INTRODUCTION
Patients with the severe form of COVID-19 develop viral pneumonia with severe hypoxemia that progresses to acute respiratory distress syndrome (ARDS). These patients require management in Intensive Care Units (ICU) where they are exposed to immobilization, immunosuppression, malnutrition or infections, thus increasing mortality and stay in the ICU 1. Rehabilitation is one of the approaches formulated in the face of this situation and the strategies applied have been reinforced or rejected according to the results based on the evidence and the greater understanding of this pandemic 2,3,4,5,6.
One of the most important neuromusculoskeletal alterations in patients with critical illness is Intensive Care Unit - Acquired Weakness (ICUAW), which can have a prevalence of up to 70% 7. Its main clinical manifestation is generalized symmetric weakness, which affects the extremities and can cause tetraplegia 8 and being involved in around 60% of failures in weaning from Mechanical Ventilation (MV), thus increasing the stay in the ICU and the days of MV, generating a vicious circle 9 with an impact on the length of stay in hospital (LOS), delirium, persistence of post-ICU syndrome and mortality 10. In a report of patients with COVID-19 who required MV in the ICU, in a city in Belgium 72% presented ICUAW on waking up and 52%, upon discharge from the ICU. In addition, patients with weakness stayed longer in days. ICU 11.
There is scientific evidence in favor of reducing the stay in ICU, use of invasive mechanical ventilation (IMV), increase in ventilator-free days (VFDs) at 28 days (VFDs-28) and functionality at discharge, among others, as a result of different modalities of rehabilitation installed during the critical phase of the disease 12,13,14. The application of multimodal rehabilitation programs; that is, those that include various interventions such as mobilization, muscular, respiratory and functional training 15, can avoid the impact of ICUAW.
Rehabilitation in critically ill patients with COVID-19 continues to be studied and is based on the different therapy modalities previously studied such as mobilizations, respiratory physiotherapy, patient mobility, bed cycling, electrotherapy, or speech and swallowing therapy 16,17,18,19 which have achieved partial consensus regarding its application 20,21. The results of a clinical trial in the United Kingdom based on different rehabilitation modalities, for patients in the ICU due to COVID-19, reported that, at ICU discharge, half of the patients managed to climb into a chair or walk despite the high prevalence by ICUAW 22
It is necessary to establish rehabilitation models that improve the efficiency of healthcare resources, availability of ICU beds and mechanical ventilators, reducing the impact of critical illness that causes moderate or severe disability, with the consequent individual and social cost and overload in the healthcare system 23. The objective of this research was to determine the effects of a Multimodal Rehabilitation Program (MRP) in patients with COVID-19 admitted to the ICU and to present a working model based on indicators.
MATERIAL AND METHODS
Protocol
The study was based on the protocol formulated by the members of the research team (protocol available at Figshare.com).
Participants
Patients hospitalized in the ICU of the Hospital de Alta Complejidad "Virgen de la Puerta" - EsSalud (Trujillo, La Libertad, Peru) from August 1 to November 7, 2020. The inclusion criteria were: age over 18 years, use of Invasive mechanical ventilation no longer than 72 hours prior to admission to the ICU. Where excluded, those with some degree of functional dependence, a diagnosis of neuromuscular diseases, tracheostomy carriers or those who had required this procedure during their stay, admission to the ICU with a main diagnosis other than ARDS due to COVID-19 or those who were admitted and died before the enrollment.
Allocation
The coding of the patients was based on the order of admission to the ICU, those with an odd admission number received Usual Care and those with an even number were part of the MRP. The allocation was sequential in a 1: 1 ratio to the MRP or the Usual Care group, with the sample frame being the records of admission to the Intensive Care Service. The total number of participants was 32 for each group.
Procedures
The MRP assigned to the intervention group was carried out six days a week and was in charge of Technologists in Physical and Respiratory Therapy. They were previously instructed in the modalities to be carried out as well as their registration.
Intervention
- Abbreviate name
Multimodal Rehabilitation Program (MRP)
- ¿Why?
MRP was proposed to provide different interventions in ICU patients in order to achieve a shorter stay in the ICU and use of MV. It was based on four modalities 16,17,24,25, which were a) mobilizations of four limbs, b) bed cycling, c) functional training, d) respiratory muscle training.
- ¿What?
Materials: Was necessary to use material for cycling in bed, elastic bands or therapeutic balloon. For the compilation of the intervention, files were used, which were available in the research protocol. Those responsible for the intervention were trained through audiovisual material and simulated training of data collection sheets, application of criteria for starting and stopping the intervention.
Procedures: Before the start of the interventions, the mechanical ventilation system, filters, safety of the inflatable balloon of the endotracheal tube, invasive access routes and airway permeability were verified daily. The usual care, assigned to the control group, consisted of postural changes including the beginning and end of pronation, permeability of the artificial airway by the service personnel or some routine physiotherapeutic intervention, mainly based on mobilizations.
For the application of the PRM, safety criteria based on a checklist were taken into account to decide to start or continue work with patients 17,26. These were: medical opinion of the patient's stability, heart rate between 40 and 130 beats / min, systolic blood pressure between 90 and 180 mmHg or mean arterial pressure between 60 and 110mmHg, respiratory rate between 5 and 40 breaths / min, oxygen saturation greater than or equal to 88%, inspired fraction of oxygen less than 60%, positive pressure at the end of expiration (PEEP) less than or equal to 10 cmH2O, use of norepinephrine greater than or equal to 0.1 mcg / kg / min, secured airway , changes in the level of consciousness during activity, appearance of new arrhythmia or that produces symptoms, angina pain, evidence of coronary ischemia, asynchrony with the ventilator, intolerance or rejection by the patient, evidence or suspicion of active bleeding, venous thrombosis deep or pulmonary embolism.
After the verification of security criteria, the different modalities were applied according to the description below 16,17,24,25
a. Mobilization of the extremities in functional ranges in a series of ten repetitions. When patients presented an adequate level of consciousness, active or active assisted mobilizations were carried out; otherwise, the movement was carried out only by the physiotherapist, that is, passive mobilization.
b. Bed cyclingfor up to ten minutes. This activity was also carried out actively, actively assisted or passively according to the level of consciousness and collaboration of the patient, in the case of patients with adequate collaboration.
c. Functional training, that is, displacements either in your own bed (achieving a sitting position within it or on the edge) by standing or transferring to a chair.
d. Respiratory muscle training, only in patients who were able to obeying instructionsfor the techniques used.
During the first days of stay, the activities were based on mobilization and cycling in bed, later and according to the level of collaboration of the patient, the other modalities of the program were used.
The prone position was a contraindication for bed cycling, functional training and respiratory muscle training, due to the need to comply with the medical prescription of the intensive medicine team. However, the mobilization of the limbs was continued.
When patients were able to obey complex orders or had an indication for ICU discharge (according to the decision of the medical staff of the service), an assessment of muscle strength was performed according to the Medical Research Council scale 27 to establish the diagnosis of ICUAW.
- ¿Who?
The MRP was carried out by personnel from Medical Technology in Physical and Respiratory Therapy, previously guided and trained by the research team and a specialist in Physical Medicine and Rehabilitation for the application of the MRP.
- ¿What?
The intervention was carried out in person at the bedside of each patient.
- ¿Where?
Carried out in the Intensive Care Unit of the Hospital de Alta Complejidad Virgen de la Puerta, Trujillo, La Libertad
- When and how many
During the period August - November 2020. 657 MRP modalities were carried out
- Adaptations
The intervention was applied following the proposed protocol. The work modalities could vary in duration according to either the tolerance of the patient or the adverse events triggered.
- How well
Compliance with the intervention was planned, making use of data collection sheets.
Outcomes
The variables evaluated in this study were: days of ICU stay, days of invasive mechanical ventilation, ventilator-free days at 28 days (VFDs-28), length of stay in hospital (LOS), muscle strength through the MRC (Medical Research Council) score, mortality, frequency of ICUAW, indicators of IRM and adverse events.
The use of indicators within the MRP was proposed. These were:
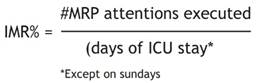
Intensity of Multimodal Rehabilitation according to the "percentage of execution" (IMR%):The calculation of this variable was carried out by obtaining the percentage of days attended at the MRP with respect to those scheduled for each patient. The number of scheduled care was equal to the number of days of ICU stay, except on Sundays. This indicator was used to estimate the coverage of care.
Intensity of Multimodal Rehabilitation according to the “number of modalities executed per scheduled day” (IMRm-scheduled):It was obtained by dividing the total number of modalities executed (mobilization, bed cycling, respiratory muscle training or functional training) between the days programmed for each patient. In other words, the number of days of ICU stay, except on Sundays. This indicator was used to estimate the average of the modalities received according to the scheduled days; that is, during the ICU stay.
Multimodal Rehabilitation Index (iMR): Value obtained by multiplying the "Percentage of execution" by the "number of modalities executed per scheduled day" that allowed to measure and compare the concentration of the modalities in each patient.
Sample size
The entire universe that met the selection criteria during the specified period was included.
Statistical methods
Measures of central tendency and dispersion were used for quantitative variables and frequencies for categorical variables. Due to the quantitative nature of the variables, days of stay in the ICU, days of mechanical ventilation in the ICU, ventilator-free days at 28 days (VFDs-28), length of stay, and muscle strength, the Mann Whitney U test and T test were used. For categorical variables such as outcome and presence of ICUAW, Pearson's X² test or Fisher's Exact Test were used to make comparisons between groups. Mean Difference (MD) was reported for values that complied with the normal distribution and Relative Risk (RR) for dichotomous variables.
The probable cut-off points for the proposed indicators were subjected to the X2 test, dichotomizing the outcome variables: days of ICU stay, days of MV, VFDs-28, LOS, muscle strength according to their trend measures central according to its normality distribution. In the case of categorical variables, only their distribution by groups was considered. This analysis was based on the work of Fuentes 28
The level of significance was established with p <0.05. The information was processed in spreadsheets and the SPSS® program
Ethical considerations
The research protocol was approved by the Specific Ethics Committee for Covid-19 ofComité de ÉticaEspecífico para Covid-19 del Instituto de Evaluación de Tecnologíasen Salud e Investigación (IETSI) - EsSalud and informed consent was obtained from the participants or authorized representatives.
RESULTS
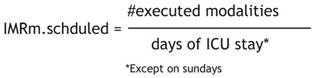
From August 1 to November 7, 106 possible participants were registered, which were interchangeably assigned to the control and intervention group. However, within each group, as 29 participants did not meet the selection criteria, they were withdrawn, leaving a total of 77 participants who began follow-up, with 11 and 2 patients withdrawing from the control and intervention group respectively. Figure 1 describes the recruitment process.
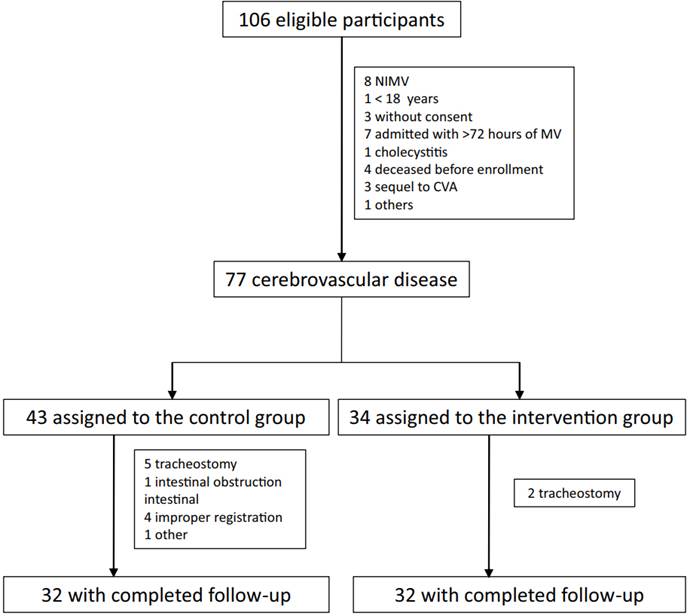
The clinical characteristics of the sample, (Table 1), included its comorbidities or risk conditions such as diabetes, obesity, cardiovascular disease - including hypertension-, age over 60 years and others. The age of the participants ranged from 29 to 79 years with an average of 52.5 ± 14.2 vs. 56.5 ± 11.2 in the control and intervention group respectively. Other data such as the number of associated comorbidities are presented in the same table. A total of 12 participants (18.8%) did not present comorbidities. Both groups presented infections during the ICU stay.
Table 1 Clinical characteristics of the participants
*Including Arterial Hypertension, HAIs healthcare-associated infections
After comparing the variables of main interest in the control and intervention groups, no statistically significant differences were found in terms of days of ICU stay (control = 13.2 days vs intervention = 18.8 days, p = 0.541), days of MVI in ICU (control = 12.1 days vs intervention = 14.7 days, p = 0.555),VFDs-28(control: 5.0 days vs intervention 8.1 days, p = 0.911), LOS (control: 25.6 days vs intervention: 27.4 days, p = 0.543), MRC (Medical Research Council) score (control 47.1 points vs intervention 47.2 points, p = 0.954). Regarding the qualitative variables, mortality (deceased vs survivors, p = 1,000) and ICUAW (YES vs NO, p = 0.437) did not show statistically significant differences either (Table 2).
Furthermore, due to the nature of the intervention, the same variables were analyzed in the surviving participants. No significant differences were found when evaluating the days of stay in the ICU (control = 11.17 days vs. intervention = 13.88 days, p = 0.579), days of MVI in the ICU (control = 9.53 days vs. 9.55 days, p = 0.588), VFDs-28(control: 18.48 days vs intervention 18.46 days, p = 0.588), LOS (control: 25.85 days vs intervention: 28.35 days, p = 0.545), MRC score (control 47.10 points vs 47.8 intervention points, p = 0.925), presence of ICUAW (p = 0.342)
Table 2: Comparison of outcomes by groups in all participants and survivors
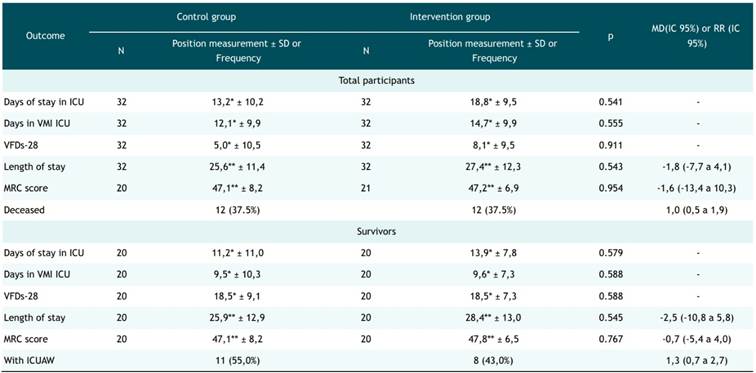
SD, standard deviation; VMI, Invasive Mechanical Ventilation; MRC, Medical Research Council, ICUAW, Acquired Weakness in ICU, VFDs-28, MV-free days in ICU at day 28; MD, mean difference; RR, Relative Risk
*Median
**Mean
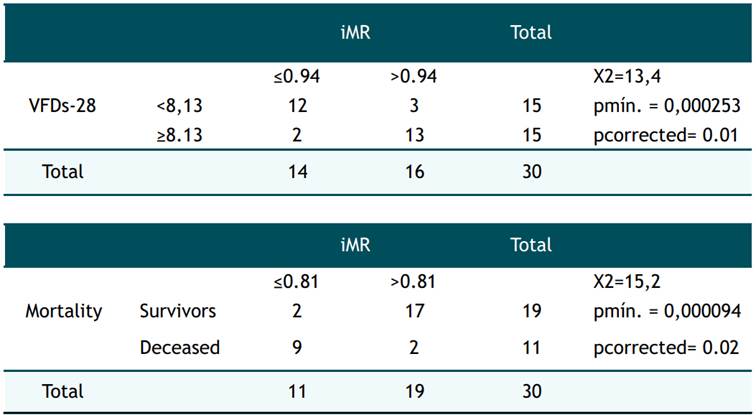
Regarding the other exploratory outcomes, that is, the MRP indicators. The IMR% was variable from 33.3% to 100% (n = 5 for IMR% between 33.3% to 50%, n = 10 for IMR% between 50% and 75%, n = 9 between 75% and 95% and n = 8 with IMR% equal to 100%) the IMRm.schduled was ranged from 0.3 to 2.7 (SD = 0.6, mean = 1.5), and the iMR from 0.1 to 2.7 (SD = 0.7, mean = 1.2). The cut-off points established for the indicators were found after selecting the values between the 5% and 95% percentiles applying the correction pcorrected = −3.13 pmin (1 + 1.65 ln (pmin)) where pmin = p-value smaller between the probable cutoff points. The iMR was significant for the cut-off points ≤ 0.94 (p = 0.01) and ≤ 0.81 (p = 0.02) in terms of VFDs-28 and mortality respectively (Table 3). The other indicators did not have significant cut-off points applying the methodology proposed by Fuentes. 28.
Table 3 Frequency distribution and comparison between the Multimodal Rehabilitation Index (iMR) with the VFDs-28 and mortality
Of a total of 657 modalities executed in the group that participated in the MRP, 7.6% (n = 50) adverse events considered as mild were reported, because they remitted spontaneously, without medical intervention. These were: intolerance to exercise in 40% (n = 20), alteration of blood pressure in 40% (n = 20), desaturation in 10% (n = 5), alteration of heart rate in 6% (n = 3), altered respiratory rate in 10% (n = 5) and others in 2% (n = 1) (Table 4). The modalities executed were based mainly on mobilization in 54% (n = 354), followed by 29% (n = 191) of bed cycling, 16% (n = 102) of respiratory muscle training and finally 1.5% (n = 10) in functional training.
Table 4: Frequencies of adverse events reported in the Multimodal Rehabilitation Program
| Adverse events | Absolute frequency | Relative frequency (%) |
| Effort intolerance | 20 | 40 |
| Altered BP | 20 | 40 |
| Desaturation | 5 | 10 |
| HR alteration | 3 | 6 |
| RR alteration | 1 | 2 |
| Others | 1 | 2 |
| Total | 50 | 100 |
HR, Heart Rate; RR, Respiratory rate
DISCUSSION
The general characteristics of the sample included a variety of comorbidities which have been related to increased mortality from severe COVID-19. Only 18.8% of the sample did not present any comorbidity. In addition, 54.7% (n = 35) presented infections demonstrated with cultures during their stay in the ICU, a value higher than those reported in other studies that range between 19% and 49% 29,30,31. Age also showed variability, and for this reason, there were various conditions that could directly influence mortality.
Despite the fact that in some reports 12,13,14 they find a benefit in favor of rehabilitation in terms of reduction of MV, stay or VFDs-28; In the present work, no significant differences were found between the control and intervention groups. The methodology used in the present work could have influenced the result because elements of the clinical trials, such as randomization and blinding, were not considered; in addition to the broad clinical spectrum of severity in COVID-19. On the other hand, the intervention did not maintain the same dosage in the PRM group. To date, there is no conclusive information on whether rehabilitation modalities in critically ill patients can reduce the duration of these variables 12,32, mainly due to the lack of consensus regarding the modalities used, duration and frequency 33.
ICUAW had no significant association with the intervention. The surviving patients showed a similar frequency in terms of the prevalence of ICUAW (control 55% vs intervention 40% p = 0.34) as well as similar averages of MRC score (control 47.1 vs intervention 47.8 p = 0.767). These results are similar to those reported in a systematic review with meta-analysis where the intervention did not appear to be related to changes in the incidence of ICUAW or the sum of the MRC score 34. It should be taken into account that the IMR% and the iMR varied between 41% to 100% and 0.41 to 2.71 respectively, among the survivors, due to the safety criteria applied in the patients that limited the interventions, as well as the condition of sedation that prevents functional training and breathing exercises. Due to the safety of the intervention, already established previously 26, the safety criteria could be broadened, assessing risk-benefit 26,32, allowing a higher percentage of execution and received therapies.
The quantification of the intervention provided in the MRP, through indicators, obtained a significant relationship when comparing the cut-off point of the iMR with the outcome and the VFDs-28 that are considered as outcome measures in ICU services 35. Even the use of VFDs-28 has been recommended in small sample sizes if it is proposed that the treatment to be investigated simultaneously reduces the duration of ventilation and improves survival outcomes 36. Although mobilization has not been shown to reduce mortality, respiratory therapy activities may have some impact on mortality 37,38. Taking into account that the patients with the lowest iMR were those who presented greater contraindications that limited the intervention; It could be argued that the observed increase in mortality, as well as the few VFDs-28, were possibly due to greater conditions of clinical instability during their stay in the ICU than a direct effect due to the absence of intervention. It cannot be ruled out that those who had higher IRM; that is, those who received a greater concentration of the intervention, could also obtain the established benefits of rehabilitation.
Some of the interventions and care involved in the broad spectrum of respiratory rehabilitation, such as patient positioning 39 could reduce the suspicion of ventilator-associated pneumonia. However, most of the studies are based on multimodal interventions according to the clinical condition of the patients, a situation that can diversify the intervention and limit adequate conclusions of its effect 37,38, although it was not possible to find studies that mention the efficacy of interventions in populations with superinfections.
The safety of these interventions has also been evaluated taking into account the number of adverse effects, including death, with respect to the total number of sessions performed. In this program, the safety and use of early rehabilitation programs for patients admitted to the ICU is established. This aspect was important because commonly a patient admitted to the ICU is considered unstable (high PEEP, pronation, use of vasopressors, high-dose sedoanalgesia, muscle relaxation, among others) and therefore does not receive rehabilitation in the first hours of admission. However, no adverse effects with fatal outcome were reported in this study. Around 15 adverse events that may require interventions have been reported for every 12,200 sessions 32. Regarding the specific use of bed cycling, 5 adverse events have been reported from 3,117 sessions, that is, 0.16% 40. During the development of this study, 8.37% adverse events were reported, all mild, remitting spontaneously without pharmacological intervention or changes in ventilatory parameters, which demonstrates the safety of MRP in critically ill patients. No events that required active therapeutic management were reported.
Limitations
Although the analysis of the outcomes was carried out among the total of participants and also among the survivors, this data could require a more careful interpretation, since the observed mortality constitutes a competitive risk.
The proposed modalities were considered with the same hierarchy. However, there is evidence in favor of superior benefits in terms of the use of respiratory physiotherapy compared to mobilizations.
Conclusions
No statistically significant differences were found in favor of the application of the MRP in terms of reduction of days of ICU stay and days of mechanical ventilation. In an exploratory way, the use of indicators made it possible to quantify the intervention and it was possible to determine that the iMR was related to the VFDs-28 and mortality.
Recommendations
Quantifiable work models that detail the interventions applied in ICUs are required because there are reports that do not specify, for example, the components of respiratory physiotherapy or modes of mobilization.
The security parameters could be expanded, assessing risk benefit, allowing a higher percentage of execution of the recommended modalities.