INTRODUCTION
Obesity is a public health problem. Over the years, its prevalence and incidence have been progressively increasing worldwide 1-2. The global prevalence of obesity has increased at an alarming rate in children and adolescents from 0.7% to 5.6% in boys and from 0.9% to 7.8% in girls between 1975 and 20162.
The nutritional status classifications in children and adolescents can be classified according to body mass index2 (BMI) (Table 1). Although BMI provides a good measure of body fat in adults, children body fat varies according to age and gender. As such, fixed levels of BMI provide inaccurate comparisons3.
Table 1 Weight categories for youth (2-18 years) according to body mass index (BMI).
| NUTRITIONAL STATUS | BMI |
| Underweight | BMI <5th percentile for age |
| Normal weight | BMI ≥ 5th to < 85th percentile for age |
| Overweight | BMI ≥ 85th to <95th percentile for age |
| Obesity | BMI ≥ 95th |
| Severe obesity | BMI ≥ 120 % of the 95th percentile or a BMI ≥ 35 Kg/m2 |
Additionally, according to the WHO, in children under 5 years of age, overweight can be diagnosed when the weight/height ratio is greater than 2 standard deviation and obesity when the weight/height ratio is greater than 3 standard deviations.
In Peru, during the last decade, the prevalence of overweight and obesity in children under 5 years of age, after having reached their minimum values in 2016 (6.1% and 1.5% respectively), have been increasing progressively to 6.7% overweight and 2.1% obesity for the second quarter of 2021, according to the Sistema de Información Del Estado Nutricional (SIEN) of the Instituto Nacional de Salud (INS)1.
Obesity is associated with multiple comorbidities2, including cardiovascular, dermatologic, endocrine, gastrointestinal, neurologic, orthopedic, psychosocial, and pulmonary comorbidities (Table 2).
Table 2 Comorbidities of obesity in children and adolescents
| Cardiovascular | Hypertension, dyslipidemia, abnormal cardiac structure and function and adult cardiovascular disease |
| Dermatologic | Acanthosis nigricans, striae, intertrigo, furunculosis, hydradenitis suppurativa |
| Endocrine | Prediabetes, diabetes mellitus, metabolic syndrome, hyperandrogenism and polycystic ovary syndrome, growth and puberty |
| Gastrointestinal | Nonalcoholic fatty liver disease, cholelitiasis |
| Neurologic | Idiopathic intracranial hypertension |
| Orthopedic | Slipped capital femoral epiphysis, fractures, genu varus or valgus |
| Psychosocial | Social isolation, anxiety, depression, distorted peer relationships, disorder eating patterns |
| Pulmonary | Asthma, obstructive sleep apnea, obesity hypoventilation syndrome |
PATHOPHYSIOLOGY
Obesity in children has a complex etiology that originates from environmental factors (sedentary lifestyle, high-calorie diets) in modern societies2. Nonetheless, genetic factors may play an important role in its pathogenesis. However, the role of genes in obesity may be modest, and obesity predisposition may result from a combination of specific genes. More studies need to be conducted to fully understand the gene-environment interaction and epigenetics mechanism related to obesity4.
Obesity substantially increases the risk of metabolic and cardiovascular diseases such as type 2 diabetes mellitus, fatty liver disease, hypertension, myocardial infarction and stroke 2. The increase in adipose tissue influences the pathogenesis of atherosclerosis. Adipose tissue includes two types, namely, white adipose tissue (WAT) and brown adipose tissue.
WAT secretes peptides and proteins that play an important role in obesity, insulin resistance, immune functions, atherosclerosis, and CVD. Among them, adiponectin stands out, that is expressed at high levels in lean and healthy people and is deregulated in obesity5. Molecular studies have reported that adiponectin could modulate atherogenic mechanisms involved in endothelial cells (nitric oxide production, mitigation of pro-atherogenic mediators, stabilization of the coronary plaque, and arterial vasodilation). Likewise, it is known that perivascular adipose tissue, particularly in obese people, promotes local inflammation and deterioration of endothelial function, providing a link between adipose tissue and vascular disease6.
On the other hand, obesity is considered an inflammatory state, in which an increase in adipose tissue and a reduction in adiponectin levels occurs. Its unbalance perpetuates inflammation, leading to cardiometabolic alterations. Furthermore, obesity leads to insulin resistance and endothelial dysfunction due to the formation of pro-inflammatory cytokine and lipid metabolism products6. Endothelial dysfunction has been associated with cardiovascular conditions, such as atherosclerosis, hypertension (HT), hyperlipidemia, and insulin resistance5.
Obesity is associated with elevated levels of leptin and greater release of reactive oxygen species from the endoplasmic reticulum, generating less insulin secretion and sensitivity. Leptin influences the production of nitric oxide and activates the sympathetic system, causing sodium retention, systemic vasoconstriction, and blood pressure elevation7.
Obesity and covid-19
The COVID-19 pandemic led to different policies to contain the virus, such as lock-downs around the world, resulting in physical activity and changes in dietary behavior among children and adolescents. In addition, the reduction in social interaction causes isolation and a feeling of loneliness among children, leading to changes in emotional eating8.
As a result of this, children gained weight, and the prevalence of childhood obesity increased in different countries8. In the Unites States, the prevalence increased more than 15%9. In China, the BMI increased significantly in adolescents and young adults (15-17 years), while the prevalence of obesity increased from 10.5% to 12.9% (I < 0.001) in these age groups10. A new term, “covibesity,” was introduced to describe the worsening of obesity rates due to confinements11.
The three main risk factors that link obesity with COVID-19 demonstrated in adults that are also present in children and adolescents are chronic subclinical inflammation, impaired immune response, and underlying cardiorespiratory diseases12. Obesity is linked to a pro-inflammatory state induced by the production of cytokines such as interleukin-6 (IL-6) and C-reactive protein. These cytokines have been positively correlated with COVID-19 severity, and their higher levels in obese pediatric population may be related to increased susceptibility to severe infection13.
Obesity and cardiovascular risk
Both obesity and atherosclerosis are considered chronic inflammatory conditions, in which the activation of nonspecific and immune-adaptive processes plays a significant role14. The pathogenesis of obesity and atherosclerosis has several common factors. In both cases, the oxidized LDL particles and free fatty acids activate the inflammatory process and trigger the disease. Inflammation is responsible for all steps toward atherosclerosis, from the onset of endothelial dysfunction to atherosclerotic plaques, causing complications, and is related to obesity, insulin resistance, and type 2 diabetes (T2DM)15.
Fat tissue releases adipocytokines, which induce insulin resistance, endothelial dysfunction, hypercoagulability, and systemic inflammation, facilitating the atherosclerotic process. In visceral obesity, inflammatory adipocytokines (e.g., TNF-α, IL-6, MCP-1, leptin, and resistin) rise to higher levels. Furthermore, increased C-reactive protein level is associated with an increased risk of myocardial infarction, peripheral vascular disease, and diabetes mellitus16.
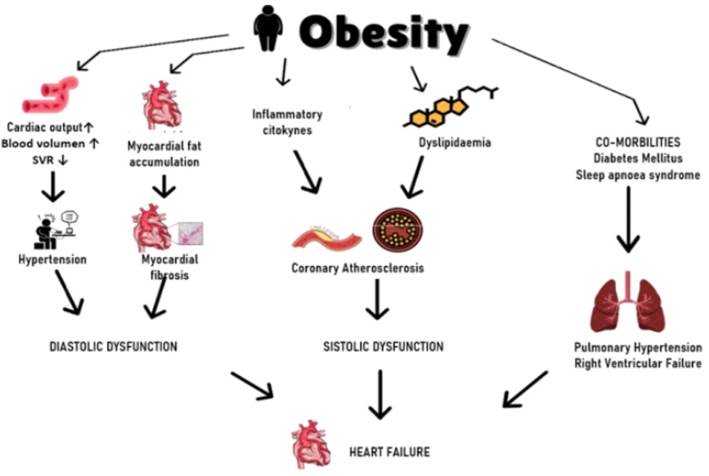
Likewise, obesity leads to heart failure through several indirect mechanisms. Excess weight leads to hemodynamic changes: an increase in cardiac output and blood pressure has been observed, and an increase in BMI of 5 kg/m2 generates a 5 mmHg increase in systolic blood pressure. On the one hand, it is related to the activation of the renin-angiotensin-aldosterone system and the increased activity of the sympathetic nervous system7.
Obesity increases the aldosterone level and expression of the mineralocorticoid receptor, promoting interstitial fibrosis, platelet aggregation, and endothelial dysfunction in the heart. Increased blood volume facilitates venous return flow, which improves preload, causing increased ventricular wall tension and ultimately leading to ventricular dilation. The inflammatory cytokines (TNF-α, IL-1, IL-6, IL-8), which are increased in obese people, also play an important role in heart failure development. The effect of leptin and adiponectin on the metabolism and extracellular matrix can contribute directly to the myocardial transformation. The accumulation of triglycerides in the heart muscle can be observed regularly in obese patients and facilitates the generation of toxic metabolites (ceramide and diacylglycerol), causing apoptosis of cardiomyocytes16.
Besides, obesity has been shown to increase the probability of heart failure, not only by itself but also through associated medical comorbidities (Figure 1).
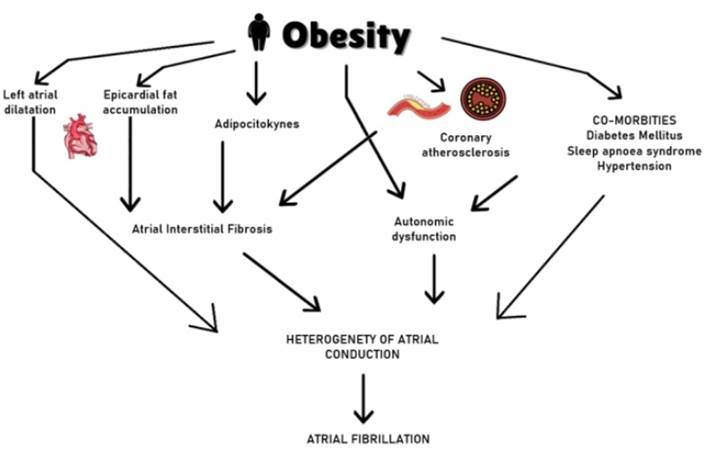
Several studies have shown the relationship between obesity and atrial fibrillation (Figure 2). Obese patients have a 1.52 times higher risk of developing atrial fibrillation compared to the normal weight population. Likewise, an increased risk of sudden cardiac death, stroke, thromboembolic complications, and heart failure exists in patients with atrial fibrillation. Moreover, atrial fibrillation lengthens the hospitalization time and worsens quality of life and physical capacity17.
Morbid obesity (defined as BMI > 35 kg/m2) potentially causes a wide range of alterations in heart performance, including changes in cardiac hemodynamics, left ventricular function, and morphology18 (Table 3).
Table 3 Impact of obesity on hemodynamics and heart morphology.
| HEMODYNAMICS | ↑ blood volume, stroke volume/work ↑ arterial pressure, LV wall stress Pulmonary artery hypertension |
| CARDIAC STRUCTURE | • LV concentric remodeling, hypertrophy Left atrial enlargement RV hypertrophy |
| CARDIAC FUNCTION | LV diastolic or systolic dysfunction RV failure |
RV: Right ventricle, LV: Left ventricle.
Screening for cardiometabolic risk factors (HT, dyslipidemia, T2DM) should be undertaken in all children with obesity. Specific coronary risk scores, such as the Framingham risk score, are well established for clinical risk stratification in adults; however, no similar risk stratification tools are available in children19.
A risk score developed from the PDAY (Prediction of coronary artery calcium in young adults using the pathobiological Determinants of Atherosclerosis in Youth) study has been used in pediatric, using the autopsy findings in subjects 15-34 years of age and coronary heart disease risk factors (gender, age, serum lipoprotein concentrations, smoking, HT, obesity, and hyperglycemia) to estimate the probability of advanced atherosclerotic lesions in the coronary arteries. However, more studies are needed to assess the utility of this risk score20.
Sleep disorders and obesity
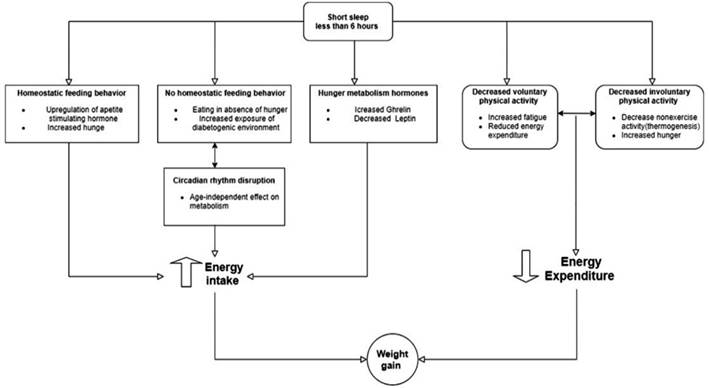
Sleep restriction seems to be related to our modern way of life. People who sleep little can have difficulties in maintaining a healthy lifestyle in the current environment since it promotes excessive consumption of food and sedentary behaviors. Moreover, there is strong evidence to support that sleep reduction is a contributor to obesity in all age groups of the pediatric population(21). Increased food intake seems to be the main explanation for why a lack of sleep can lead to weight gain(22).
Chaput JP et al. hypothesized an interesting theory to explain the relationship between short sleep duration and obesity. For weight gain to occur, there must be an imbalance between energy intake and expenditure. The energy intake is determined by eating food, and the energy expenditure is determined by physical activity. Both factors would be altered by a decrease in sleep, the consequence of which would be weight gain22. (Figure 3). However, this author does not define exactly the number of hours that would be the threshold to define short sleep, which would have this effect (weight gain). Subsequent studies clearly show that sleeping for less than 6 h is considered a cutoff point for this particular effect and other harmful effects on health23.
Obstructive sleep apnea (OSA) is an obesity-related complication that has recently gained attention. It is defined as a breathing disorder during sleep in which partial or complete airway obstruction disrupts ventilation. The prevalence of OSA varies between 1% and 5% in general pediatric population; however, among obese children and adolescent, the prevalence of OSA is estimated to range between 20% and 61%. OSA in obese children is associated with cardiovascular complications such as right and left ventricular dysfunction, besides increased systolic blood pressure24. All this information suggests that OSA may have a negative impact on long-term cardiovascular health.
Nafld and obesity
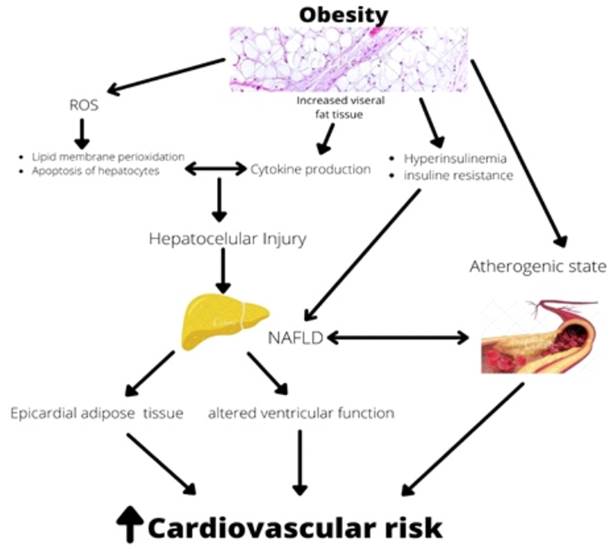
Nonalcoholic fatty liver disease (NAFLD) is directly linked to obesity and has become a major cause of chronic liver disease among children and adolescent with obesity. Two hypotheses have been put forward to explain the pathophysiology of NAFLD. First, obesity-related hyperinsulinemia and insulin resistance lead to liver steatosis25. Second, the oxidative stress by reactive oxygen species (ROS) may cause hepatocellular damage inhibiting mitochondrial respiratory chain enzymes. Furthermore, ROS may cause lipid membrane peroxidation, apoptosis of hepatocytes induced by Fas ligand, and cytokine production, perpetuating hepatocellular injury and fibrosis26.
NAFLD has been recognized as an independent risk factor for CVD; however, the association is still debated in pediatric population. This association has not been fully understood yet, but increased visceral fat tissue and insulin resistance may be important contributing factors27. NAFLD is part of the metabolic syndrome, which is an atherogenic state. Atherosclerosis has been shown to begin in pediatric age28. To the best of our knowledge, the mechanism by which NAFLD may lead to atherogenesis is not elucidated, but increased visceral adipose tissue expressed by particularly periaortic fat thickness, altered lipoprotein metabolism, insulin resistance, and inflammatory cytokines released by NAFLD may play a significant role. (Figure 4)
Treatment of obesity in children and adolescents
The three main treatment approaches for pediatric obesity are diet and lifestyle modification, pharmacological interventions, and surgical management.
A. Behavioral interventions for weight loss
Successful weight loss can be improved by incorporating behavioral strategies29.
Examples of well-proven behavioral weight loss programs designed to reduce body weight include the Diabetes Prevention Project, the Look AHEAD Study for Adults, and family-based behavioral weight loss programs (FBT) for children29. Systematic reviews in this area show that adults who participate in behavioral weight loss (BWL) programs of 12-26 sessions lose approximately 6% of their body weight30, while children who participate in at least 26 BWL sessions lose 0.2 ZBMI31, both clinically significant weight losses associated with multiple improvements in health.
The trials used different intervention methods, such as group, individual, and mixed. Group interventions consisted of classroom-style sessions that lasted from 1 to 2 h and ranged from eight group sessions over 2.5 months to weekly group sessions over 1 year. Most individual-based interventions provided individual counseling sessions, with or without ongoing telephone support, with a median number of sessions in the first year of 1232. Mixed-based interventions included the same number of group and individual counseling sessions. Most of these interventions were carried out for more than 1 year and involved more than 12 sessions (median, 23 sessions in total in the first year). In the technology-based interventions, web-based intervention modules, web-based self-monitoring, mobile phone-based text messages, smartphone apps, social media platforms, or DVD learning were included. In addition, in most of these behavioral interventions, self-control was promoted by recording daily dietary intake33. Using websites that provided real-time feedback on the total calories consumed for the day based on the foods and portion sizes recorded, the remaining calories can help achieve the participant’s personal daily goal34.
Most of these behavioral interventions were designed to help participants achieve or maintain a weight loss of 5%-10% or more through a combination of dietary changes and increased physical activity29.
B. Pharmacological intervention
The 2017 Endocrine Society Clinical Practice Guidelines recommend pharmacotherapy for children or adolescents after a formal program of intensive lifestyle modification has failed35.
Orlistat is the only FDA (US Food and Drug Administration)-approved weight loss medication for use in children ≥ 12 years who are overweight/obese. This lipase inhibitor is associated with 1-2 kg weight loss in adolescents. It has been associated with modest improvement in diastolic blood pressure and a marker of endothelial function (flow-mediated dilation), but its cumulative effect on reducing cardiometabolic disease remains unknown35.
Metformin is the most common agent evaluated for the treatment of obesity in children. Randomized trials of metformin have demonstrated modest weight loss (2-4 kg) in youth with marked improvement in markers of insulin resistance. However, similar to studies conducted for orlistat, most metformin trials are ≤ 1 year in duration, and the durable effect of these pharmacological agents on weight loss or cardiometabolic risk reduction requires further investigation36.
C. Surgical management
Bariatric surgery is a treatment option for obese adolescents. Three procedures are primarily used for adolescent bariatric surgery, namely, laparoscopic sleeve gastrectomy (LSG), laparoscopic adjustable gastric banding (LAGB), and Roux-en-Y gastric bypass (RYGB). Weight loss occurs due to a restrictive and malabsorptive component37.
The International Pediatric Endosurgery Group recommends surgery in adolescents who have attained or almost attained adult stature with specific guidance37. (Table 4)
Table 4 Criteria for bariatric surgery in adolescents.
| REQUIREMENTS | • Severe obesity (BMI ≥ 40) with serious obesity related comorbidities. • Have attained or depending on the severity of comorbidity, nearly attained adult stature. • Have failed at least 6 months of organized conventional attempts at weight management. • Demonstrated commitment to comprehensive pediatric psychological evaluation both before and after surgery and agree to avoid pregnancy for at least 1 year post-operatively. • Be capable of and willing to adhere to nutritional guidelines post-operatively. • Have decisional capacity and provide informed assent for surgical management. |
| SERIOUS COMORBID CONDITIONS | Type 2 diabetes mellitus Moderate to severe obstructive sleep apnea Pseudotumor cerebri Severe and progressive steatohepatitis |
| LESS SERIOUS COMORBIDITIES | • Weigh related arthropathy • Hypertension • Dyslipidemia • Venous stasis disease • Urinary incontinence • Non-alcoholic fatty liver disease • Gastroesophageal reflux • Severe psychosocial distress and significant impairment in activity of daily living |
Due to the complex nature intervention, particularly at the vulnerable age of these patients, the use of multidisciplinary team has become well established as the gold standard of care necessary to provide a safe and efficient service.
The team members recommended by the American Society of Metabolic and Obesity Surgeon (ASMBS) includes an experienced bariatric surgeon; a pediatrician with a speciality in endocrinology and nutrition; a dietician with experience in pediatric obesity; and a psychiastrist or psychologist with specialty training in treating eating disorders and obesity in adolescents38:
Regarding the outcomes of the surgical management of obesity in this population, there are several studies carried out. In the Swedish Adolescent Morbid Obesity Surgery study, a prospective nationwide study, they performed laparoscopic RYGB in adolescents aged 13-18 years old. A significant lower BMI was observed postoperatively compared with age-matched medically managed controls. Moreover, cardiovascular risk factors substantially improved after surgery, including glucose tolerance, blood pressure, and plasma lipid concentration. All patients experienced T2DM remission39. The Follow-up of Adolescent Bariatric Surgery at 5 Plus Years (FABS 5+) investigated the outcomes of adolescent bariatric surgery 5-12 years after RYGB. In that study, mean baseline BMI was reduced postoperatively by 29%. Furthermore, there were remission of T2DM and resolution rate of hypertension40.
CONCLUSIONS
Obesity by itself, and its associated comorbidities, generates structural and functional alterations, increasing cardiovascular risk.
The pathophysiological processes that link obesity with atherosclerosis and CVD imply a chronic inflammatory state.
People with obesity without metabolic abnormalities have a higher risk of coronary artery disease and heart failure than metabolically healthy people of normal weight.
Severe obesity in children and adolescents is associated with a higher incidence of HT, dyslipidemia, and impaired fasting glucose.
Timely diagnosis and treatment of obesity is important to decrease the mortality among pediatric population.