Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Horizonte Médico (Lima)
versão impressa ISSN 1727-558X
Horiz. Med. vol.23 no.4 Lima out./dic. 2023 Epub 18-Dez-2023
http://dx.doi.org/10.24265/horizmed.2023.v23n4.09
CASE REPORT
Complex rotational atherectomy in an elderly female patient with multivessel coronary artery disease. A case report
1Universidad de Caldas. Manizales, Caldas, Colombia.
Rotational atherectomy is a specific procedure for managing complex coronary artery lesions, especially when there is coronary artery calcification (CAC). This technique was widely used until the last decade of the 20th century; however, although it is rarely used, it currently plays an important role in patients who could be candidates for surgical revascularization but reject surgeries due to different pathologies-such as diffuse atheromatous disease requiring long stents, in-stent restenosis, calcified ostial lesions and chronic total occlusions. Rotational atherectomy is a method that uses a diamond-coated burr to reduce the volume of atherosclerotic plaques and calcification of vessels. This device breaks up plaque into microfragments, leading to an increase in lumen diameter. These fragments, which have a tiny diameter, pass predominantly into the capillary circulation and are then absorbed by the reticuloendothelial system. Among the complications of this technique are arterial dissection, device entrapment, bradycardia and microperforation of coronary arteries. The latter can be corrected with the use of thrombin, subcutaneous fat or beads. This article reports the case of an elderly female patient with multivessel coronary artery disease associated with extensive calcification of all the coronary arteries secondary to radiotherapy received in previous years for breast cancer. The patient, not being a candidate for cardiovascular surgery, required a rotational atherectomy that resulted in a microperforation of a coronary artery but with good subsequent progress.
Keywords: Atherectomy, Coronary; Vascular Calcification, Coronary Disease
Introduction
Rotational atherectomy (RA) is a specific technique to treat complex lesions, particularly those with heavy calcification that cannot be properly dilated with conventional ballons or stents, leading to the rupture of the former and subexpansion of the latter 1. Differently from the percutaneous transluminal coronary angioplasty (PTCA), this technique removes part of the obstructive atheroma through differential cutting. Consequently, rotation is associated with less deep wall injury; therefore, the results may be better in the short and long term 2. The use of RA has decreased since the end of the 1990s, when it was used in approximately 10 % of percutaneous coronary interventions (PCI) in the United States. More recent records show that the use of RA account for < 1 % of the cases of PCI in the United Kingdom and 1.35 % in people over 65 years old in a large register of the USA 3. This is the case of an 80-year-old female patient with multivessel coronary artery disease and extensive calcified coronary circulation due to a history of radiation therapy. For this reason, it required RA and the insertion of drug-eluting stents.
Clinical case
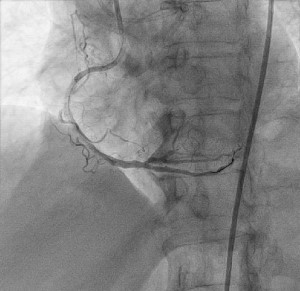
A 80-year-old female patient with type 2 diabetes mellitus, hypertension, dyslipidemia and breast cancer for 6 years (with indication of radiation therapy) was admitted to the hospital due to thoracic pain with typical characteristics. The physical examination showed stable vital signs and no respiratory distress or signs of pulmonary or systemic congestion. Biomarker analysis and electrocardiogram were caried out: the results were negative for acute ischemia. The electrocardiogram showed a normal left ventricular ejection fraction (LVEF), dilated left atrium, absence of contractility disorders and mild to moderate mitral insufficiency. A coronary angiography revealed a left coronary artery without significant obstructive lesions, calcified lesion in 70 % of the proximal third of the anterior descending artery and 70 % of the middle third of such artery, totally occluded middle third of the right coronary, severely calcified vessel and total occlusion of the posterolateral artery. Also, multivessel coronary disease was diagnosed; the assessment by cardiovascular surgery was requested, but there was no possibility of such surgical procedure due to calcification throughout the coronary arteries. Later, a coronary angiography was carried out, with permeabilization of the anterior and posterior descending artery through RA and the insertion of a drug-eluting stent (Figure 1 and Figure 2). Microperforation of the posterolateral artery was reported during the process, but it was possible to correct it in the same surgical intervention using microparticle embolism. Following the intervention, the patient showed good clinical progress and was discharged.
Discussion
RA is indicated in the event of coronary artery calcification (CAC), which is the most frequent pathology of the coronary arteries. The procedure is also indicated in diffuse atheromatous disease that requires long stents, in-stents restenosis as well as in calcified ostial lesions and chronic total occlusions 4. Since RA avoids plaque prolapse or shifting, it could be especially useful in bifurcation lesions, which allows better preservation of the side branches 5. The use of RA has decreased since the end of the 1990s, when it was used approximately in 10 % of PCIs in the United States. More recent records show that the use of RA account for < 1 % of PCIs in the United Kingdom and 1.35 % of patients over 65 years old in a large register in the USA 3.
CAC is influenced by various factors such as age, sex, diabetes mellitus, hypertension and chronic renal disease 6. Our patient had two of such risk factors, and also had a history of radiation therapy for breast cancer. According to the BACCARAT study, this treatment increases the risk of CAC, particularly of the anterior descending artery because it is the most exposed vessel 7. CAC can be measured by imaging procedures such as electron beam computed tomography, and there is an association between its severity and mortality 8.
RA is a specific technique to treat complex lesions, particularly those with heavy calcification that cannot be properly dilated with conventional balloons or stents, leading to the rupture of the former or sub-expansion of the latter. RA induces lumen enlargement by the physical removal of plaque, generates microfragments and reduces plaque rigidity, facilitating proper dilation 1. As these resulting fragments are small, they pass to capillary circulation, and are absorbed by the reticuloendothelial system 9,10. The combination of RA and stent therapy has been associated with the highest revascularizationfree survival rate of the target lesion as well as highest event-free survival rate after nine months (85.4 % and 85.4 %, respectively). The final minimum lumen diameter of the treated lesion was the only significant independent predictor of event-free survival 11.
Concerning the application of this process in elderly patients, Dahdouh et al. conducted a study in a group of patients with indication of surgical revascularization but without the possibility of carrying it out because they had CAC. They showed that RA is safe, does not an involve an increased risk of renal injury compared to PCI without RA, and has a significant effectiveness rate 12, regardless of the fact whether the radial of femoral approach is used 13.
Complications of this procedure include coronary perforation or rupture, slow flows, entrapment or disconnection of the burr and ostial right coronary artery lesions 14. The perforation caused by the burr is the most serious complication of RA, and the incidence is about 1 %. The risk of perforation largely depends on the characteristics of the lesion such as the vessel tortuosity or calcification eccentricity. In general, it is considered that the risk of perforation is greater in eccentric calcification such calcified nodules compared to a concentric calcification as the so-called "napkin-ring sign." The selection of the right burr size and RotaWireMR are important to prevent perforation. The use of intravascular imaging devices would help operators to select the optimal size of burr and RotaWireMR 15.
REFERENCIAS BIBLIOGRÁFICAS
1. Iannopollo G, Gallo F, Mangieri A, Laricchia A, Erriquez A, Tzanis G, et al. Tips and tricks for rotational atherectomy. J Invasive Cardiol [Internet]. 2019;31(12):376-83. [ Links ]
2. Dill T, Dietz U, Hamm CW, Kuchler R, Rupprecht HJ, Haude M, et al. A randomized comparison of balloon angioplasty versus rotational atherectomy in complex coronary lesions (COBRA study). Eur Heart J [Internet]. 2000;21(21):1759-66. [ Links ]
3. Couper LT, Loane P, Andrianopoulos N, Brennan A, Nanayakkara S, Nerlekar N, et al. Utility of rotational atherectomy and outcomes over an eight-year period: RA Treats Complex Lesions With Low Procedural Complications and MACE Rates. Catheter Cardiovasc Interv [Internet]. 2015;86(4):626-31. [ Links ]
4. Gruberg L, Mehran R, Dangas G, Hong MK, Mintz GS, Kornowski R, et al. Effect of plaque debulking and stenting on shortand long-term outcomes after revascularization of chronic total occlusions. J Am Coll Cardiol [Internet]. 2000;35(1):151-6. [ Links ]
5. Mota P, de Belder A, Leitao-Marques A. Rotational atherectomy: Technical update. Rev Port Cardiol [Internet]. 2015;34(4):271-8. [ Links ]
6. Sharma V, Abdul F, Haider ST, Din J, Talwar S, Oï¿1/2Kane P, et al. Rotablation in the very elderly safer than we think? Cardiovasc Revasc Med [Internet]. 2021;22:36-41. [ Links ]
7. Honaryar MK, Allodji R, Ferrieres J, Panh L, Locquet M, Jimenez G, et al. Early coronary artery calcification progression over two years in breast cancer patients treated with radiation therapy: Association with cardiac exposure (BACCARAT study). Cancers [Internet]. 2022;14(23):5724. [ Links ]
8. Budoff MJ, Lane KL, Bakhsheshi H, Mao S, Grassmann BO, Friedman BC, et al. Rates of progression of coronary calcium by electron beam tomography. Am J Cardiol [Internet]. 2000;86(1):8-11. [ Links ]
9. Ahn SS, Auth D, Marcus DR, Moore WS. Removal of focal atheromatous lesions by angioscopically guided high-speed rotary atherectomy. Preliminary experimental observations. J Vasc Surg [Internet]. 1988;7(2):292-300. [ Links ]
10. Self SB, Coe DA, Normann S, Seeger JM. Rotational atherectomy for treatment of occluded prosthetic grafts. J Surg Res [Internet]. 1994;56(2):134-40. [ Links ]
11. Hoffmann R, Mintz GS, Kent KM, Pichard AD, Satler LF, Popma JJ, et al. Comparative early and nine-month results of rotational atherectomy, stents, and the combination of both for calcified lesions in large coronary arteries. Am J Cardiol [Internet]. 1998;81(5):552-7. [ Links ]
12. Dahdouh Z, Roule V, Dugue AE, Sabatier R, Lognone T, Grollier G. Rotational atherectomy for left main coronary artery disease in octogenarians: transradial approach in a tertiary center and literature review: Rotational atherectomy for left main coronary artery. J Interv Cardiol [Internet]. 2013;26(2):173-82. [ Links ]
13. Watt J, Oldroyd KG. Radial versus femoral approach for high-speed rotational atherectomy. Catheter Cardiovasc Interv [Internet]. 2009;74(4):550-4. [ Links ]
14. Sakakura K, Ito Y, Shibata Y, Okamura A, Kashima Y, Nakamura S, et al. Clinical expert consensus document on rotational atherectomy from the Japanese association of cardiovascular intervention and therapeutics. Cardiovasc Interv Ther [Internet]. 2021;36(1):1-18. [ Links ]
15. Januszek R, Siudak Z, Dziewierz A, Dudek D, Bartus S. Predictors of in-hospital effectiveness and complications of rotational atherectomy (from the ORPKI Polish National Registry 2014-2016). Catheter Cardiovasc Interv [Internet]. 2018;92(4):278-87. [ Links ]
Received: July 14, 2023; Revised: July 31, 2023; Accepted: August 07, 2023











 texto em
texto em