, confirming a 10-cm giant HH.
Treatment for hernias is surgery; it is recommended to reduce hernias with a sac dissection and resection and subsequent esophageal restitution to the abdomen 14. After the treatment, hernias tend to reappear since the hiatus is exceeded by the pressure between the intraabdominal and intrathoracic compartments. To avoid recurrence, there are treatments such as repair with biologic mesh, which reinforces surgical sutures, thus preventing tension 15. In this case, the patient refused to undergo surgery; nevertheless, it was decided to follow up the patient since he did not present additional complications typical of hernia such as obstruction or perforation.
REFERENCES
1. Mantilla-Cadena EN, Montenegro-Garcia ED, Morales-Silva BL, Navarrete-Acuna SP. Diagnostico y tratamiento de las Hernias Hiato, articulo de revision. Domino de las Ciencias. 2022;8(2):370-86. [ Links ]
2. Kahrilas PJ. Hiatus hernia. UpToDate [Internet]. 2021; Disponible en: https://www.uptodate.com/contents/hiatus-hernia?search=hiatal%20hernia&source=search_result&selectedTitle=1~93&usage_type=default&display_rank=1 [ Links ]
3. Farina del Rio M, Rodriduez A, Melgarejo S. Hernia hiatal gigante. Reporte de caso. Rev Cir Parag. 2018;42(1):41-3. [ Links ]
4. Cha RR. Find out the differences by types of hiatal hernia! J Neurogastroenterol Motil. 2020;26(1):4-5. [ Links ]
5. Csendes A, Braghetto I, Burgos AM, Henriquez A. Sintomas, hallazgos radiologicos, endoscopicos y estudios funcionales del esofago en pacientes con hernia hiatal mayor a 5 cm. Rev Chil Cir. 2013;65(5):402-8. [ Links ]
6. Madriz W, Alvarado VH, Jaen J. Diagnostico radiologico de hernia hiatal. Rev Med Cos Cen. 2008;65(583):103-8. [ Links ]
7. Braghetto I, Csendes A, Korn O, Musleh M, Lanzarini E, Saure A, et al. Hernias hiatales: ï¿1/2cuando y por que deben ser operadas? Cir Esp. 2013;91(7):438-43. [ Links ]
8. Elizondo-Argueta S, Rodriguez-Guerrero F. Diaphragmatic Hernia, A propos of a Case. Medicina Interna de Mexico. 2013;29(5):525-28. [ Links ]
9. Qureshi WA. Hiatal Hernia: Practice Essentials, Background, Pathophysiology [Internet]. Medscape. 2019 [citado el 7 de marzo de 2023]. Disponible en: https://emedicine.medscape.com/article/178393-overview [ Links ]
10. Ramon PJ. La hernia hiatal y su relacion con el reflujo gastroesofagico. Gen. 2010;64(4):306-10. [ Links ]
11. Bernardo RJ, Portocarrero JP, Tagle M. Lesiones de Cameron: experiencia clinica. Rev Gastroenterol Peru. 2012;32(2):157-60. [ Links ]
12. Ospino-Saumett G, Martinez-Barbosa P, Valverde-Robert R. Volvulo gastrico intratoracico secundario a hernia diafragmatica izquierda cronica postraumatica. Acta Med Costarric. 2005;47(2):94-6. [ Links ]
13. De Grazia JA, Godoy M, Cavallo I, Cortes C. Hernia hiatal gigante con estomago intratoracico: Reporte de un caso y revision de la literatura. Rev Chil Radiol. 2012;18(4):179-83. [ Links ]
14. Pereira JG, Roque R, Martinez MA, Torres R, Barreras J, Lopez AB. Cirugia videolaparoscopica en la hernia hiatal gigante. Rev Cubana Cir. 2015;54(2):148-56. [ Links ]
15. Saad AR, Velanovich V. Laparoscopic antireflux surgery: Are old questions answered? Mesh hernioplasty. ABCD, Arq Bras Cir Dig. 2022;35:e1710. [ Links ]
Received: December 13, 2022; Revised: January 30, 2023; Accepted: February 14, 2023











 texto em
texto em 



