Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO - Veja o fascículo
Compartilhar
Horizonte Médico (Lima)
versão impressa ISSN 1727-558X
Horiz. Med. vol.23 no.4 Lima out./dic. 2023 Epub 18-Dez-2023
http://dx.doi.org/10.24265/horizmed.2023.v23n4.10
Corrige o artigo: 10.24265/horizmed.2024.v24n1.16
CASE REPORT
Insulinoma: a case report of a successful resective surgery
1Hospital Nacional Arzobispo Loayza. Departamento de Cirugía General (General Surgery Service). Lima, Peru.
2Universidad de San Martín de Porres, School of Human Medicine. Lima, Peru.
Insulinoma is a pancreatic neuroendocrine tumor that produces hyperinsulinism and causes a severe lowering of blood glucose levels with chronic symptoms such as fainting. It is more common in males and can occur at any age, either as solitary or multiple neoplasms, the latter known to be part of the multiple endocrine neoplasia, type 1 (MEN 1) group. Insulinomas are rare and require resective surgery, with symptoms resolution being the marker of recovery. This article describes a case of insulinoma in a 51-year-old woman with a clinically typical presentation and signs and symptoms of hyperinsulinism. Laboratory tests revealed increased insulin secretion, while magnetic resonance imaging showed features of insulinoma, where the pancreatic tumor could be seen. This case was treated by surgical resection of the pancreatic tumor during an exploratory laparotomy, using the enucleation technique, which is described in detail herein. There were no intraoperative or postoperative complications, i.e., the result was successful in terms of health recovery. This surgical technique is used at Hospital Nacional Arzobispo Loayza in Lima, Peru, when facing cases such as the one described. This type of neoplasm is very uncommon, so it should be considered highly suspicious and, in this case, the images were essential for choosing the surgical resection. Other cases of insulinoma have been treated surgically at the Hospital; moreover at least one case of nesidioblastosis could not receive an adequate treatment.
Keywords: Insulinoma; Hyperinsulinism; Pancreas; Neoplasms
Introduction
Insulinoma is the most frequent pancreatic endocrine tumor. About one to four cases per million have been reported every year 1. It is more common in males and can occur at any age 2. It is usually benign and made up of a mass with a diameter of less than 2 cm. Insulinomas can also occur as multiple neoplasms (10 % of the cases), which are associated with the multiple endocrine neoplasia syndrome, type 1 (MEN 1). The symptoms are unspecific; therefore, treatment initiation usually delays. Patients frequently show signs of hypoglycemia because insulinomas secrete insulin 3. After clinical confirmation of hyperinsulinism, imaging staging—which is usually complicated—is carried out. The curative treatment for insulinoma is resective surgery, in spite of the fact that surgical localization is usually a diagnostic dilemma if there are not devices to perform an intraoperative ultrasound.
This case report describes the treatment for insulinoma at Hospital Nacional Arzobispo Loayza in Lima.
Clinical case
A 51-year-old female patient who went to Hospital Loayza in March 2012. She had been sick for two years, and her disease was characterized by fainting, particularly at night after dinner. There was not a history of pancreatic diseases in her family. When she was admitted to the hospital, she had hypoglycemia—with a blood sugar level of 50 mg/dl—and for this reason she underwent insulin testing, the result of which was 80 IU (range 25 IU higher). She was prescribed prolonged fasting, and hypoglycemia associated with hyperinsulinism was observed. In addition, the C-peptide level was elevated. An MRI scan was carried out (Figure 1), which revealed a nodular lesion in the anterior side of the pancreas with a diameter of approximately 2 cm. Hormones such as cortisol and thyroid hormone were measured to rule out MEN syndrome.
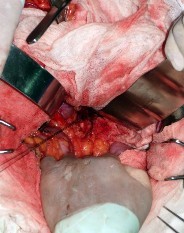
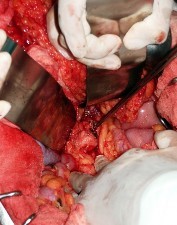
The patient underwent open surgery with a mediumsized supraumbilical incision, which allowed opening the omental bursa (Figure 2). The lesion could be observed directly; therefore, more intraoperative images were not required. Bimanual palpation of the pancreas was carried out applying an extended Kocher maneuver to assess the lesion depth.
The punch biopsy technique was applied to remove the lesion, then silk suture was used (Figure 3) as anchorage, and the nodular lesion was removed with a monopolar electrocautery (Figure 4). The result was absolute hemostasis (Figure 5). Finally, the omental bursa was closed, and the cavity was then closed using a single layer closure without drains.
The surgeon removed a 2 cm tumor (Figure 6), which was sent to the laboratory, and the anatomopathological diagnosis was insulinoma. The glucose level normalized, and the patient did not show hyperinsulinism during the postoperative period or subsequent controls; therefore, she was discharged: on the sixth day without complications.
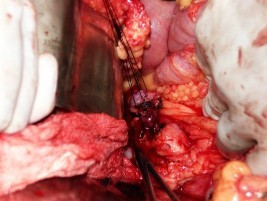
Figure 4 Removal of insulinoma with punch biopsy technique and unipolar electrocautery in spray mode
The patient was followed-up for four years following the surgery. There was no evidence of symptoms of hyperinsulinism, and radiologic examinations did not show recurrence.
Discussion
Insulinomas are very rare tumors that have an unspecific clinical presentation. When reviewing different autopsies, the rate of silent insulinomas observed was 0.8 to 10 % 4-7. When there are symptoms, patients usually have confusion, behavioral changes, visual disturbances, weakness, vertigo, syncope, fatigue, obtundation, seizures, among others 8,9. Insulinomas are responsible for 70 to 75 % of the cases of hyperinsulinism 10-12. An MRI scan has proven very useful in tumor localization in 47 % of cases, with a mean sensitivity of 45 % 13,14.
This case shows clinical signs and symptoms that clearly suggest insulinoma. The diagnostic tests were appropriate, and the possibility of multiple endocrine neoplasia was ruled out. It is very rare to find this type of tumors by imaging; however, in this case the neoplasm could be identified very clearly (Figure 1). This improves the conditions for resective surgery, which when associated with appropriate surgical maneuvers such as an adequate bimanual palpation and wide enucleation, may predict good prognosis.
The partial success of insulinoma resection in Hospital Arzobispo Loayza can be mentioned, among other experiences. Moreover, there has been at least one case of nesidioblastosis 15, for which the proper treatment could not be administered to the patient.
REFERENCIAS BIBLIOGRÁFICAS
1. Okabayashi T, Shima Y, Sumiyoshi T, Kozuki A, Ito S, Ogawa Y, et al. Diagnosis and management of insulinoma. World J Gastroenterol. 2013;19(6):829-37. [ Links ]
2. Bouslama K, Maghrebi H, Bedioui H, Bouslama K. Lï¿1/2insulinome pancreatique: approche diagnostique et modalites therapeutiques. J Afr Hepatol Gastroenterol. 2014;8:11-5. [ Links ]
3. Patel S, Narwari M, Parekh D, Shah V. Insulinoma: case report and review of diagnostic and treatment modalities. J Assoc Physicians India. 2013;61(6):423-6. [ Links ]
4. Shin JJ, Gorden P, Libutti SK. Insulinoma: pathophysiology, localization and management. Future Oncol. 2010;6(2):229-37. [ Links ]
5. Service FJ, McMahon MM, O'Brien PC, Ballard DJ. Functioning insulinoma incidence, recurrence, and long-term survival of patients: a 60-year study. Mayo Clin Proc. 1991;66(7):711-9. [ Links ]
6. Halfdanarson TR, Rabe KG, Rubin J, Petersen GM. Pancreatic neuroendocrine tumors (PNETs): incidence, prognosis and recent trend toward improved survival. Ann Oncol. 2008;19(10):1727-33. [ Links ]
7. Sada A, Glasgow AE, Vella A, Thompson GB, McKenzie TJ, Habermann EB. Malignant insulinoma: a rare form of neuroendocrine tumor. World J Surg. 2020;44(7):2288-94. [ Links ]
8. Abboud B, Boujaoude J. Occult sporadic insulinoma: localization and surgical strategy. World J Gastroenterol. 2008;14(5):657-65. [ Links ]
9. Cryer PE. Symptoms of hypoglycemia, thresholds for their occurrence, and hypoglycemia unawareness. Endocrinol Metab Clin North Am. 1999;28(3):495-500. [ Links ]
10. Rostambeigi N, Thompson GB. What should be done in an operating room when an insulinoma cannot be found? ClinEndocrinol (Oxf). 2009;70(4):512-5. [ Links ]
11. Gramatica L, Herrera MF, Mercado-Luna A, Sierra M, Verasay G, Brunner. Videolaparoscopic resection of insulinomas: experience in two institutions. World J Surg. 2002;26(10):1297-300. [ Links ]
12. Christ E, Iacovazzo D, Korbonits M, Perren A. Insulinomatosis: new aspects. Endocr Relat Cancer. 2023;30(6):e220327. [ Links ]
13. Hirshberg B, Libutti SK, Alexander HR, Bartlett DL, Cochran C, Livi A, et al. Blind distal pancreatectomy for occult insulinoma, an inadvisable procedure. J Am Coll Surg. 2002;194(6):761-4. [ Links ]
14. Pellegrino F, Granata V, Fusco R, Grassi F, Tafuto S, Perrucci L, et al. Diagnostic management of gastroenteropancreatic neuroendocrine neoplasms: technique optimization and tips and tricks for radiologists. Tomography. 2023;9(1):217-46. [ Links ]
15. Dravecka I, Lazurova I. Nesidioblastosis in adults. Neoplasma. 2014;61(3):252-6. [ Links ]
Received: June 22, 2023; Revised: July 10, 2023; Accepted: July 20, 2023; corrected: January 01, 2024











 texto em
texto em