INTRODUCTION
The correct function of the mental health system is useful for decreasing the burden of mental disorders. It has allocated 13 percent of the world burden of disease that will increase to 15 percent in 20301. Based on evaluations of world mental health organization, the govern of mental health, financial sources, giving suitable services- human's sources and information are necessary bases for correct working of the mental health system in every country. And their duty is to do the useful functions to decrease the mental disorders2. Each mental health system needs to collect, analyze, evolve and feedback about its own information. Therefore, in the innovative project for evaluating the sociological mental health in Canada (CMHEI), different groups of individuals and organizations are out broken; for example, the governments, the social servers, families and service users. The study provides evidence that proper decision has been made on the future of mental health and support services. The findings of this study help to appoint that, which one of the studied organizations that have effective functions, will help to the study. This study evaluates the effectiveness and supportable services about mental health, based on the community it provides for supporting of future decides about plans and giving suitable services3.
The continuous mental health evaluation initiatives project (CEQM) was another project that has been done based on appointing some criteria for evaluating the primary mental health services in Canada. The target of this plan is to extol the mental health services quality for all Canadians and it follows by promoting and deployment assay qualification, and to determine some quality indexes of the mental health initial tendencies. These indexes can be used for attempting to extol the quality on different levels of the health system, for example, the functional level4. Similar to other countries, there are also extensive studies in Iran about the challenges, opportunities and barriers to mental health promotion in the health system. Which can be noted in the studies of Bakhshani et al, as well as Malek Afzali and Dawasaz Irani5,6 7 8 9 10 11 12. Also, some research activities have been done about effectiveness and costs for extreme depressed and epileptic patients13,14 15. Another important study was an evaluation of clients and families. Satisfaction, from received services16 and satisfaction rate of patients in psychological centers for mental health, from cure connector's role in Iran17. Also, Bolhari & et al have evaluated the mental health affrical program on the initial health care site. In Iran18, Shariat et al have done the program of awareness, views and satisfaction of clients and employers, that are under care the mental health services affricate in PHC19 as it is shown, each country should have an own clear image of mental health system, that the world health organization has presented an instrument called (WHO-AIMS) for evaluating and helping to extol the mental health. This instrument includes 6 domains, 28 subsets and 156 indexes. The domains are:
1. Policy, plans, and legislation
2. Mental health services.
3. Mental health in primary health care (PHC).
4. Human resources.
5. Public education and links with other sectors.
6. Monitoring and research2,20.
Now, there will be a question: can this instrument evaluate the mental health system for all countries or all country states as equal by notice to all problems, that there are for mental health system, and, all targets of the world health organization and the targets of Action plan in 2013- 2020 are included in it? And are the mental health problems shown by this instrument for evaluating the mental health system in Iran? Considering the existence of operational and operational problems in achieving the goals of the World Health Organization in the Mental Health Program 2013-2020.
OBJECTIVES
The present study was aimed at extracting components for the development of mental health system assessment tools.
MATERIALS AND METHODS
Study method and research area
This cross-sectional descriptive study was done both qualitatively and quantitatively; in the quantitative phase, the cross-sectional descriptive method was applied for assessing Khuzestan mental health system and in the qualitative phase, the opinion of the employees and experts was taken into consideration. The research population included the practitioners of human sources of Khuzestan domain (mental health managers, nurses, psychologists, psychoanalysts), that evaluated the survey about WHO-AIMS.
Study design
In this level, the main instrument was given to the people and they answered to 11 questions that they were confirmed by experts as contentive designed, and they replied to them as "Yes" or "No". Also, as contentive replied of replyers to the 3-point Likert scale: 1- Agree 2- No idea 3- Correct or delete. The domain of subsets and instrument indexes were evaluated and by looking at abundant percent and average repliers answers, they deleted or corrected or isolated some of them.
Also, they asked 10 question boxes by Yes or No and one open-ended question about each domain that finally they showed which domain needs to be changed. Sampling was as census and the questioner was distributed among people that they returned 143. Also, interview with the mental health manager of Khuzestan about weakness and power of instrument and the quality data were collected about the mental health domain in Khuzestan.
Also, the researcher studied the Action plan in 2013- 2020 of the world health organization and the gap of mental health in countries and mental health system programs in Iran and other countries (from 2010- 2017) were studied and each characteristic of the study was changed to some description for each domain, Content Validity Ratio (CVR), Content Validity Indexes (CVI) for them. In this level, 13 experts (10 people of mental health experts and 1 person of mental health managers and 2 people that they had experiences of making instrument) were asked to judge the dialectics. Based on the 3-point Likert scale: 1-it is not required 2-it is useful 3-it is required.
Calculating and analyzing the findings
The replies were calculated based on formulation number 1 and based on Lavsheh chart: some of them that were with content validity ratio less than %51 were deleted (Lavsheh, 1975). After CVR rate calculation with a group of expert's offer, the dialectic have given to experts to calculate narrative index again, and wanted them to suggest about each dialect based on, Likert an 4 parts group 1-not related 2-it is a little related 3-it is related 4-completely related, and this rate was calculated by using of Content Validity Index and after calculation this rate, if the score of dialectic in questioner was more than or equal to 79 percent, that was kept in the questioner. If this score was between 70 and 79, it was corrected and if it is less than 70 percent, it was deleted.
Finally, 11 main components were identified and 95 questions were designed for them. In the sixth phase, these questions were provided to mental health managers for exploratory and confirmatory factor analysis and identification of their main factors and variables as well as their effect on the development of the World Health Organization assessment instrument for mental health systems - (WHO-AIMS). Out of 11 components and 95 questions proposed, 6 factors that were effective on the development of the above instrument were identified using PLS software.
RESULTS
A study for mental health system condition in Khuzestan province and interviewing about instrument
Khuzestan province has a population about 4908989 people, that there is just one special psychological hospital with 210 beds in it. And there are the mental departments in generate hospitals just in 3 cities. Collecting the information of mental health system was not possible because the information was not registered. The mental disorders epidemic rate based on family medical team evaluation included mental disorders 11,2 per 1000 people, severe mental disorders 1,8 per every 1000 people, little mental disorders epidemic 3,5 per every 1000 people, mental deficiency discovers epidemic 3,4 per 100 people. The most mental disorders have been among married people with 60,1; also, most of the mental disorders were among housewives with 45 percent and by looking at the ages, the most age groups that had mental disorders were in ages 15-24 years old. By looking at the education, the most mental disorders were among uneducated people with 39,8 percent.
The findings showed that the noticeable numbers of researching community needed to mental health basic services. That with psychologists and psychological beds deficiencies in the state that they are in state center- it is needed to attempt to access a great information of mental health system and the world health organization has presented the WHO-AIMS instrument; therefore, the researcher has interviewed with a good expert for mental health system in Khuzestan about power and weak points of the instrument. The results are shown in (Table 1).
Table 1 The collected information from phases, that have done for extolling the initial questions for developing the WHO-AIMS instrument
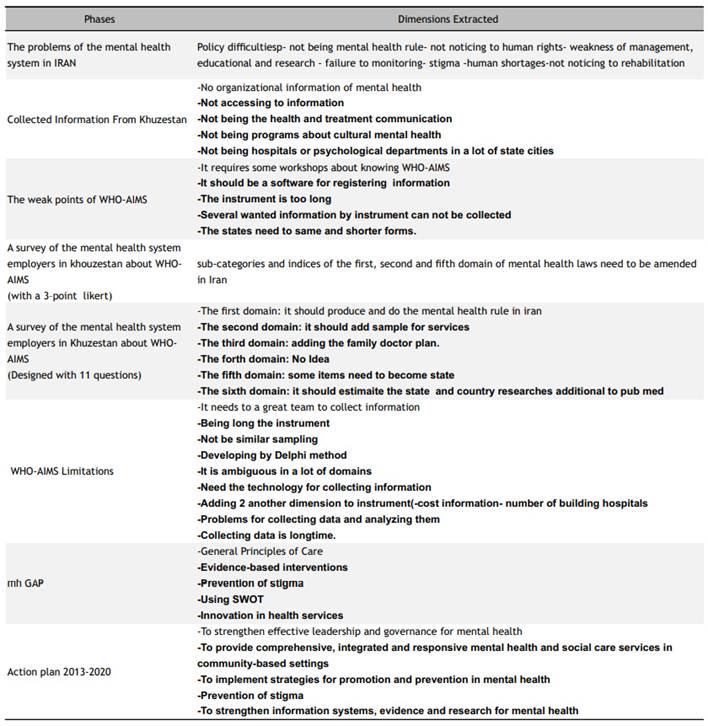
Study for Action plan in 2013-2020 of the world health organization and Mental Health Gap program (mh GAP) The Action plan of the world health organization 2013- 2020, helps to extol mental health with leadership support and mental health determination, basic and fundamental services, and effective mental health services in communities, health technologies for extolling and preventative plans for mental health, alimentating information system, evidence-based information system and research for mental health, access to high quality services, social mark forbidden((20 21, Ivbijaro (2012) explained some main principles of functional by noticing the mental health justice, access to mental health services, making better human rights, function based on witnesses making the mental health disorders patients powerful22. Eaton et al (2014) attempted to increase access to mental health services, preventing from malignant to human rights, and preventing the social mark for important strategic events about mental health23. Saxena et al(2014)24) and Semrau et al. (2015) also found out that the information for mental health services is very important and also using Who- aims for collecting mental health data, by notice to targets and Action plan principle are important for developing mental health system25. And, so far, the main care principles, inventory in health services, noticing to social mal mark, noticing to human rights, information system elimination based on withness, noticing to human, cultural, beliefs, sources and healthy behaviors and using this analysis. From the mental health gap program by WHO in 2008 and doing the mental health gap program is for the targets, like reaching some new solutions for giving same services and access to careens based on the evidence26.
Patel et al. mentioned that decreasing the mental health gap by participating careens by employing with the community, supporting server leadership, the switable working with community culture, notice to services in all areas, and is possible27. The main extolled points from the study, that there are not in the WHO-AIMS instrument, are shown in (Table 1).
After extoling the different characteristics, all cases were given to experts as some questions for each domain, and the CVI /CVR questions for were remained, that the researcher thinks they are needed for developing instrument and produce a state sample.
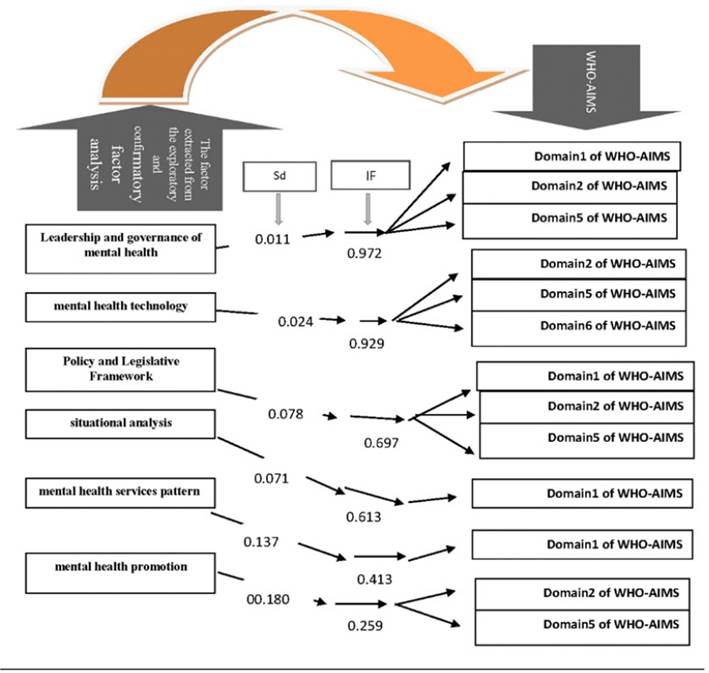
Finally, a total of 11 main components were identified and 95 questions designed for them; these question were then provided to mental health managers for exploratory and confirmatory factors analysis, identification of their main variables and their impact on the development of WHO-AIMS .Out of 11 components and 95 questions proposed, 6 factors that were effective on the development of the above instrument were identified using PLS software (Figure 1) and (Figure 2).
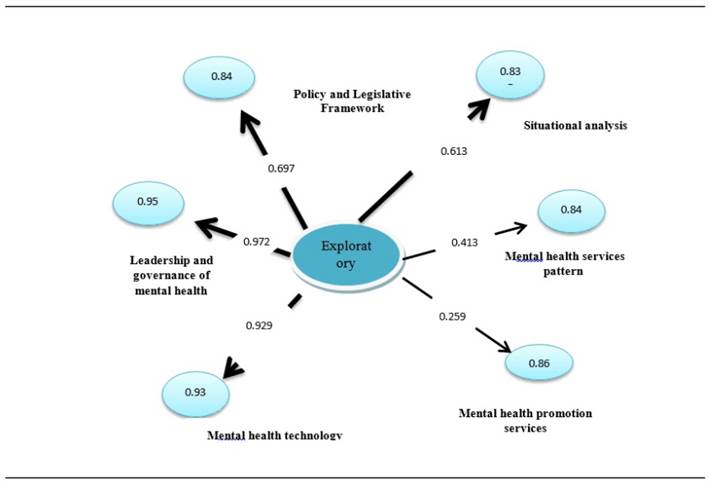
Figure 1 The effect of exploratory factors on the development of mental health system assessment tools based on the coefficient of influence and alpha of Cronbach
DISCUSSION
Leadership and governance of mental health with impact factor (0.972) and standard deviation (0.011) and significant level of p-value = 0.000 was considered as the first factor affecting the development of WHO- AIMS.
Leadership and governance of mental health are announced as a key goal of 2013-2020 operational plan, and leaders was assigned the duty of planning, organizing, and financing of health systems26.
In his study titled " Participatory Leadership in the Development and Success of the 10 Mental Health Organizations Network", Welkel (2014) showed that taking into account the creative leadership plays an important role in providing mental health services and assessing their effectiveness; leaders are involved in the quality of services28 29.
Patel et al. (2016) showed in their study titled the "China-India Mental Health Alliance: Mental Health System Accountability to the Treatment Gap in Adults in India and China" showed that leadership that is based on appropriate content and according to the culture of each community eliminates the mental health gap27.
Kabba referred in his study (2013) to nine managerial tasks that enhance the quality of services that include defining goals, emphasizing shared values of the organization, achieving the organization's vision, monitoring and evaluating the organization, motivating, achieving practical unity, explanation of the services, showing the path to the group, and change of the system30; therefore, one of the issues that needs to be taken into account in the management evaluation of the mental health system is paying attention to staffs so that they have no problems with their new information in the provision of mental health services.
Mansoori et al. (2011) also referred to unscientific management as the most important mental health challenge in Iran , Therefore, effective leadership has positive effects on organizational creativity and promotes organization31,32.
This factor is used in the development of the first, second, and fifth domains of WHO-AIMS. Confirmation of this case is also shown in Table 1. Investigations carried out in the first phase of the study showed that many countries have problems in the first domain (policy-making, legislation, and policies), the second domain (mental health services), as well as fifth domain (general education and communication with other sectors) and most of them have prioritized the proper management of human, financial resources, services and education in their programs35,38.
The mental health technology and the use of electronic services with impact factor (IF) (0.929) and standard deviation (SD) (0.024) and a significant level of p-value = 0.000 was announced as the second factor influencing the development of WHO-AIMS. Its subsets respectively include the use of teledentistry service with IF (0.727), the number of centers with new mental health technologies with IF of (0.716), the existence of a mental health information registration system with IF (0.543), and the number of articles on new technologies in mental health compared to all mental health articles with IF of (0.432).
In his 2016 study entitled Information Systems for Mental Health in Six Countries, Nawaraj found that countries face political, human resource, and management challenges, and proposed a Health Management Information System (HMIS)33, since the teledentistry is highly applicable to remote areas deprived of mental health services34. Its advantages have also been emphasized in Beher's research (2017) and the use of telemedicine in mental health Will reduce costs, save time, and reduce the length of stay39 40. On the other hand, in his study titled telepsychiatry in the 21st century: the transformation of health care into technology, Deslich (2013) showed that telemedicine should be used in psychiatric care and evaluated since this method has improved the quality of mental health services in the United States40. Therefore, considering what has been said in WHO's goals to promote mental health it is necessary to investigate countries in terms of having mental health technologies and the use of electronic services. On the other hand, many countries have approved the WHO- AIMS, and necessitate it to advance mental health goals. However, the large size of the instrument, and data collection problems, and lack of trust in data have led countries such as Lebanon, to express the need to integrated mental health information gathering system in their suggestions32. WHO-AIMS This factor is used in the development of the second, fifth, and sixth domains of WHO-AIMS. The confirmation of this case is presented in (Table 1). The researches carried out in the first phase of the research showed that many countries and especially Iran have problems in the second (mental health services), the fifth (general education and communication with other sectors), and the sixth domains (monitoring and researching); on the other hand, the problems reported in the mental health system of Khuzestan province in the second phase indicate that the system needs information technology to minimize its problems while providing services, education, and research.
Therefore, the reliability of this factor is confirmed with respect to Cronbach's alpha=0. 933; and on the other hand, this factor has exhibited high power in predicting its construct (Q2 = 0.358).
The mental health Policy and Legislative Framework was announced as the third factor influencing the development of WHO-AIMS with IF = 0.697, SD= 0.078, and significance level= 0.000. Considering that the mental health act has been included in WHO-AIMS and has been approved in various versions of the tool, but as researcher's comparative studies suggest that the WHO- AIMS is long and needs to be summarized, as well as the tool shortening was considered necessary by significant percentage of mental health system staffs during the provincial opinion polling on the one hand, and since there is no mental health Policy and Legislative Framework in Iran and the elimination of unnecessary cases was prioritized on the other hand; the mental health rules should be eliminated practically, but since this tool is universal, the researcher investigated the domain of the main tool under the guidance of his professors once again, and extracts domains that were related to mental health rules (first, second and fifth domains). The researcher then included them his final questions to assess their effect on the tool development by the professors and experts once again, and was finally opinion polled by in by managers at the national level; therefore, it was shown to be the third most influential factor in exploratory factor analysis (Figure 1).
The importance of this factor has been shown in most studies, including the WHO Atlas (2014), which specified more than 20% of 149 countries surveyed do not have mental health policies and rules, and at least one third of countries have no policy regarding the implementation of the rules. American, European, and Southeast Asian countries have a higher level of enforcement, but African and Eastern Mediterranean countries have lower levels of enforcement of mental health act s14. On the other hand, Since Yadollahi & Bolhari showed in their researches in Iran that more than 75% of psychiatrists face legal problems in their career and more than 70% of them considered the existing act s to be inadequate, thus, prioritizing the achievement of the mental health act, which led to development of draft of the Mental Health Act by the subsequent researches carried out by Nasr Esfahani and Attari Moghaddam in 2016, as it has been stated in this study that Iran has no independent mental health act, and it has been shown that countries have moved towards having such rules over time; for example, 15.9% of the countries had a mental health act in the 1950, and this figure reached 40.6% from 1991 to 200041. Therefore, the removal of this item from the tool is not in favor of the mental health system of Iran, because there are many challenges in mental health of the country. On the other hand, opinion polling of national experts and managers, the test statistics of the effect of the Mental Health Act on WHO mental health system in Iran is equal to 8.879 (sig = 0.000), which indicates that the Mental Health mental health with IF 0.697 of affects the WHO mental health system in Iran.
Therefore, with respect to Cronbach's alpha 0.840, the reliability of this factor is confirmed and on the other hand, this factor has shown moderate power in predicting its constructs (Q2 = 0.143).
The status quo analysis with IF (0.613). SD (0.011), and p-value = 0.00 was announced as the fourth factor influencing the development of WHO-AIMS. There was no status quo analysis in the WHO-AIMS main tool. Therefore, after carrying out comparative studies, interviews, and studies on the status of Iran, the researcher included this item in the expert's and then managers' opinion polling. Its subsets, including assessing the weaknesses of the mental health system, listing the existing problems and mental health gaps, assessing the strengths of mental health system, investigation of threats and opportunities in the mental health system with high IF were approved (Figure 2).
Saxena (2007) showed in his evaluation that investigation of the status of the mental health system would lead to the development of mental health services and an increase the reliability of information of the mental health system during assessments24.
Xavier et al. (2015) conducted a research titled "Updating Mental Health Programs in Portugal: using SWOT", by which mental health programs were examined in 2007-2016, and weaknesses, strengths, opportunities, and threats were evaluated. Authors considered the use of existing status analysis as necessary to promote mental health of the country42.
The status quo analysis has been prioritized in the mental health policy document of 2011-2015 for the preparation of a comprehensive mental health promotion program; because the analysis of the status of the mental health system of the country shows that the internal environment is currently weak and the external environment is threatened, and the he current situation promotion requires the internal capacity building of the mental health system and the development of inter-sectorial cooperation, including public participation43; therefore, it is necessary to determine the mental health status of each province to provide a complete picture of the mental health status of the country for future planning. Therefore, the reliability of this factor is confirmed with respect to Cronbach's alpha= 0.613, but this factor has shown moderate power in predicting its constructs (Q2 = 0.188). The researcher has attribute such moderate power to the fact that the status quo analysis has been carried out in all provinces. Moreover, according to the Mental Health Policy document, the status quo analysis has only been investigated in some provinces; however, since it has shown good inter-construct composite reliability (CR= 0.881), the researcher regards this factor as necessary for the development of mental health tools.
Presentation of mental health services model for prevalent disorders with IF=0.413, SD= 0.137, and p- value = 0.003, was considered as the fifth factor affecting the development of mental health system assessment tool, which had less impact on the development of tool and the item accounting for the highest weight includes the existence of a model for mental health services for each of prevalent disorder with IF=0.81 (Figure 2).
Referred to common disorders of the country (mood disorders, schizophrenia, etc.) and the provision of mental health services and structures as two of the priorities of mental health of the country, and this is indicative of the fact that Iran needs a model to have specific service delivery model for each type of disorder43. On the other hand, they announced in the 2013-2020 operational plan, the four main objectives for implementing the program including effective leadership, mental health governance, comprehensive provision of mental health services, and integrated care, prevention and promotion strategies. This project showed premature occur 40-60% higher in patient with mood disorders and schizophrenia and also stated the use of evidence-based protocols to provide mental health services. This project also strongly recommends for coverage of services (over 20%) for people with severe mental disorders by 202026.
According to the Mental Health Gap Intervention Guide (2010), mental disorders were prioritized based on mortality, disability, and high cost of treatment, and care designed for those disorders (based on evidence) and reviewed every 5 years. In this guide, reference has been made to cases such as the provision of evidence- based mental health services, setting of goals, promotion of quality improvement, family and community education, prevention programs, rehabilitation programs and mental health promotion programs, which evidence-based services reduce mental health gaps44.
This factor is used in the development of the first domain of WHO-AIMS. The confirmation of this case has also been shown in (Table 1), and given that the questions of this factor are used to monitor a service delivery model for common disorders, and the content of the first domain revolves around mental health frameworks, policies, and plans (1, 2); the researcher consider this factor essential for the development of WHO-AIMS. On the other hand, Cronbach Alpha= 0.845 is indicative of its good reliability, although it has shown moderate power in predicting its constructs (Q2 = 0.020). Mental health promotion services with IF=0.259, SD= 0.180, and p-value = 0.151 have been identified as the sixth factor affecting the development of WHO-AIMS, which, however, it has a very weak impact on the development of the above instrument according to the statistical coefficients. The researcher attributed such weak impact to the proximity of the second and the fifth factors to be the sixth factor. As is evident in the WHO-AIMS, all domains are closely interrelated, for example, the fourth domain assesses the human resources in the mental health system, and the third domain of the instrument also investigates the trained human resources24. And the researcher has mentioned the number of human resources that provide mental health promotion services in the development of their proposed instrument.
However, considering Cronbach's alpha= 0.863, the reliability of this factor is confirmed and has shown good inter-construct composite reliability (CR = 0.859). On the other hand, after opinion polling the experts, the content validity ratio (CVR) and the content validity index (CVI) of the constructs of this factor have been confirmed.
In his research titled "Is there a case for mental health promotion?", Fernandez (2014) writes: The promotion of mental health services requires a large-scale initiative (such as progressive policies, opposition to injustice, and promotion of social justice) and micro-scale initiative (e.g., individual education)45 46. Therefore, this is a very broad area. According to the WHO's operational plan and mental health gap, all the constructs of this factor were prioritized for investigation26) and the individual constructs expressed in this factor have been approved in comparative studies. For example, the number of service providers is evaluated in this factor, and was confirmed in Santos's research (2016). In this study, one of the barriers to the patient care is stated to be the insufficient number of trained service providers35.
Other cases that are evaluated in the mental health service promotion factor include destigmatization and mental health literacy promotion services, which have also been reported in Jang (2015) as the most important cases in measurement of mental health services36 37. In their research titled showing mental health status in the post-2015 development agenda, Eton et al. (2014) showed the need to promotion services such as destigmatization services, but there is still do no strategic plan23. Samero (2015) showed in a study that the inputs and outputs of the mental health system should be evaluated in order to coordinate mental health programs, and one of these inputs was stated to be mental health services, and the quality of their implementation and promotion services25.
Mental health is one of the important public and social health issues that affects the development and promotion of a community, and each country is working to achieve the full physical and mental well-being of individuals; therefore, mental health governance and service delivery innovation are it is mandatory so that we achieve progress in the mental health system; moreover, a clear picture of this system is prepared when all information are available and such information Cen be collected using WHO-AIMS.
After carrying out opinion polling at the provincial and national levels, and reviewing relevant studies in this area, the researcher developed the instrument and dimensions extracted in the domains of leadership and governance of mental health, technology and use of electronic services, current status analysis, mental health service delivery, and mental health promotion services were confirmed. due to the problems of the Iranian mental health system such as: lack of mental health act, lack of attention to human rights, shortage of human resources, shortage of financial resources, lack of culture building, social stigma of mental disease, monitoring problems, management weakness, and research problems significantly help to integrate mental health system information. The development of WHO-AIMS in Iran will help identify the gap in mental health system and determine the service model based on the problems identified, and the key indicator for developing this instrument is to understand the need for patient intervention and care. This understanding will be possible by strengthening leadership in the mental health system, participatory care through interaction with society, collecting relevant content based on community needs and culture, and paying attention to the coverage of services to reduce such gap.