Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Horizonte Médico (Lima)
versão impressa ISSN 1727-558X
Horiz. Med. vol.23 no.3 Lima jul./set. 2023 Epub 13-Set-2023
http://dx.doi.org/10.24265/horizmed.2023.v23n3.10
Case report
Midbrain stroke syndrome: Weber’s syndrome in two male HIV-positive patients with cerebral toxoplasmosis
1Hospital María Auxiliadora, Department of Neurology. Lima, Peru.
2Universidad de San Martín de Porres, School of Human Medicine. Lima, Peru.
This report describes the case of two male HIV-positive patients who were not receiving treatment and whose diagnosis was confirmed by serology testing. Both patients developed midbrain stroke syndrome and the structural injury, which was caused by a central nervous system infection due to cerebral toxoplasmosis, was verified by brain magnetic resonance imaging. This condition was confirmed by cerebrospinal fluid serology testing.
Weber’s syndrome is a very rare type of midbrain stroke syndrome with little information available on its symptoms and evolution. It was first described by Sir Herman David Weber in 1863 and is characterized by ipsilateral injury of the third cranial nerve fascicle with contralateral hemiparesis due to injury of the corticospinal and corticobulbar tracts of the cerebral peduncle. Its causes range from ischemic or hemorrhagic processes, which damage the third cranial nerve fascicle and cerebral peduncle, to brain tumors, aneurysms, extradural hematomas and infectious diseases that behave like spreading processes.
The assessed patients showed clinical signs and symptoms such as ptosis; vertical double vision; difficulty standing up; hemiparesis; hyporeflexia; decreased superficial and deep sensation; poor balance and coordination; third cranial nerve palsy; slurred speech; intermittent disorientation in time, place and person; and facial asymmetry. Oral trimethoprimsulfamethoxazole, clindamycin and prednisone were administered as specific treatment for toxoplasmosis, which enabled the improvement of the clinical picture.
This case report presents the sequence of events, treatment and a brief review of the literature to be considered in the diagnosis and determine its importance in patients with HIV-toxoplasmosis of the central nervous system.
Keywords: Brain Stem Infarctions; HIV; Toxoplasmosis
Introduction
Midbrain stroke syndrome, described by Sir Herman David Weber in 1863, is characterized by ipsilateral injury of the third cranial nerve fascicle with contralateral hemiparesis due to injury of the corticospinal and corticobulbar tracts of the cerebral peduncle 1,2. Its causes range from ischemic or hemorrhagic processes, which damage the third cranial nerve fascicle and cerebral peduncle, to brain tumors, aneurysms, extradural hematomas and infectious diseases that behave like spreading processes 3,4.
Toxoplasmic encephalitis is the most frequent opportunistic infection that affects the central nervous system (CNS) of 26 % of patients with HIV/AIDS and is associated with multiple focal injuries in the brain 5.
The criteria to diagnose cerebral toxoplasmosis are based on histology testing and laboratory tests to determine the definitive diagnosis—along with the signs and symptoms shown by patients and the injury evidenced by neuroimaging. Nevertheless, the presumptive diagnosis is more frequently based only on the signs and symptoms of patients, compatible injuries found with neuroimaging and the radiological response within 10-14 days after the empirical start of the anti-toxoplasma treatment 6. In these two cases we will describe the clinical presentation of two male HIV-positive patients with CNS toxoplasmosis
in the Department of Neuroinfectious Diseases at Instituto Nacional de Ciencias Neurológicas (INCN, National Institute of Neurological Sciences) in Lima, Peru.
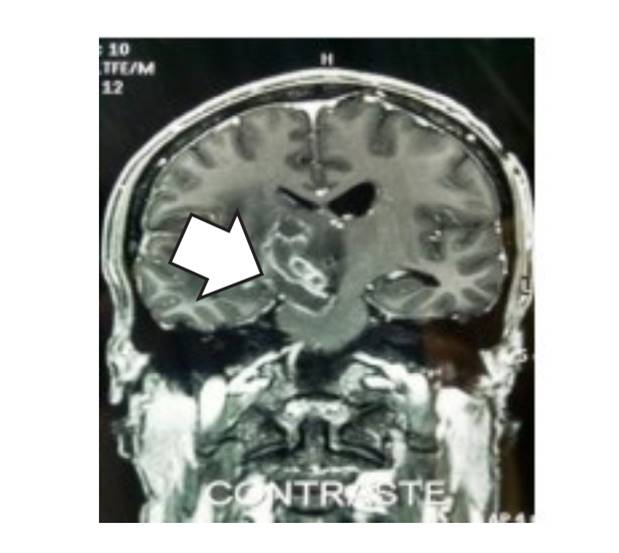
Clinical case I
This is the case of a 28-year-old male patient recently diagnosed with HIV, without antiretroviral therapy. He was admitted to the hospital with the following symptoms: ptosis of the right eyelid, vertical double vision, dragging of the left foot, inability to keep standing, left hemiparesis (muscle strength: upper limb 2/5, lower limb 2/5), left hypotony, deep tendon reflexes (DTRs): left hyporeflexia (+/++), decreased left superficial and deep sensation, poor balance and coordination, third cranial nerve palsy (75 %), 5 mm right pupil unreactive to light and absence of consensual pupillary reflex. A contrast-enhanced magnetic resonance imaging (MRI) scan showed an image compatible with cerebral toxoplasmosis (Figure 1). Moreover, cerebrospinal fluid (CSF) serology testing for cerebral toxoplasmosis using chemiluminescence (IMMULITE 2000 Immunoassay System) found IgM antibodies > 1.1 with "reactive" result, which revealed an active infection. Therefore, a protocol-based treatment was prescribed at the institution and recovery was observed; the patient made good progress and his symptoms improved.
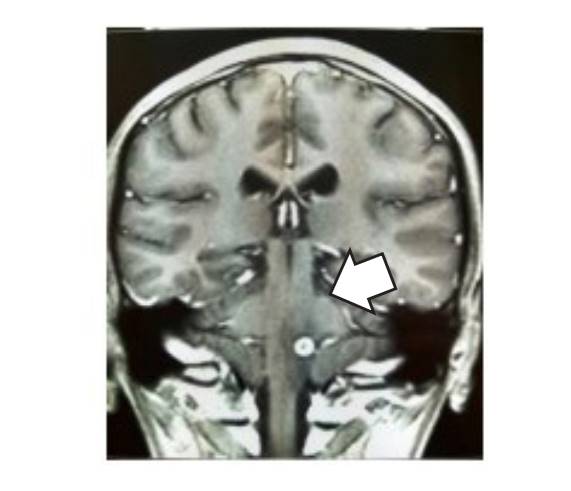
Clinical case II
This is the case of a 40-year-old male patient diagnosed with HIV about a year before, without antiretroviral therapy and without controls. He went to the hospital because he had presented ptosis of the right eyelid and slurred speech for approximately four days. The assessment determined intermittent disorientation in time, place and person; left facial asymmetry; left hemiparesis (4/5); left hyporeflexia (++/+++); decreased sensation in the left hemibody; absence of meningeal signs; third cranial nerve palsy; 3.5 mm right pupil hyporeactive to light; disfluency and slurry speech. A contrast-enhanced MRI scan showed an injury compatible with cerebral toxoplasmosis (Figure 2). Moreover, CSF serology testing for cerebral toxoplasmosis using chemiluminescence (IMMULITE 2000 Immunoassay System) found IgM antibodies > 1.1 with "reactive" result, which revealed an active infection. Therefore, a protocolbased treatment was prescribed at the institution and recovery was observed; the patient made good progress and his symptoms improved.
Discussion
HIV-seropositive patients may suffer many opportunistic infections, and cerebral toxoplasmosis is one of the most frequent in the CNS with a rate of about 26 %, particularly in countries with a high burden of infection and limited access to antiretroviral therapy 5,7. In most of the cases in which patients live with HIV, cerebral toxoplasmosis manifests clinically with an HIV viral load over 50 copies/ml and CD4+ cell count < 100/mm3 8. The brain is one of the tissues preferred by toxoplasma because of its low inflammatory reaction and, in most cases, cerebral toxoplasmosis occurs because of the reactivation of a latent infection 9,10. Midbrain injuries that cause ipsilateral palsy of the third cranial nerve and hemiplegia or contralateral hemiparesis are characteristic of Weber’s syndrome 11,12.
The occurrence of stroke syndromes in the context of HIV and cerebral toxoplasmosis is quite rare since their onset manifests with very specific symptoms such as homolateral ophthalmoplegia and contralateral palsy of the lower face, tongue, arm and leg. The palsy of the medial rectus muscle causes ptosis of the upper eyelid; if the Edinger-Westphal nucleus is damaged, the pupil will be dilated and fixed to light and accommodation because of the damage to the third cranial nerve 2-4. The possible etiologies of Weber’s syndrome are compression injuries of the interpeduncular fossa such as meningeal diseases, midbrain infarctions, aneurysms, brain tumors or infections, as shown in the cases presented in the literature, in which patients had CNS infection caused by cerebral toxoplasmosis with damage to the midbrain and the third cranial nerve 6,13.
The patients received alternative and standard treatment established by the Ministry of Health of Peru. The following scheme was used: trimethoprim (TMP) 320 mg-sulfamethoxazole 1,600 mg bid, and clindamycin 600 mg every six hours for at least six weeks (duration could be extended if the clinical and imaging responses were incomplete after six weeks). In the clinical cases presented, the patients showed significant improvement between the sixth and eighth week since the onset of their neurological signs and symptoms. Also, they started highly active antiretroviral therapy (HAART) and were followed up for six months with maintenance therapy for toxoplasmosis until their CD4+ cell count improved 14,15. These cases show the importance of considering midbrain stroke syndrome as a probable diagnosis in the context of an HIV infection and CNS toxoplasmosis, and making a correct diagnosis for the prompt treatment to minimize the possible sequalae.
REFERENCES
1. Palacio M, Nunez T, Montiel K, Ferrer Y, Finol F, Parra M. Sindrome de Weber hemorragico: a proposito de un caso. Revista Latinoamericana de Hipertension [Internet]. 2012;7(2):45-7. [ Links ]
2. Serra Valdes MA, Serra Ruiz M, Comas Valdespino R. Infarto isquemico mesencefalico: sindrome de Weber. Rev Cubana Med [Internet]. 2018;57(3):43-9. [ Links ]
3. Montalvo Herdoiza JP, Montalvo Perero PS, Moreira Vera DV. Sindrome de Weber, etiologia infrecuente y resolucion espontanea. Rev Ecuat Neurol [Internet]. 2015;24(1):1-3. [ Links ]
4. Adeva Bartolome MT, Gomez Sanchez JC, Marcos Toledano M, Ciudad Bautista J, Fermoso Garcia J. Triple asociacion de sindromes mesencefalicos. Rev Neurol [Internet]. 1999;28(4):403-4. [ Links ]
5. Duran E, Mirazo I, Combol A. Toxoplasmosis cerebral en pacientes con sida. Parasitol al dia [Internet]. 1997;21(3-4):1213-8. [ Links ]
6. Vidal JE. HIV-related cerebral toxoplasmosis revisited: Current concepts and controversies of an old disease. J Int Assoc Provid AIDS Care [Internet]. 2019;18(1):1-20. [ Links ]
7. Pacheco PRG, Zara ALSA, Silva e Souza LC, Turchi MD. Late onset of antiretroviral therapy in adults living with HIV in an urban area in Brazil: Prevalence and risk factors. J Trop Med [Internet]. 2019;2019:5165313. [ Links ]
8. Seo H, Han H, Lee S, Hong S, Cho S, Kim S, et al. Modelling Toxoplasma gondii infection in human cerebral organoids. Emerg Microbes Infect [Internet]. 2020;9(1):1943-54. [ Links ]
9. Wang Z, Wang S, Liu H, Ma H, Li Z, Wei F, et al. Prevalence and burden of Toxoplasma gondii infection in HIV-infected people: a systematic review and meta-analysis. Lancet HIV [Internet]. 2017;4(4):e177-88. [ Links ]
10. Dian S, Ganiem AR, Ekawardhani S. Cerebral toxoplasmosis in HIV-infected patients: a review. Pathog Glob Health [Internet]. 2023;117(1):14-23. [ Links ]
11. Parija S, Lalitha CS, Naik S. Weber syndrome secondary to brain stem tuberculoma. Indian J Ophthalmol [Internet]. 2018;66(7):1036-9. [ Links ]
12. Khalil M, Malik TG, Farooq K. Weberï¿1/2s syndrome with vertical gaze palsy. J Coll Physicians Surg Pak [Internet]. 2009;19(10):668-9. [ Links ]
13. Lizarazo J, Castro F, de Arco M, Chaves O, Pena Y. Infecciones oportunistas del sistema nervioso central en pacientes con VIH atendidos en el Hospital Universitario Erasmo Meoz, Cucuta, 19952005. Infectio [Internet]. 2006;10(4):226-31. [ Links ]
14. Instituto Nacional de Ciencias Neurologicas. Guia de Practicas Clinicas del paciente neurologico con infeccion por el virus de la inmunodeficiencia humana (VIH) sida - Aspectos Generales y Toxoplasmosis del Sistema Nervioso e Infeccion por el virus de la Inmunodeficiencia Humana (VIH) [Internet]. Ministerio de Salud. 2016. Disponible en: https://www.incn.gob.pe/wp-content/uploads/2020/09/RD._037-2016_Aprobar_Gu%C3%ADa_de_practica_clinica_de_Enf_Transmisibles.pdf [ Links ]
15. Konstantinovic N, Guegan H, Stajner T, Belaz S, Robert-Gangneux F. Treatment of toxoplasmosis: Current options and future perspectives. Food Waterborne Parasitol [Internet]. 2019;15(e00036):e00036. [ Links ]
Received: February 23, 2023; Revised: March 27, 2023; Accepted: April 10, 2023











 texto em
texto em