Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Liberabit
Print version ISSN 1729-4827
liber. vol.22 no.1 Lima jan./jun. 2016
ARTICLE
Diagnosis and treatment of ADHD: criteria used by different professional categories
Diagnóstico y tratamiento de TDAH: criterios usados por diferentes categorías profesionales
Laura Aragão*, Daniele Leôncio**, João Alencar***, Priscila Andrade de Sousa****, Jorge Falcão***** e Izabel Hazin******
*, **, ***, ****, *****, ****** Universidade Federal do Rio Grande do Norte, Brasil
* lauraclaragao@gmail.com **** priscilaandrade.psi@hotmail.com ** danicarolly@hotmail.com ***** falcao.jorge@gmail.com *** joaocarlos.alencar@hotmail.com ****** izabel.hazin@gmail.com
ABSTRACT
This study aimed to investigate the diagnostic criteria and intervention proposals related to ADHD in different professional categories from the city of Natal, RN, Brazil. In the study participated 34 professionals conveniently selected and a semi-structured interview was conducted with them. After the categorization of information we proceeded to a multidimensional descriptive Cluster analysis. There was an evident division of the whole group into two other groups due to three bigger relevance variables: education, number of sessions used in the diagnosis, and the use of formal instruments. Group 1, formed by physicians, was characterized by the use of two to three sessions and by the use of instruments and formal scales. In Group 2, the average number of sessions was higher than three and all psychologists and most educational psychologist from this group did not use formal scales for diagnosis. We suggest that the academic training determines the diagnostic modalities and intervention modalities for ADHD.
Keywords: Attention Deficit Hyperactivity Disorder, diagnosis, treatment
RESUMEN
Este estudio tuvo como objetivo investigar los criterios diagnósticos y propuestas de intervención relacionados al TDAH de diferentes categorías profesionales en la ciudad de Natal – RN, Brasil. Participaron 34 profesionales seleccionados por conveniencia y a quienes se les realizó una entrevista semi-estructurada. Luego de la categorización de las informaciones se procedió al análisis descriptivo multidimensional de tipo Clusters. Se hizo evidente la división de la muestra total en otros dos grupos en relación a las tres variables de mayor relevancia: educación, número de sesiones utilizadas en el diagnóstico y uso de instrumentos formales. El Grupo 1, formado por médicos, se caracterizó por la utilización de dos o tres sesiones y por el uso de instrumentos y escalas formales. En el grupo 2, el número promedio de sesiones fue superior a tres y todos los psicólogos y la mayoría de los psicopedagogos no utilizaron escalas formales en el diagnóstico. Se sugiere que la formación académica determina las modalidades diagnósticas y de intervenciones utilizadas junto al TDAH.
Palabras clave: Trastorno por déficit de atención con hiperactividad, diagnóstico, tratamiento.
Introduction
Attention Deficit Hyperactivity Disorder (ADHD) is among the most common disorders in childhood, occurring in approximately 5 % of children (American Psychiatric Association, 2013). Despite a large body of scientific evidence attesting the neurobiological nature of ADHD (Couto, Melo-Junior & Gomes, 2010; Gallagher & Rosenblatt, 2013; Kieling, Goncalves, Tannock & Castellanos, 2008; National Health and Medical Research Council, 2012; Pajo & Cohen, 2013; Tarver, Daley & Sayal, 2014; Tripp & Wickens, 2009), the disorder has been the focus on important critical disputes, especially regarding its legitimacy, diagnostic effectiveness and therapeutic effectiveness.
The controversy surrounding ADHD seems associated, among other aspects, to the heterogeneity of the symptom expression due to the stages of development, together with the influence of cultural aspects; symptoms showed by individuals diagnosed as ADHD become pathological because of changes in temporality and intensity (American Psychiatric Association, 2013), being at the same time related to contextual, social and moral aspects that modulate the impact of these symptoms in the child’s or teenager’s lives.
In addition, studies suggest that the vagueness of its etiological factors could be at the root of the lack of agreement regarding specific diagnosis tools (Brzozowski & Caponi, 2012; Caliman, 2009). The absence of biological markers connected to the occurrence of ADHD, like genetic aspects and specific brain structures, forces diagnosis process to be mostly clinical, directly connected to the knowledge of the professional responsible for establishing the stages and procedures to be used.
As a result, it is evident that the diversity of methodological practices in the assessment process, namely, the use of diagnostic criteria, the evaluation of life impairment, the source of obtained information, and the employment of instruments and techniques, like scales, neuropsychological evaluation and exams, tends to have a significant influence on ADHD prevalence rates (American Psychiatric Association, 2013; Bunte, Schoemaker, Hessen, van der Heijden & Matthys, 2013; Graeff & Vaz, 2008; Polanczyk, Willcutt, Salum, Kieling & Rohde, 2014).
The variation of the diagnosis criteria complicates the definition of the disorder as a clinical category with homogeneous dimensions in etiological and prognostic terms. This seems to be directly associated to the professionals’ education and upbringing, which lead them to used different approaches involved in the diagnosis process, especially in terms of differences among theoretical perspectives underlying the curriculum of each type of professional education (Peixoto & Rodrigues, 2008).
Concerning medical practice area, aspects related to the patient’s integral care are still considered as peripheral to the central target of Medicine, facing obstacles from practionners (Alves, Moreira, Azevedo, Rocha & Vilar, 2009; Amorim & Araújo, 2013; Rios, 2010). Clinical Psychology, on its turn, is characterized by many epistemological attitudes, leading to a divided approach of the human subject – sometimes disconnecting him from his sociocultural and political context, sometimes dissociating his behavior and cognitive processes from brain, anatomical substrates and neurophysiological mechanisms (Azzi, 2010; Paiva & Yamamoto, 2010). Last but not less important point, professionals issued from Psycho-pedagogy, also involved in ADHD diagnosis, sometimes propose a treatment allowing a «pedagogical cure» of isolated clinical cases (Andrade, 2004), other times take into account the global comprehension of learning and its difficulties in the context of the relationship the individual establishes with school, family and society (Fernandes & Viana, 2009).
Based on the above considerations, the objective of this study was to evaluate the diagnosis criteria and intervention proposals related to ADHD from different professional categories in the city of Natal, in northeastern Brazil. The following specific objectives stand out: (a) investigate whether there are specific associations between education and theoretical conception of ADHD; (b) investigate whether there are specific associations between education and diagnosis modality used for ADHD; and (c) investigate whether there are specific associations between education and the intervention modalities used in the treatment of ADHD.
The following working hypotheses were formulated: (a) Physicians, psychologists and educational psychologist have different conceptions and make different contributions for ADHD diagnosis; (b) Physicians, psychologists and educational psychologist have different conceptions on ADHD intervention.
Method
Firstly, the research project was approved by the Research Ethics Committee of Onofre Lopes University Hospital – CEP/HUOL, and all participants gave authorization to their participation in the study through the signing of the Informed Consent Form and Voice Recording Authorization.
Participants
Thirty-four health professionals participated in the study. They belonged to four groups: 9 psychiatrists, 10 clinical psychologists, 10 educational psychologist (with degrees mainly in Languages and Pedagogy) and 5 neurologists, all of them work in the city of Natal and were selected without random assignment, by convenience.
With the goal of composing a sample calculation for the composition of the medical professional group, we used the website of the Regional Council of Medicine to identify the total amount of neurologists, neuropediatricians and psychiatrists, specialized in childhood and adolescence. However, when performing the procedure, no professional was identified using the filters «Pediatric Neurology», «Neuropediatrics» and «Childhood Psychiatry». A new procedure was performed by using more general filters, namely «Neurology» and «Psychiatry». As a result, a total of twenty-eight neurologists and fifty-four psychiatrists were identified. The next step was a phone research, which allowed the identification of the professionals, who directly provided service and monitored children and adolescents, and gave information about the composition of the group of professionals as well.
The same procedure was performed to compose the sample calculation of psychology professionals. However, when contacting the Regional Council of Psychology, we identified 2781 psychologists in the city, which were not defined in terms of active and not active, or regarding specialty and practice areas. Thus, it was yet again impossible to compose the sample calculation of these participants, and phone research was used to compose the group.
It is important to note that educational psychology is not a regulated profession and, therefore, there is no reference on the total number of professionals in the city; thus, we used a similar strategy to that adopted for the composition of the other groups.
The sample of physicians, psychologists and educational psychologist was composed with the professionals from the attendance network in Natal who service children and adolescents and who met the inclusion and exclusion criteria, namely: (a) At least one year of experience in child and adolescent clinical practice; (b) History of servicing patients of school age who presented a diagnostic hypothesis of ADHD; (c) Working in only one of the practice areas considered in this study.
Measures
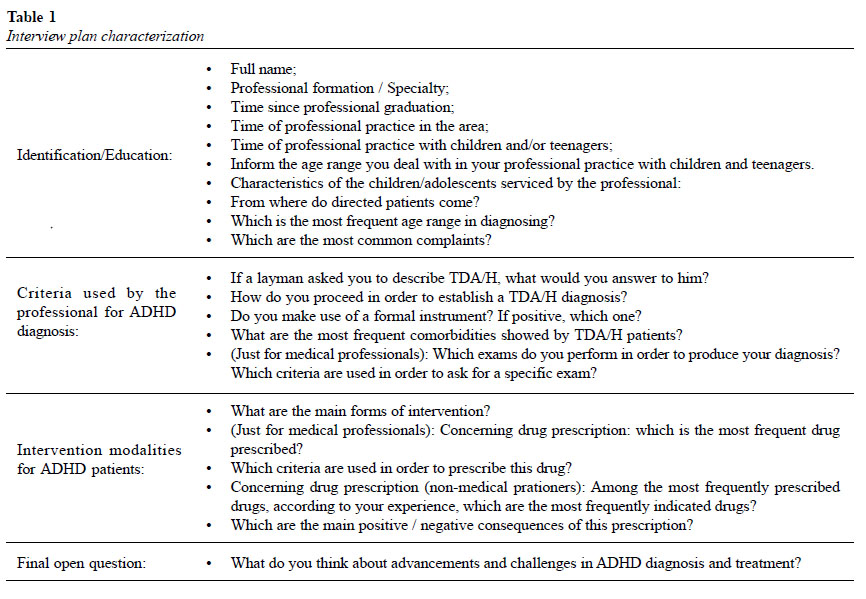
For the data collection procedure, we used a research plan created by the researcher, composed of semi-open questions, distributed in four distinct thematic sessions. Questions are shown in the Table 1.
The interview plan was submitted for analysis by judges, namely, 2 neuropaediatricians, 3 psychologists, 4 educational psychologists and 2 speech therapists. All professionals were specialists in the clinical and research areas of ADHD and members of a reference child neuropsychology service. We asked for an evaluation of the plan regarding the appropriateness of the terms used based on the target population, clarity of questions, incentive for engagement of the interviewee in answers, and the ability to reach the proposed objective (Belei, Gimeniz-Paschoal, Nascimento & Matsumoto, 2008).
We performed individual interviews with the professionals in their workplaces, with an approximate duration of thirty minutes. As previously stated, the participants were recruited with information available on Internet, contact with child and adolescent clinics and services in the city of Natal, and referral of professionals by the participants of the study.
Data analysis
After the transcription of the answers provided by the participants and a careful reading of the material in order to verify its reliability, we started the information categorization stage. We chose to elaborate the categories a posteriori, constructed from the report of the professionals interviewed, identifying recurring content inside the thematic lines that composed the interview plan.
Subsequently, we used a multidimensional descriptive analysis of the Cluster type with the objective of grouping information contained in the category-descriptive variables, in order to obtain group characteristics that could be interpreted by the researcher. Statistical analyses of the data were performed with the aid of the Statistical Package for the Social Sciences (SPSS 21.0) software.
Results
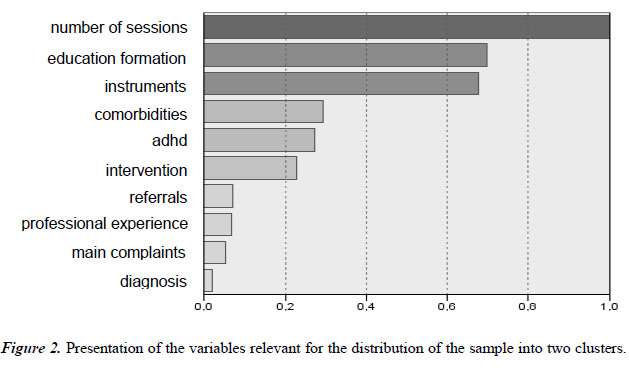
The multidimensional descriptive analysis of the Cluster type spanned eleven variables common to all participants of the study, namely: «Education», «Length of professional experience», «Source of referrals», «Age group at the moment of diagnosis», «Main complaints related to ADHD», «Criteria used for ADHD characterization», «Diagnosis criteria for ADHD», «Use of formal instruments», «Number of sessions needed for ADHD diagnosis effectuation or ADHD hypothesis indication», «Comorbidities associated to ADHD», and «ADHD intervention modalities».
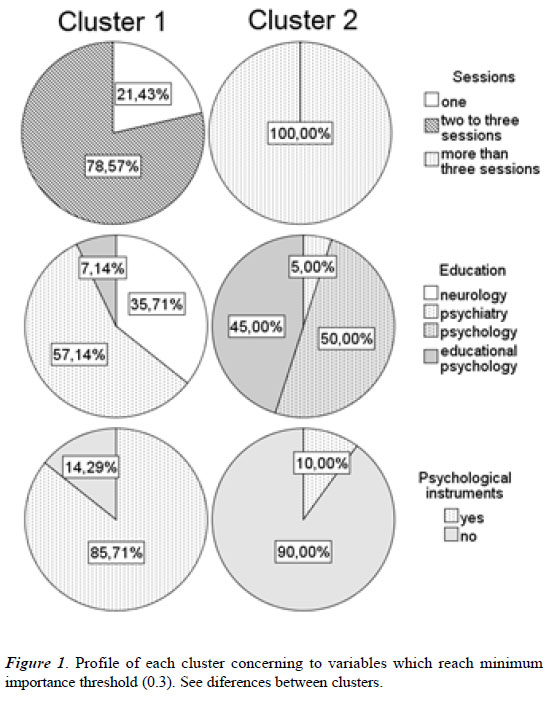
The analysis evidenced a set of variables relevant for the division of the whole group into two groups composed by 41.2 % (Group 1) and 58.8 % (Group 2) of the whole sample, without losses, that is, without any subject not included in one of the two groups. It was a division with a reasonable cluster quality, in which the measurement of the cohesion and separation silhouette was equal to 0.3 (Figure 1).
We considered the variable with a minimal importance threshold close to 0.3 (in an interval from 0.0 to 1.0, with a usual minimum index of 0.5). Thus, we have verified that the variable with the largest segmentation force was «Number of sessions needed for ADHD diagnosis effectuation or ADHD hypothesis indication», followed by «Education» and «Use of formal instruments».
Globally, by analyzing the segmentations of the clusters, it was possible to characterize them, thus constructing profiles for each one. Group 1 was predominantly composed by medical professionals, namely, neurologists (100 %) and psychiatrists (88.9 %). These professionals are strongly connected by similar answers to specific categories. The first one is related to the average number of two to three sessions performed by most professionals of that group (78.6 %) for ADHD diagnosis. Secondly, such professionals (72.7 %) tend to characterize ADHD by integrating etiological and symptomatology characteristics. This group (85 %) is equally characterized by the use of formal scales and instruments as auxiliary methods for diagnosis evaluation. Finally, they indicated more frequently (100 %), when compared with the other professionals that they identify the presence of other disorders comorbid with ADHD. After diagnosis consolidation, most of the neurologists and psychiatrists (64.3 %) reported that they suggested interventions targeted both to the child or adolescent and to their family and school contexts.
Group 2, on the other hand, it was comprised mostly by psychologists and educational psychologist (100 % and 90 %, respectively). For these professionals (100 %), the average number of sessions usually performed for the consideration of ADHD diagnosis is higher than three. All psychologists and most educational psychologist (80 %) participating in the research do not use formal scales as a tool for the diagnostic analysis of the disorder.
The large majority of psychologists and educational psychologist (85 %) defined ADHD from its symptomatology or etiological characteristics to the detriment of the association between these aspects. In general, it was a group that wanted to identify comorbidities associated with ADHD, although the non- identification of comorbid presentations was frequent between these professionals (40 %). Regarding intervention modalities, most of the psychology and educational psychologist (95 %) suggest integrated therapies that is, directed to the child or adolescent and to the other contexts in which they live, namely, family and school.
Discussion
The main objective of this study was to investigate how different professional categories, physicians, psychologists, and educational psychologists have performed or contributed to ADHD diagnosis and how do they conceive ADHD intervention for children and adolescents.
We have noticed that the professional categories and the particularities that underlie the education regarding the conception of subject, mental disorders and its consequences (Amorim & Araujo, 2013; Azzi, 2010; Bueno, 2011; Freire & Tavares, 2011; Paiva & Yamamoto, 2010; Rios, 2010) seem significantly related to the variation in diagnostic and therapeutic conceptions for ADHD adopted by physicians, psychologists and educational psychologists. Likewise, the inconsistencies on several dimensions of the disorder, namely, disputes its origin and empirical validity, also suggest the absence of methodological and interventional standardization (Mallett, Natarajan & Hoy, 2014).
The study indicates that the medical professionals from the city of Natal, Brazil, characterized ADHD from the articulation of etiological and symptomatological aspects, conceiving the disorder as having a neurobiological nature. Clinical psychologists and educational psychologists, in turn, characterized the disorder predominantly from symptomatological characteristics. These findings are consistent with the study by Missawa and Rossetti (2014), in which the psychologists answer «disorganization», «damage», «agitation» and «difficulty with self-control» as first evoked words by ADHD.
In addition, physicians and educational psychologists have reported integrated socio-behavioral and learning aspects as the main complaints associated with ADHD, while psychologists presented mostly sociobehavioral complaints. These results seem related to the specificities in the conception of subject associated to each professional area, which corroborates the previous hypothesis that clinical psychologists tend to emphasize behavioral, affective and social aspects instead of the biological aspect (Azzi, 2010).
On the other hand, specificities regarding the «Diagnosis criteria for ADHD» were also identified among the professional categories. Most psychologists and educational psychologists usually evaluate and raise the diagnostic hypothesis of ADHD in a number of sessions higher than the number of sessions performed by physicians. We also stress that only neurologists and psychiatrists stated that they performed the ADHD diagnosis in one single session. These finding are in line with previous results (Missawa & Rossetti, 2014; Peixoto & Rodrigues, 2008).
The stance adopted by some medical professionals suggests that they remove themselves from the complexity underlying the disorder, which makes difficult the judicious analysis of the symptoms and its consequences for the academic and social life of the child or adolescent (Palomino, 2014). Furthermore, it increases the risk of inaccurate treatments, since quick diagnoses increase the chances of an indiscriminate use of medication (Hinshaw & Scheffler, 2014).
Another diagnostic criterion that significantly distinguished the professional categories was the use of formal instruments. Most physicians stated that they used structured scales for assistance in the diagnosis process of ADHD, as opposed to all psychologists and most educational psychologists, who stated that they did not use these tools. SNAP-IV appeared more frequently in the answers by the medical professionals. This questionnaire is similar to the list of ADHD symptoms from the DSM-IV, including the same behavioral observations, namely, absent-mindedness, hyperactivity and impulsiveness (Posserud et al., 2014).
These findings are consistent with the general data found by Peixoto and Rodrigues (2008), in a study that involved psychiatrists, neurologists and psychologists. In this study, the most used diagnostic instruments were: anamnesis, psychological evaluation, intelligence evaluation and questionnaires (i.e. Conners Scale). However, the results of the study were not presented in a segmented way. This impedes the investigation on the association between the professional category and the use of diagnostic criteria.
In turn, Missawa and Rossetti (2014) have identified that all the psychologists interviewed used clinical observation as a diagnosis instrument. In addition to observation, some psychologists used scales and questionnaires, while others used games. However, none of the psychologists requested complementary exams.
In addition, we verified that medical professionals enumerated a much higher number of comorbidities associated to ADHD when compared to the other professional categories. The presence of comorbidities was considered one of the most representative criteria for the choice of medicine in the therapeutic process.
The results presented to date, especially regarding the stages for the diagnostic consolidation of ADHD, suggest that medical professionals tend to comply with the diagnostic criteria from the reference manuals. This stance is discussed by Azzi (2010), who argues that medical diagnosis is guided by the schematic knowledge of the diseases, for example, its set of symptoms which, in turn, guides the investigation of the characteristics of the individual. In addition, as pointed out by Missawa and Rossetti (2014), it is necessary to stress that psychologists lack systematization both in diagnosis and treatment of ADHD.
Regarding the «ADHD intervention modalities», globally, the need for integration between therapeutic, individual and contextual strategies was significant between the professionals who participated in the study, especially for clinical psychologists and educational psychologists, which corroborates the recommendation of the multimodal nature of its treatment (Palomino, 2014).
We stress that the answers that mentioned intervention modalities restricted to therapeutic and pharmacological treatments, although little significant, were given only by the physicians. For Brzozowski and Caponi (2013), this stance increases the risk of indiscriminate medication use, which contributes for the defense of those who argue that the body of the individual is the only focus of problems that should be solved, without considering the impact of the disorder for the social and academic contexts in which the child or adolescent is. This stance is close to the logic that underlies the medical education — for which the organic aspects are a priority in relation to psychosocial aspects when understanding mental disorders (Brzozowski & Caponi, 2013).
From the above considerations, it is important to state that diagnostic errors will invariably cause therapeutic errors. Thus the absence of physical exams that prove the presence of the disorder requires an effort by the professional in the sense of considering its comprehensiveness and heterogeneity, not only in the biological aspect — bearing in mind the quantity of structure and brain function factors that comprise it — but also in the sociocultural, cognitive emotional and behavioral aspects (Pajo & Cohen, 2013).
In addition, to take as a basis the neurodevelopmental character of ADHD and, consequently, its symptom variability during the child’s development, it allows for the qualitative analysis of the symptoms, which can be identified early, which makes possible the use of combined interventions that is, with and without medicine, thus reducing the chances of symptom exacerbation or future academic and social dysfunctions (Ruiz, 2012; Schmiedeler & Schneider, 2014).
By way of conclusion, despite the findings described above, we highlight that the general results of this study suggest that the professionals from the city of Natal involved in ADHD evaluation and intervention conceive the disease as a multideterminate disorder, which expresses the interconnection of biological, behavioral and sociocultural factors. Consequently, they advocate the consideration of judicious steps, composing a complex evaluation for functional analysis and analysis of intensity of symptoms and its developmental course.
Finally, we highlight that a significant limitation of this study is the small sample of the medical category, namely, psychiatrists and neurologists. This is justified by the scarcity of professionals from those areas that focus on the children and adolescents in the city of Natal.
Furthermore, we stress the need for further studies to identify the diagnostic criteria and intervention criteria used by different professionals, either in terms of country regions, or in terms of comparison between regions, since Brazil is characterized by a great cultural and socioeconomic variation.
That said, we point out that the data from this study may help the decision-making in terms of local and national public policies, as well as serve as a base for debates regarding the curricula offered for the different professional categories, filling gaps and indicating specific continuous training demands.
References
Alves, A. N. de O., Moreira, S. da N. T., Azevedo, G. D. de., Rocha, V. M. da., & Vilar, M. J. (2009). A humanização e a formação médica na perspectiva dos estudantes de Medicina da UFRN – Natal – RN – Brasil. Revista Brasileira de Educação Médica, 33(4), 555-561.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Autor.
Amorim, K. P. C. & Araújo, E. M. de. (2013). Formação Ética e Humana no Curso de Medicina da UFRN: Uma Análise Crítica. Revista Brasileira de Educação Médica, 37(1), 138-148.
Andrade, M. S. de. (2004). Rumos e diretrizes dos cursos de psicopedagogia: análise crítica do surgimento da psicopedagogia na América-Latina. Cadernos de Psicopedagogia, 3(6), 70-71.
Azzi, E. (2010). A situação atual da profissão de psicólogo no Brasil. In O. H. Yamamoto & A. L. F. Costa (Orgs.), Escritos sobre a profissão de psicólogo no Brasil (pp. 105-120).
Natal, RN: EDUFRN. Belei, R. A., Gimeniz-Paschoal, S. R., Nascimento, E. N., & Matsumoto, P. H. V. R. (2008). O uso de entrevista, observação e videogravação em pesquisa qualitativa. Cadernos de Educação, 30, 187-199.
Brzozowski, F. S. & Caponi, S. N. C. de. (2012). Determinismo biológico e as neurociências no caso do transtorno de déficit de atenção com hiperatividade. Revista de Saúde Coletiva, 22(3), 941-961.
Brzozowski, F. S. & Caponi, S. N. C. de. (2013). Medicalização dos desvios de comportamento na infância: Aspectos positivos e negativos. Psicologia: Ciência e Profissão, 33(1), 208-221.
Bueno, R. (2011). Reflexiones acerca del objeto y metas de la Psicología como ciencia natural. Liberabit, 17(1), 37-48.
Bunte, T. L., Schoemaker, K., Hessen, D. J., van der Heijden, P. G., & Matthys, W. (2013). Clinical usefulness of the Kiddie-Disruptive Behavior Disorder Schedule in the diagnosis of DBD and ADHD in preschool children. Journal of Abnormal Child Psychology, 41(5), 681-690.
Caliman, L. V. (2009). A constituição sócio-médica do «Fato TDAH». Psicologia & Sociedade, 21(1), 135-144.
Couto, T. de S., Melo-Junior, M. R. de., & Gomes, C. R. de A. (2010). Aspectos neurobiológicos do transtorno do déficit de atenção e hiperatividade (TDAH): Uma revisão. Ciência & Cognição, 15(1), 241-251.
Fernandes, T. L. G. & Viana, T. V. (2009). Alunos com necessidades educacionais especiais (NEEs): Avaliar para o desenvolvimento pleno de suas capacidades. Estudos em Avaliação Educacional, 20(43), 305-318.
Freire, T. & Tavares, D. (2011). Influência da autoestima, da regulação emocional e do gênero no bem-estar subjetivo e psicológico de adolescentes. Revista de Psiquiatria Clínica, 38(5), 184-188.
Gallagher, R. & Rosenblatt, J. L. (2013). Attention-Deficit/ Hyperactivity Disorder predominantly inattentive type. In L. A. Reddy, A. S. Weissman, & J. B. Hale (Eds.), Neuropsychological assessment and intervention for youth: An evidence-based approach to emotional and behavioral disorders (pp. 155-176). Washington, DC: American Psychiatric Association.
Graeff, R. L. & Vaz, C. E. (2008). Avaliação e diagnóstico do transtorno de déficit de atenção e hiperatividade (TDAH). Psicologia USP, 19(3), 341-361.
Hinshaw, S. P. & Scheffler, R. M. (2014). The ADHD explosion: Myths, medication, money, and today’s push for performance. New York: Oxford University.
Kieling, C., Goncalves, R. F., Tannock, R., & Castellanos, F. X. (2008). Neurobiology of Attention Deficit Hyperactivity Disorder. Child and Adolescent Psychiatric Clinics of North America, 17(2), 285-307.
Mallett, C. A., Natarajan, A., & Hoy, J. (2014). Attention Deficit/ Hyperactivity Disorder: A DSM timeline review. International Journal of Mental Health, 43(4), 36-60.
Missawa, D. D. A. & Rossetti, C. B. (2014). Psicólogos e TDAH: Possíveis caminhos para diagnóstico e tratamento. Construção Psicopedagógica, 22(23), 81-90.
National Health and Medical Research Council. (2012). Clinical practice points on the diagnosis, assessment and management of attention deficit hyperactivity disorder in children and adolescents. Commonwealth of Australia. Recuperado de www.nhmrc.gov.au/guidelines/publications/mh26
Paiva, I. L. de. & Yamamoto, O. H. (2010). Formação e prática comunitária do psicólogo no âmbito do «terceiro setor». Estudos de Psicologia, 15(2), 153-160.
Pajo, B. & Cohen, D. (2013). The problem with ADHD: Researchers’ constructions and parents’ accounts. International Journal of Early Childhood, 45(1), 11-33.
Palomino, D. (2014). Trastorno por déficit de atención e hiperactividad (TDAH): Nuevos critérios diagnósticos. El farmacéutico: Profesión y Cultura, 508, 10-19.
Peixoto, A. L. B. & Rodrigues, M. M. P. (2008). Diagnóstico e tratamento de TDAH em crianças escolares, segundo profissionais da saúde mental. Aletheia, 28, 91-103.
Polanczyk, G. V., Willcutt, E. G., Salum, G. A., Kieling, C., & Rohde, L. A. (2014). ADHD prevalence estimates across three decades: An updated systematic review and metaregression analysis. International Journal of Epidemiology, 43(2), 434-442.
Posserud, M., Ullebo, A. K., Plessen, K. J., Stormark, K. M., Gillberg, C., & Lundervold, A. J. (2014). Influence of assessment instrument on ADHD diagnosis. European Child & Adolescent Psychiatry, 23(4), 197-205.
Rios, I. C. (2010). Humanidades e medicina: Razão e sensibilidade na formação médica. Ciência & Saúde Coletiva, 15(1), 1725-1732.
Ruiz, E. (2012). TDAH, hacia una concienciación, implicación y abordaje común. Revista AOSMA, 15. Recuperado de http://dialnet.unirioja.es/servlet/oaiart?codigo=4054735
Schmiedeler, S. & Schneider, W. (2014). Attention-deficit hyperactivity disorder (ADHD) in the early years: Diagnostic issues and educational relevance. Clinical Child Psychology and Psychiatry, 19(3), 460-475.
Tarver, J., Daley, D., & Sayal, K. (2014). Attention-deficit hyperactivity disorder (ADHD): An updated review of the essential facts. Child: Care, Health and Development, 40(6), 762-774.
Tripp, G. & Wickens, J. R. (2009). Neurobiology of ADHD. Neuropharmacology, 57(7-8), 579-589.
* Universidade Federal do Rio Grande do Norte, Brasil
Recibido: 28 de octubre de 2015
Aceptado: 11 de abril de 2016