Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Horizonte Médico (Lima)
versão impressa ISSN 1727-558X
Horiz. Med. vol.23 no.3 Lima jul./set. 2023 Epub 13-Set-2023
http://dx.doi.org/10.24265/horizmed.2023.v23n3.01
Original article
Pediatric graduate students’ and pediatricians’ knowledge and habits on child oral health
1 Universidad Maimónides, Department of Maternal and Child Health. Buenos Aires, Argentina.
2 Universidad Maimónides, Graduate School, Pediatric Dentistry Specialty. Buenos Aires, Argentina.
Objective:
To analyze child oral health training background, habits and knowledge in a group of pediatric graduate students and recently graduated pediatricians.
Materials and methods:
A descriptive study using an anonymous self-administered 18-item survey sent via Google Forms to students and graduates of a Pediatrics specialty program from Universidad Maimonides in the Autonomous City of Buenos Aires, Argentina.
Results:
Sixty participants completed the survey: 80 % were women, most of them with no children, who were pursuing one of the three years of a specialty program or had less than two years of clinical experience. Out of the respondents, 78.9 % did not usually record information on oral health in the patients’ medical records, and 72 % failed to establish the prevalence of cavities in relation to other childhood illnesses. Misconceptions were also found regarding cavities etiology. A total of 67.2 % have had no prior oral health training, and those who had had such training stated that it had been insufficient. The self-perception to carry out preventive actions was uneven, and difficulties were identified for the early detection of dental disease. Sixty percent were unable to establish the right amount of toothpaste recommended for a child and felt unprepared to offer advice on the right brushing technique. Likewise, in the sample there were no correct and uniform criteria for the first visit of healthy children to pediatric dentists.
Conclusions:
As stated by other authors, deficiencies were found in pediatric graduate students’ and recently graduated pediatricians’ training and, therefore, self-perception of topics related to oral health. Despite the difficulties participants identified, they agreed on the key role pediatricians play in oral health prevention and its impact on children’s quality of life.
Keywords: Oral Health; Pediatrics; Education, Medical; Knowledge
Introduction
Oral and dental health are integral parts of overall good health. Dental caries is very common in childhood and is defined as a disease resulting from an ecological imbalance caused by increased intake of fermentable carbohydrates leading to an imbalance in the composition and activity in the biofilm and mineral loss caused by contact with bacterial acids. Early childhood caries (ECC) affects the teeth of children aged 0 to 5 years. According to the Global Burden of Disease (GBD) study, in 2017, more than 530 million children worldwide had dental caries in baby teeth. Despite this, some professionals did not consider such situation important because, based on their beliefs, milk teeth exfoliate with children’s growth 1. Carious lesions impact individuals, families and societies. The disease affects not only both dentitions but also general health and quality of life. It is related to other common childhood diseases, mainly due to risk factors in common with other non-communicable diseases (NCDs), e.g., high sugar intake, and diseases related to other health conditions such as obesity. Dental caries can lead to abscesses and toothache, which could make chewing and sleeping difficult, thus restricting children’s life activity. Severe dental caries are associated with growth disorders. In addition, caries is an economic burden for families and society since treatment is particularly expensive.
In Argentina, as in many other Latin American countries, there is no continuous oral health monitoring system that provides complete and comparable information to find out the trend of dental caries over time, the distribution of the disease at the population level and the factors that regulate its prevalence 2. A child with severe dental caries may experience chronic oral pain and infection, be malnourished, miss school frequently and suffer from low self-esteem due to missing or defective teeth 3.
Pediatricians, who in their practice interact with pregnant women in the prenatal consultation and with children in their daily practice, play a key role in providing the necessary preventive advice on oral health. This contributes to creating healthy habits rather than correcting harmful habits and already existing dental problems, making dental health education the first and most important pillar of prevention 2,4.
According to the World Health Organization (WHO), the prevalence of oral diseases is one of the main public health problems. Based on recent studies, dental caries affects approximately 90 % of the population in Latin America; the most alarming aspect is that it begins early in life and increases as the individual grows older 5.
Dental caries is a multifactorial process. When studying the subject, biological risk factors are usually addressed and the fact that the family members—especially parents and/or caregivers—are an essential part of future promotion and prevention programs in order to reduce morbidity, disease progression and costs is overlooked 6.
According to the WHO, approaches to ECC prevention and control include changing personal behaviors, working with families and caregivers, and providing public health solutions such as developing health policies, creating enabling environments, promoting health, and orienting health services toward universal health coverage. It is essential to create adequate environments to integrate ECC prevention and control into general health activities. In addition, primary care teams, including community health workers, are crucial to the success of the programs 1.
Social and economic pressures often affect the behaviors and practices of children and their environment, thus generally resulting in poor oral health. The prevalence of ECC is rapidly increasing in lowand middle-income countries 7,8.
Some studies have reported sequelae of the disease such as infection caused by severe caries with pain and abscesses. An infection produces pain and may prevent the child from eating and make it difficult for the child and family to sleep. Severe dental caries is associated with growth disorders 9-11.
Dental caries is the leading cause of tooth loss 5. The American Academy of Pediatrics (AAP) states in its oral health policies and recommendations that pediatricians should learn how to determine the oral health risk in all patients from six months of age 4.
For its part, the WHO, in 2000, proposed that oral health promotion should be a priority in preschool and school children 5. The etiology of ECC is multifactorial and is frequently associated with poor diet and poor oral health habits 2,6,12,15.
Almost all risk factors are modifiable and involve not only the oral cavity but also the child, the family, the social environment and even the health policies. The behaviors and beliefs of the family group influence their diet; to understand the etiology and management of ECC, it is essential to assess the effects of excessive and frequent consumption of free sugars. The importance of establishing good eating habits in childhood to minimize the risk of ECC and obesity cannot be overemphasized. Considering that eating behaviors learned in childhood transfer into adulthood, establishing healthy eating habits in early years is a major goal 1,14.
ECC prevention and control interventions should be included in primary care programs, e.g., maternal and child health programs, immunization and general medical exams. This could lead to continuous interventions that provide confidence to parents and caregivers, thus improving their knowledge of the need to attend medical appointments 15. There are relatively few trained oral health professionals worldwide. Fortunately, most ECC interventions are proven effective, affordable and feasible in places where people usually live. These interventions can be performed by non-oral health specialists in community or primary care settings 1. Carious lesions progress much faster in primary than in permanent teeth, so early detection is crucial to treat ECC and prevent related problems; treatment is also likely to be painless and less expensive 16.
According to Pierce et al., training pediatricians in child oral health can help identify, with an adequate level of accuracy, children with cavitated carious lesions 17. The study results suggest that dental screenings can be easily incorporated into pediatrics practice and significantly contribute to the overall oral health of young children by identifying those who need to be referred to a pediatric dentist.
For all of the above, this study was conducted with the aim of analyzing the behaviors and level of knowledge of pediatric graduate students and pediatricians with less than two years of experience regarding children’s oral health.
Materials and methods
Study design and population
An observational, descriptive and cross-sectional study conducted with an anonymous online questionnaire-type survey sent via Google Forms, whose link was distributed through cell phones. The population consisted of students of the Pediatrics specialty program from Universidad Maimonides in the Autonomous City of Buenos Aires, Argentina, and graduates of said specialization with less than two years of experience.
Variables and measurements
The structured survey included 18 items aimed at analyzing the following variables: sociodemographic data (sex and age), year of training, training history, knowledge and behaviors on oral health (etiology, impact and prevention of dental caries, role of pediatricians in oral health promotion, ability to detect oral problems in children and caregivers, adequate use of toothpaste and first referral to the pediatric dentist).
The instrument was designed by consulting five experts in pediatric dentistry and analyzing updated literature. The survey was tested for comprehension with a pilot group of pediatricians who did not meet the inclusion criteria.
Results
A total of 72 invitations were sent and 60 surveys were obtained (response rate: 83.3%). The general characteristics of the surveyed physicians are presented below (Table 1).
Table 1 Demographic characteristics of respondents
| Characteristic | Percentage | |
|---|---|---|
| Sex | Female | 80.30% |
| Male | 19.70% | |
| Children | No | 62.90% |
| Yes | 37.10% | |
| Level of pediatrics training | Graduates with < 2 years of experience | 32.70% |
| First-year graduate student | 24.60% | |
| Second-year graduate student | 19.70% | |
| Third- to fourth-year graduate student | 23.00% |
Source: self-elaboration.
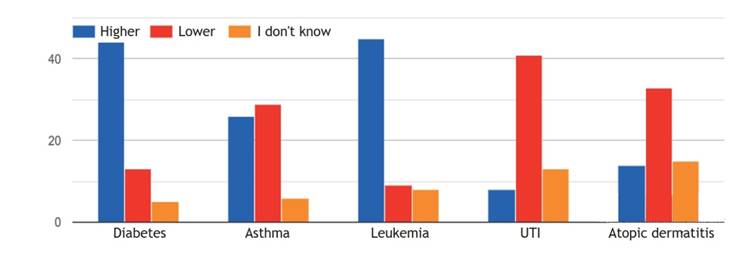
Seventy-two percent of the respondents claim that the prevalence of dental caries in children is higher than that of diabetes and leukemia but lower than that of asthma, urinary tract infection (UTI) and atopic dermatitis. Figure 1 shows how they considered the prevalence of dental caries in relation to other childhood health problems
When inquiring about their training in oral health during the specialty program, 67.20 % answered that they had received no training. The remaining 32.60 % reported having carried out some activity (attending a workshop, taking a tour at a dental office or having spent time watching a dentist at work). However, 72 % said that this learning time was scarce. Concerning their professional practice, 78.90 % responded negatively to whether they found blank spaces in medical histories to include details of the oral health of their patients.
Using a 1-5 scale, where 1 is "not at all confident" and 5 is "very confident," the participants were asked to indicate their self-perception of their ability to conduct different practices related to oral health (Figure 2).

Source: self-elaboration. Used scale: 1 = "not at all confident" and 5 = "very confident."
Figure 2 Self-perception of abilities concerning children’s oral health (OH)
When asked to select the image that showed the right amount of toothpaste that a 2-year-old child should use during brushing, only 40 % answered correctly. A total of 50% of respondents believed that children aged 7 years or older could only brush their teeth without supervision.
As for the risk factors for dental caries, more than 90 % responded that dietary sugar consumption and poor brushing had a great impact, and more than 65 % believed that breastfeeding had almost no influence on the occurrence of dental caries. They ranked the following risk factors in descending order: brushing without toothpaste, non-nutritive sucking (finger, pacifier, etc.), living with family members with caries and genetic factors.
Regarding the age they consider appropriate to recommend the first visit to the dentist, the answers varied and are shown in Figure 3. As for the role of the pediatrician in oral disease prevention and oral health promotion, they answered as follows: inform parents and caregivers of the risks of falling asleep with a bottle (93.30 %), inform that sugary drinks have a negative effect on oral health (100 %), detect teeth with caries (91.60 %), teach parents and caregivers the right tooth brushing technique (85 %), detect dental plaque and enamel demineralization (61 %) and assess parents’ and caregivers’ oral health (56.60 %).

Source: self-elaboration.
Figure 3 Age considered appropriate to recommend the first visit to the dentist
A series of questions were asked to find out pediatricians’ opinion on caries and oral disease in children. Table 2 shows the degree of agreement reported by the respondents.
Table 2 Respondents’ degree of agreement
| Strongly agree | Slightly agree | Undecided | Slightly disagree | Strongly disagree | |
|---|---|---|---|---|---|
| Untreated caries is associated with poorer quality of life in children | 49 | 10 | 1 | - | |
| Poor oral health in childhood leads to social problems in adulthood | 41 | 12 | 7 | - | |
| Pediatricians should be able to apply topical fluoride | 11 | 17 | 6 | 15 | - |
| It is very difficult to detect early caries without special equipment | 17 | 22 | 9 | 8 | 2 |
| Caries is more frequent in high-income population with access to junk food | 24 | 19 | 9 | 4 | 5 |
Discussion
Latest research works conclude that there is a relationship between dietary habits and dental caries and that the prevalence of dental caries can even exceed 90 % in the pediatric population 18.
The research sample consisted of young pediatricians pursuing or recently graduated from a specialty program, mostly females with no children. There was a lack of previous training in child oral health, both in quantity and duration. Although our participants failed to recognize the prevalence of caries in relation to other childhood health problems, they identified dietary sugar and poor brushing as the main risk factors. All this agrees with the findings of Roló et al., who conducted a study in Paraguay 3, as well as with those reported by Carlos-Medrano et al. in Mexico 19 and by Hope et al. in Chile 20.
Medical histories include patients’ written, accurate, clear, organized and detailed information which enables establishing an adequate diagnosis for children’s successful treatment 21. The lack of blank spaces to record data means that these are considered unimportant or unnecessary. Given the prevalence of oral diseases and its impact on health, oral examination should be an essential part of the physical examination and be included in the medical history.
Self-perception to carry out oral health-related activities was high for informing relatives and caregivers that sugary drinks and falling asleep with a bottle have a negative effect on oral health; average for identifying caries; and low for explaining the right brushing technique, identifying plaque and demineralization, and assessing parents’ oral health which is known to be related to that of the child.
Newborns’ oral hygiene should be performed with a gauze and/or silicone finger toothbrush; after the appearance of the first tooth, it should be done using a small toothbrush with fluoridated toothpaste 13. Since young children usually swallow 30 % of the toothpaste, it is important to limit its amount 6 and to supervise the child until approximately 10 years of age 22. In our sample, there was no clear agreement as to the age of first toothpaste use, its right amount according to the age or the need for adult supervision.
The WHO recommends exclusive breastfeeding for the first six months of life. Although human milk lactose is less cariogenic than sucrose, it can also cause demineralization when in contact with tooth enamel for a prolonged period of time and in the absence of salivary protection factors (sleep) 3,12,18,21,23. When evaluating respondents’ knowledge of this risk factor, only a small percentage (14.7 %) considered it as moderate risk, while 68.3 % deemed that it did not influence the appearance of dental caries. This agrees with the findings by Rolón et al., who obtained a percentage of 12 % in their study 3.
There are several predisposing factors to dental caries, which is reflected in the variety of cariogenic factors and habits.
The first visit to the pediatric dentist is extremely important in early childhood since it is necessary to highlight educational and preventive aspects regarding the infant’s oral health. The pediatrician is usually the one who refers the child for the first check-up. Although some specialists recommend a first visit before 6 months of age, as long as the child has no disease that would require an earlier visit, it is generally agreed that the first visit should be before 2 years of age and preferably between 6 and 12 months 3,21. Even though there is no agreement as to the exact age, more than 90 % would refer the child to a pediatric dentist before 2 years of age, which is a higher number than that reported by authors such as Rolón et al. 3 and Contreras-Vásquez et al. 13.
Early dental caries has not only biological but also social and economic consequences. In this regard, Hope et al. 20, in their study conducted in Chile, point out that pediatricians recognize that childhood caries is related to a poorer quality of life and believe that poor oral health in childhood is directly related to social problems in adulthood. However, unlike the Chilean study, the pediatricians in our sample did not agree to apply fluoride varnish during a routine checkup. Moreover, among our findings, there is the misconception that caries affects more high-income populations with access to junk food. It has been shown that children living in poverty, marginalized populations and the elderly are the most affected by oral diseases and, in turn, have little access to dental care 24. Caspary et al., in the United States, conducted a survey of more than 600 pediatricians who were about to graduate and reported that they received little training in oral health. While the participants agreed with performing oral screenings, they perceived a lack of technical skills and resources. The skills for which they felt most trained were informing parents about the harmful effects of sugary drinks and falling asleep with a bottle, while they were less willing to perform tasks requiring more technical training 25.
Pediatricians play a leading role not only in the referral of healthy children but also in the identification of risks and lesions in patients with chronic diseases and greater susceptibility 26,27.
Based on the findings of this study and following a regional and worldwide trend, a mandatory theory-practice training program in oral health was implemented in the curriculum of the graduate program at Universidad Maimónides. Said program is managed by professors working in an interdisciplinary way with the leadership, professors and students of the Pediatric Dentistry specialty with excellent results and high level of satisfaction of the participants 28-30.
When interpreting the results of the present study, it is important to acknowledge the possible limitations. Since this study was conducted with cross-sectional data, the relationship between the level of knowledge and skills of the professionals cannot be determined. As a consequence, causality cannot be tested and it cannot be determined whether the reported practices are reflected in their daily clinical experiences.
In conclusion, pediatric consultation is an excellent opportunity to provide recommendations, detect diseases and refer the patient in a timely manner. It has been demonstrated that pediatricians in Latin America receive poor training in oral health. Although surveyed pediatricians considered caries as an important problem that affects overall health, difficulties, differences in criteria and incomplete registration during medical care were found. Despite recognizing pediatricians’ role in health promotion and disease detection, those surveyed considered that they lacked the tools for correct management.
The findings of this study allowed the development of a graduate training program in response to the deficiencies detected.
REFERENCES
1. Organizacion Mundial de la Salud. Poner fin a la caries dental en la infancia: manual de aplicacion de la OMS [Internet]. Ginebra: Organizacion Mundial de la Salud; 2021. Disponible en: https://apps.who.int/iris/handle/10665/340445 [ Links ]
2. Schafer TE, Adair SM. Prevention of dental disease. The role of the pediatrician. Pediatr Clin North Am [Internet]. 2000;47(5):1021-42. [ Links ]
3. Rolon Lara MC, Samudio M. Conocimiento, actitud y practica de los medicos pediatras sobre factores preventivos de la salud oral en la primera infancia. Pediatr [Internet]. 2017;41(3):191-200. [ Links ]
4. Medina-Aguilar S, Mendoza Roaf PL, Bracamontes-Campoy CE, GalvanSalcedo MG. Nivel de conocimiento y actitud de los pediatras ante la caries dental temprana. Rev Tame [Internet]. 2020;8(24):957-63. [ Links ]
5. Cardozo BJ, Gonzalez MM, Perez SR, Vaculik PA, Sanz EG. Epidemiologia de la caries dental en ninos del Jardin de Infantes ï¿1/2Pinochoï¿1/2 de la ciudad de Corrientes. Revista Facultad de Odontologia [Internet]. 2016;9(1):35-41. [ Links ]
6. Colak H, Dulgergil CT, Dalli M, Hamidi MM. Early childhood caries update: A review of causes, diagnoses, and treatments. J Nat Sci Biol Med [Internet]. 2013;4(1):29-38. [ Links ]
7. Otero G, Pechlaner G, Liberman G, Gurcan E. The neoliberal diet and inequality in the United States. Soc Sci Med [Internet]. 2015;142:47-55. [ Links ]
8. Thomson W. Public health aspects of paediatric dental treatment under general anaesthetic. Dent J [Internet]. 2016;4(2):20. [ Links ]
9. Monse B, Heinrich-Weltzien R, Benzian H, Holmgren C, van Palenstein Helderman W. PUFA: An index of clinical consequences of untreated dental caries. Community Dent Oral Epidemiol [Internet]. 2010;38(1):77-82. [ Links ]
10. Kamran R, Farooq W, Faisal MR, Jahangir F. Clinical consequences of untreated dental caries assessed using PUFA index and its covariates in children residing in orphanages of Pakistan. BMC Oral Health [Internet]. 2017;17(1):108. [ Links ]
11. Khanh LN, Ivey SL, Sokal-Gutierrez K, Barkan H, Ngo KM, Hoang HT, et al. Early childhood caries, mouth pain, and nutritional threats in Vietnam. Am J Public Health [Internet]. 2015;105(12):2510-7. [ Links ]
12. Siquero-Vera KNS, Mattos-Vela MA. Factores de riesgo asociados a caries de infancia temprana severa. Kiru [Internet]. 2018;15(3):146-53. [ Links ]
13. Contreras-Vasquez N, Valdivieso-Vargas MM, Cabello-Morales E. Nivel de conocimientos y practicas de medidas preventivas de profesionales de salud sobre caries dental en el infante. Rev Estomatol Hered [Internet]. 2014;18(1):29-34. [ Links ]
14. Fisher-Owens SA, Gansky SA, Platt LJ, Weintraub JA, Soobader M-J, Bramlett MD, et al. Influences on childrenï¿1/2s oral health: a conceptual model. Pediatrics [Internet]. 2007;120(3):e510-20. [ Links ]
15. Phantumvanit P, Makino Y, Ogawa H, Rugg-Gunn A, Moynihan P, Petersen PE, et al. WHO global consultation on public health intervention against early childhood caries. Community Dent Oral Epidemiol [Internet]. 2018;46(3):280-7. [ Links ]
16. Guedes RS, Piovesan C, Ardenghi TM, Emmanuelli B, Braga MM, Ekstrand KR, et al. Validation of visual caries activity assessment: A 2-yr cohort study. J Dent Res [Internet]. 2014;93(7 Suppl):101S-107S. [ Links ]
17. Pierce KM, Rozier RG, Vann WF Jr. Accuracy of pediatric primary care providersï¿1/2 screening and referral for early childhood caries. Pediatrics [Internet]. 2002;109(5):E82-2. [ Links ]
18. Guerra MH, Desiree RN, Zamudio YC, Hoffman IM. Habitos alimenticios y su relacion con la caries de la primera infancia. Rev AMOP. 2018;30(2):60-7. [ Links ]
19. Carlos-Medrano LE, Luengo Fereira JA, Toscano Garcia I, Luevano Bueno AP, Anaya Alvarez M. Conocimientos, creencias y percepcion de universitarios mexicanos sobre caries temprana de la infancia. Acta Univ [Internet]. 2017;27(2):46-52. [ Links ]
20. Hope Lopez B, Zaror Sanchez C, Vergara Gonzalez C, Diaz Melendez J, Bustos Medina L. Conocimientos y actitudes de los pediatras chilenos sobre salud oral. Int J Odontostomatol [Internet]. 2013;7(2):245-51. [ Links ]
21. Pinto JM, Chavez DB, Navarrete C. Salud bucal en el primer ano de vida. Revision de la literatura y protocolo de atencion odontologica al bebe. Odous Cientifica [Internet]. 2018;19(1):60-72. [ Links ]
22. Dos Santos APP, Nadanovsky P, de Oliveira BH. A systematic review and meta-analysis of the effects of fluoride toothpastes on the prevention of dental caries in the primary dentition of preschool children. Community Dent Oral Epidemiol [Internet]. 2013;41(1):1-12. [ Links ]
23. De la Luz Ayala Carmen. Los pediatras en la prevencion de enfermedades bucales. Arch Pediatr Urug [Internet]. 2016;87(3):257-62. [ Links ]
24. Pistochini A. Ensenanza de Odontopediatria en el entorno actual. Odontol Sanmarquina [Internet]. 2022;25(3):e23213. [ Links ]
25. Caspary G, Krol DM, Boulter S, Keels MA, Romano-Clarke G. Perceptions of oral health training and attitudes toward performing oral health screenings among graduating pediatric residents. Pediatrics [Internet]. 2008;122(2):e465-71. [ Links ]
26. Arrieta-Blanco JJ, Bartolome-Villar B, Jimenez-Martinez E, SaavedraVallejo P, Arrieta-Blanco FJ. Problemas bucodentales en pacientes con diabetes mellitus (I): Indice de placa y caries dental. Med Oral [Internet]. 2003;8:97-109. [ Links ]
27. Molina Lopez S, Frausto Esparza S, Aceves Medina MC, Aguilera Galaviz LA. Algunas implicaciones de la enfermedad periodontal en las enfermedades cronicas no transmisibles. Contexto odontologico [Internet]. 2015;5(9):1-9. [ Links ]
28. Ramos-Gomez F, Askaryar H, Garell C, Ogren J. Pioneering and interprofessional Pediatric Dentistry programs aimed at reducing oral health disparities. Front Public Health [Internet]. 2017;5:207. [ Links ]
29. Palma Fernandez JC. Odontologia para pediatras. Curso de Actualizacion [Internet]. Actualizacion en pediatria; 2015. Disponible en: https://www.aepap.org/sites/default/files/cursoaepap2015p207-212.pdf [ Links ]
30. Reynolds EC. Transdisciplinary research: The virtuous cycle of research translation to improve oral health. J Dent Res [Internet]. 2022;101(6):613-5. [ Links ]
Received: June 22, 2023; Revised: June 28, 2023; Accepted: July 07, 2023











 texto em
texto em