Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Horizonte Médico (Lima)
versión impresa ISSN 1727-558X
Horiz. Med. vol.23 no.2 Lima abr./jun. 2023 Epub 30-Mayo-2023
http://dx.doi.org/10.24265/horizmed.2023.v23n2.11
Case report
Dropped appendicolith following an appendectomy
1 Universidad César Vallejo, School of Medicine. Trujillo, Peru.
2 Hospital III de Emergencias Grau EsSalud. Lima, Peru.
Dropped appendicolith following an appendectomy is a rare complication which may occur as a consequence of appendicolith expulsion from the appendix due to a previous perforation or failure to identify the appendicolith. A fecalith generally becomes symptomatic over time as a result of abscess formation, intestinal obstruction, fistula tract or inflammation of the appendiceal stump. Two cases of dropped appendicolith following an appendectomy are described hereinbelow. Case 1: A 23-year-old female patient, who underwent an appendectomy the previous day, was admitted to the emergency room due to hypogastric pain. A computed tomography (CT) scan revealed a dropped appendicolith in the right iliac fossa, and a diagnostic laparoscopy showed intra-abdominal abscesses and a dropped appendicolith in the appendiceal stump. Case 2: A 77-year-old male patient, who underwent surgery for acute appendicitis caused by appendicoliths, showed abdominal distension on the sixth postoperative day. The CT scan revealed intestinal obstruction and a dropped appendicolith at bowel loops. In the surgical reintervention, erosion of the mesentery caused by the appendicolith was evidenced. Both patients made good progress after the reoperations. The incidence of dropped appendicolith following an appendectomy is currently unknown since few data are available in the literature worldwide. Therefore, it is important to present these cases to expand the casuistry, learn more about dropped appendicoliths following an appendectomy, demonstrate their complications if they are not removed early and show how to prevent them. In conclusion, dropped appendicoliths following an appendectomy must be removed early to avoid complications.
Keywords: Appendicitis; Appendectomy; Fecal Impaction
Introduction
Acute appendicitis is the most frequent surgical emergency 1 and one of its causes is the obstruction of the appendiceal lumen by a concretion 2. Appendicoliths—also known as fecalith, coprolith, stercolith—are incidentally found in up to 32 % of the asymptomatic population 3,4. Appendicoliths are usually small 5; those measuring ≥ 5 mm or multiple appendicoliths are associated with acute appendicitis and higher rates of perforated appendicitis 2,3.
Appendicoliths are composed of firm stools, mineral deposits, fats, inorganic salts (calcium phosphate) and organic waste. Its hardness is directly related to the amount of calcium it contains 4. There is no known correlation between appendicolith and appendiceal malignancy 6.
Dropped or retained appendicolith following an appendectomy is a rare complication which may occur as a consequence of appendicolith expulsion from the appendix due to a previous perforation or failure to identify the appendicolith 4,7,8 or a forced removal through the umbilical port during a laparoscopic appendectomy 4. Complications associated with dropped appendicoliths have been more prevalent with the use of laparoscopic appendectomy 8.
Dropped appendicoliths are most frequently found in the paracecal space 9, pelvis or Morison’s pouch. Pneumoperitoneum, irrigation and positioning used during a laparoscopy can cause the appendicolith to move to unusual sites 10. Literature review shows that a fecalith can remain free in any part of the abdominal cavity, such as in the intestine 11, pouch of Douglas, rectovesical pouch, fallopian tubes and perihepatic space 9; within the liver parenchyma 12-14; and even in the subcutaneous tissue 12,15,16, iliopsoas compartment and gluteal 4 or thoracic region 10.
In most cases, the fecalith becomes symptomatic over time, as a result of abscess formation, fistula tract or inflammation of the appendiceal stump (stump appendicitis) 11.
The main objective of this case report is to demonstrate the complications of dropped appendicoliths following an appendectomy and the importance of their early removal.
Clinical case
Case 1
A 23-year-old woman was admitted to the emergency room of a public hospital in Lima, Peru, on October 17, 2022 (day 1), complaining of colicky pain in the right iliac fossa for four hours. Additionally, she reported a history of Cesarean section. Tests revealed her leukocyte count was 9,080/mm3; subsequently, she was diagnosed with acute appendicitis by clinical signs and symptoms, which was confirmed by computed tomography (CT) scan (Figure 1A). On the same day, a laparoscopic appendectomy was performed, where a 7 x 0.9 cm suppurative cecal appendix with approximately 50 cc purulent drainage in the pouch of Douglas was evidenced.
During the postoperative period, the patient made good progress and was discharged the day after the operation (day 2). On the second day of the postoperative period (day 3), the patient was readmitted to the emergency room of the same hospital because of pain in the hypogastrium, nausea and vomiting. A non-contrast CT scan showed the following findings (October 19) (Figure 1B): “impression of free fluid at the pouch of Douglas and presence of appendicolith.” Leukocytes: 6,020/mm3, C-reactive protein (CRP): 151.44 mg/l.
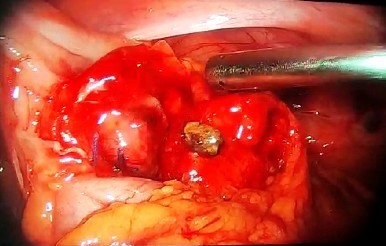
On October 20 (day 4), the patient was reoperated: a diagnostic laparoscopy evidenced approximately 280 cc seropurulent drainage at the pouch of Douglas, right paracolic gutter and right subphrenic space; multiple adhesions in the right lower quadrant; cecal appendix with undamaged stump and one coprolite inside, which was removed (Figure 2).
During the postoperative period, the patient made good progress and was discharged the day after the surgical reintervention (day 5).
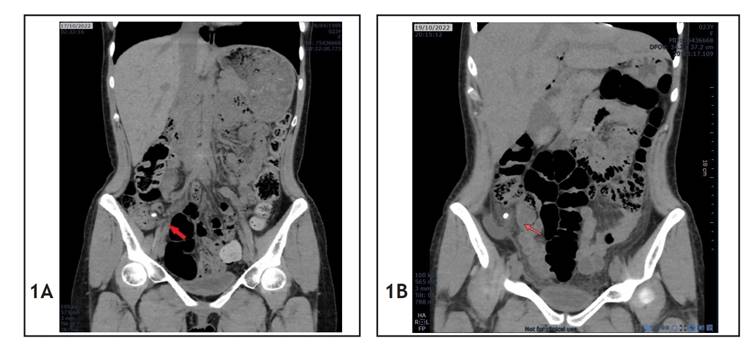
Figure 1 Case 1 CT scans. (A) Preoperative abdominal CT scan; the red arrow shows the appendicolith. (B) Postoperative abdominal CT scan; the red arrow shows the dropped appendicolith.
Case 2
A 77-year-old male was admitted to the emergency room of a public hospital in Lima on November 16, 2021 (day 1), complaining of pain in the hypogastrium for four days, with a history of hypertension and cholecystectomy. After being examined, the patient was diagnosed with acute appendicitis, confirmed by a CT scan which provided the following findings (Figure 3A): “cecal appendix thickening, 17 mm in diameter, with appendicoliths and gas bubbles inside.” The tests revealed his leukocytes: 15,290/mm3. He was then scheduled for a laparoscopic appendectomy. During the operation, an appendiceal phlegmon with friable bowel loops were observed; therefore, it was decided to convert the operation into an open appendectomy. Adhesions were removed, with opening of Toldt’s fascia of the right paracolic gutter. A retrocecal, retroperitoneal, ascending, completely necrotic cecal appendix with necrotic mesoappendix was found; two coprolites were removed from the tip of the appendix, where 15 cc abscess was drained; and an appendectomy was performed. A Penrose drain with counteropening was placed at the appendiceal stump. During the postoperative period, a tree-day fast, ceftriaxone and metronidazole were prescribed.
During postoperative hospitalization, the patient made good progress: on the fourth postoperative day (day 5) he started a soft food diet and on the following day (day 6) a complete diet, which was well tolerated, with elimination of flatus and stools. On the sixth postoperative day (day 7), the patient experienced belching and abdominal distension, so a CT scan was requested (Figure 3B). The CT scan revealed the following findings: “thin intestinal loops dilated in both the jejunum and proximal ileum, with a maximum diameter of 41 mm and several air-fluid levels; rule out adhesions. At this level, a 9 mm loose hyperdense mass in peritoneal fat, surrounded by gas, with a morphology similar to an appendicolith and collapsed thick loops was detected, not seen in a previous control.” With this report, a medical board was held to evaluate the risk-benefit of a second surgical intervention versus conservative management. It was concluded that a surgical intervention would be the most beneficial option.
On November 23 (day 8), the patient was reoperated and the following was observed: intestinal obstruction due to adhesions of the ileum, proximal to the right paracolic gutter, with scarce purulent drainage, although the fecalith was not located at that level. Therefore, a systemic examination of the entire small intestine was performed, evidencing an appendicolith of 1 cm in diameter located at the mesentery of the jejunum, at 1 m from the angle of Treitz, with erosion of the mesentery caused by the appendicolith (Figure 4).
During the postoperative period, the patient made good progress and was discharged on the seventh day of the reoperation (day 15).
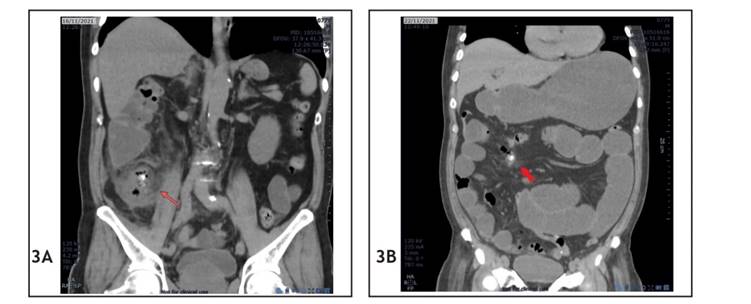
Figure 3 Case 2 CT scans. (A) Preoperative abdominal CT scan; the red arrow shows the appendicolith. (B) Abdominal CT scan on the sixth postoperative day; the red arrow shows the dropped appendicolith at the intestinal loops.
Discussion
In the first case, the patient developed an intra-abdominal abscess as a complication of a dropped appendicolith. Dropped appendicoliths are known to be strongly associated with intra-abdominal abscess formation 1. This abscess formation is because appendicoliths are potentially infectious since they harbor bacteria 4. The sites of abscess formation documented in the literature are the subhepatic, perihepatic, pelvic, tubo-ovarian and paracecal spaces, including the psoas and gluteal muscles 4,11,17. The timeline to develop an abscess varies from a few months to 15 years 9,18; however, in this case, only 48 hours were enough to develop the intra-abdominal abscess, a fact that caught our attention.
Dropped appendicoliths can also cause a mechanical obstruction of the small intestine as an early event 1. However, in our second case, the appendicolith was not precisely the cause of the obstruction: it was immediately suspected because the existing literature shows intestinal obstructions caused by dropped appendicoliths 1. During the surgery, a complication due to a dropped appendicolith not reported in the literature was observed: the erosion of the mesentery which occurred 6 days after the operation.
As a dropped appendicolith was suspected, both patients underwent a CT scan, since it is considered the most sensitive and specific diagnostic study for this condition 1,14,19.
Most surgeons consider that the definitive treatment of a dropped appendicolith is its surgical removal. Otherwise, recurrent intra-abdominal abscesses, wound infection and fistula formation may occur 4,12,13,15. Another method to remove a dropped appendicolith is by transcutaneous approach, indicated for masses < 10 mm, which may be a feasible and safe method 9.
In contrast, Albdah (2021) considers a conservative management of dropped appendicoliths with chronic pain or abscess, although his study was based only on two patients whose follow-up lasted one year. And, as it is well-known, complications may appear after several years. Consequently, in order to prevent dropped appendicoliths following an appendectomy, several authors state that dropping the appendicolith into the abdominal cavity must be avoided during surgery, for which a careful dissection must be performed, placing a double ligation of the appendiceal base (which has been associated with less chance of retention of the appendicolith) 4, paying careful attention at the moment of the appendiceal extraction and ensuring an adequate coagulation of the stump 12. During an appendectomy, the use of bags will reduce the chances of appendix fall during its removal and inadvertent wound contamination of the port site 4. Likewise, it is important to routinely check the appendiceal stump, paracolic gutters and pelvis 1.
The incidence of dropped appendicoliths following an appendectomy, whether conventional or laparoscopic, is currently unknown, as few data are available in the world literature 16. There has also been no meta-analysis or systematic review on the subject up to the time of the present work. Babington (2023) collected 24 related scientific articles on appendicoliths from the available literature, out of which only 6 addressed dropped appendicoliths 21. Therefore, it is important to present these cases in order to expand the casuistry and contribute to the knowledge of dropped appendicoliths following an appendectomy.
In conclusion, the definitive treatment of a dropped appendicolith following an appendectomy should be its early removal to avoid complications.
REFERENCES
1. Villalobos EJ, Lopez A, Sainz JC, Murillo A. Absceso subhepatico secundario a apendicolito retenido. Reporte de caso. Rev Mex Cir Endoscop. 2017;18(1):40-3. [ Links ]
2. Lafleche P, Pillay Y. Acute appendicitis with four appendicoliths: a first case report in the English literature. J Surg Case Rep. 2020;2020(7):rjaa173. [ Links ]
3. Wang N, Lin X, Zhang S, Shen W, Wu X. Appendicolith: an explicit factor leading to complicated appendicitis in childhood. Arch Argent Pediatr. 2020;118(2):102-8. [ Links ]
4. Albdah A, Aljomah N, Shalhoub M, Zekry A, Beyari N, Bahgat F, et al. Benefits of conservative management of a retained appendicolith after laparoscopic appendectomy: A case series. Int J Surg Case Rep. 2021;82:105925. [ Links ]
5. Sagkriotis I, Habib Z, Zardab M. Between a rock and a hard place: retained appendicolith causing a mechanical small bowel obstruction. J Surg Case Rep. 2020;30(9):rjz393. [ Links ]
6. Rampersad CA, Rampersad FS, Ramraj PR. Seetahal VV. Case of a Giant Appendicolith. Cureus. 2022;14(2):e22034. [ Links ]
7. Ansari FA, Bilal MI, Gondal MUR, Latif M, Iqbal N. Delayed Presentation of a Retained Fecalith. Cureus. 2021;13(6):e15919. [ Links ]
8. Ajitha MB, Ramya Y, Sharath KL. Dropped Appendicolith: Complications and Management. Int J Biomed Res. 2015;6(02):65-70. [ Links ]
9. Sundararajan L, Prabhu K, Ramesh V, Sankar J. Empyema due to Thoracic Migrating Appendicolith. Indian Pediatr. 2018;55(7):603-4. [ Links ]
10. Assenza M, Ciccarone F, Santillo S, Mazzarella G, De Meis E, Bracchetti G, et al. Hepatic abscess: An uncommon complication after laparoscopic appendectomy. Ann Ital Chir. 2021;10:1-5. [ Links ]
11. Jamil Y, Reading N. Learning from the radiological findings of dropped gall stone and/or appendicolith (its complication and management strategy). BJR Case Rep. 2019;5(2):20180096. [ Links ]
12. Muyldermans K, Brussaard C, Willekens I, de Mey J. Liver Abscess Due to Dropped Appendicolith after Laparoscopic Appendectomy. J Belg Soc Radiol. 2015;99(2):47-9. [ Links ]
13. Drew Z, Jain D, Mariyappa B. Migrating appendicolith: A retained appendicolith causing recurrent infection and migrating to the skin. BJR Case Rep. 2022;7(6):20210093. [ Links ]
14. Phan D, Goh IY, Muduioa G. Pelvic abscess masquerading as urachal malignancy-a rare presentation of retained appendicolith. J Surg Case Rep. 2022;2022(2):rjab597. [ Links ]
15. Abdullah HMA, Atiq M, Yeager T. Percutaneous removal of a retained appendicolith causing recurrent perihepatic abscesses between the liver and diaphragm. BMJ Case Rep. 2019;12(7):e230176. [ Links ]
16. Singh SC, Weber F, Meyers AB, Reyes C, Epelman M. Perihepatic abscesses caused by dropped appendicoliths in a child. Radiol Case Rep. 2018;14(1):1-5. [ Links ]
17. Ranieri DM, Enzerra MD, Pickhardt PJ. Prevalence of Appendicoliths Detected at CT in Adults With Suspected Appendicitis. AJR Am J Roentgenol. 2021;216(3):677-82. [ Links ]
18. Baskovic M, Sovic L, Posaric V, Crnjak I. Retained Appendicolith in Children a Case Report and Literature Review. Central Eur J Paed. 2022;18(1):44-9. [ Links ]
19. Cibulas M, Lao O. Retained appendicolith: Some things work themselves out. J Pediatr Surg Case Rep. 2022;81:102260. [ Links ]
20. Khan MS, Chaudhry MBH, Shahzad N, Khan MS, Wajid M, Memon WA, et al. The Characteristics of Appendicoliths Associated with Acute Appendicitis. Cureus. 2019;11(8):e5322. [ Links ]
21. Babington EA. Appendicoliths, the little giants: A narrative review. Radiography (Lond). 2023;29(1):1-7. [ Links ]
Received: January 09, 2023; Revised: January 24, 2023; Accepted: February 06, 2023











 texto en
texto en