INTRODUCTION
Self-medication -defined as the consumption of a product for preventing or treating an illness or disease without a doctor's prescription- is a common practice with widely documented adverse effects1,2. Self-medication is a relevant problem in Latin America and low- and middle-income countries, where a poorly regulated pharmaceutical market has been described3,4. Because of its adverse effects, it is a major public health concern, as it exposes the population to increased drug resistance, serious side effects or delayed medical attention5.
Due to the new coronavirus disease (COVID-19), self-medication has increased6 in the face of excessive hospital demand which health systems have been unable to cope with7,8. Given the lack of responsiveness, a high prevalence of self-medication has been reported, especially in people at higher risk of infection9-12. Absence of a pharmacological treatment for the disease or fear about becoming seriously ill12) have been suggested as the main reasons for self-medication.
In a context where health systems are at their maximum capacity, the work of pharmacists is essential, as they represent the most accessible and sometimes the first link between the patient and the health system13. In Peru, their functions are regulated by the General Health Law, which establishes that they are responsible for "dispensing, information and guidance to the user on the administration, use and dosage of the pharmaceutical product"14. Within Pharmacy training, emphasis is placed on their role as a link between the general population and the health system, being fundamental in times of health crisis, ensuring optimal pharmacological management and communication strategies to avoid self-medication15.
University pharmacy students in their final year are already exposed to pre-professional internships, in health services pharmacies, where they have first-hand experience with the population and with self-medication practices increased even further under the uncertainty of the pandemic; therefore, they could give an idea of the real dimension of the problem of self-medication during the COVID-19 pandemic.
For these reasons, the present study sought to describe the perceptions of students and faculty of a Pharmacy School of a Peruvian public university on the self-medication of the population in the context of the COVID-19 pandemic. These results will serve as a basis for defining strategies to address the problem, with an emphasis on the populations that are perceived to be most predisposed to self-medication.
MATERIAL AND METHODS
Design and setting
The present study is an exploratory, cross-sectional research. The sampling was non-probabilistic. Students in the final year of the Pharmacy and Biochemistry course at a major public Peruvian university were recruited.
Data collection
For data collection, the research team developed a questionnaire made up of questions related to socio-demographic variables, characteristics of self-medication of the population and factors associated with self-medication in the COVID-19 pandemic. Seven experts participated in its validation. Each item was analyzed in terms of content validity, i.e. whether the questions were needed to understand perceptions about the phenomenon of self-medication, applicability, and feasibility (clear wording and coherence). The questionnaire was distributed a total of students in the final year of the Pharmacy and Biochemistry course at a major public Peruvian university.
Data analysis
To analyze data, the research team measured socio-demographic variables, characteristics of self-medication and associated factors in the context of the COVID-19 pandemic. The study described categorical variables using absolute and relative frequencies; quantitative variables were expressed as mean and standard deviation. Statistical analysis and graphs were performed with the open-source software RStudio v. 1.3.1073.
RESULTS
A total of 360 students were invited to participate of which 274 responded and were included in the study (76.1%). 55.8% were women and the mean age was 23.3 ± 4.5 (See table 1). Of the total number of respondents, 80.3% reported having knowledge of someone who self-medicated during the COVID-19 pandemic. Figure 1A presents these results differentiated by the person who self-medicated. Respondents reported that their family members (52.3%) and friends (40.1%) most frequently self-medicated during the pandemic.
Table 1 Characteristics of the studied sample
| Characteristic | Total (n=274) | Yes (n=220) | No (n=54) | p value |
|---|---|---|---|---|
| Age | 23.27± 4.5 | 23 (21-24) | 22 (20-24) | 0.144 |
| < 25 | 212 (77.4) | 168 (76.4) | 44 (81.5) | 0.717 |
| 25 - 39 | 58 (21.2) | 48 (21.8) | 10 (18.5) | |
| > 40 | 4 (1.5) | 4 (1.8) | 0 | |
| Sex | ||||
| Male | 119 (43.4) | 91 (41.4) | 28 (51.9) | 0.316 |
| Female | 153 (55.8) | 127 (57.7) | 26 (48.2) | |
| Other | 2 (0.7) | 2 (0.91) | 0 |
Participants were grouped according to whether or not they perceived self-medication increased during the pandemic. Values are mean ± SD or frequency and percentage n (%).
Pharmacies (79.2%) and apothecaries or drugstores (76.3%) are the most frequent places where medicines are obtained (Figure 1B). The most common perceived reason for self-medication was the occurrence of a COVID-19 symptom (Figure 1C). while the pharmacy technician (53.3%), a family member (47.1%) or acquaintance who has had COVID-19 (48.9%) are the most frequent persons who indicate the medicine (Figure 1 D).
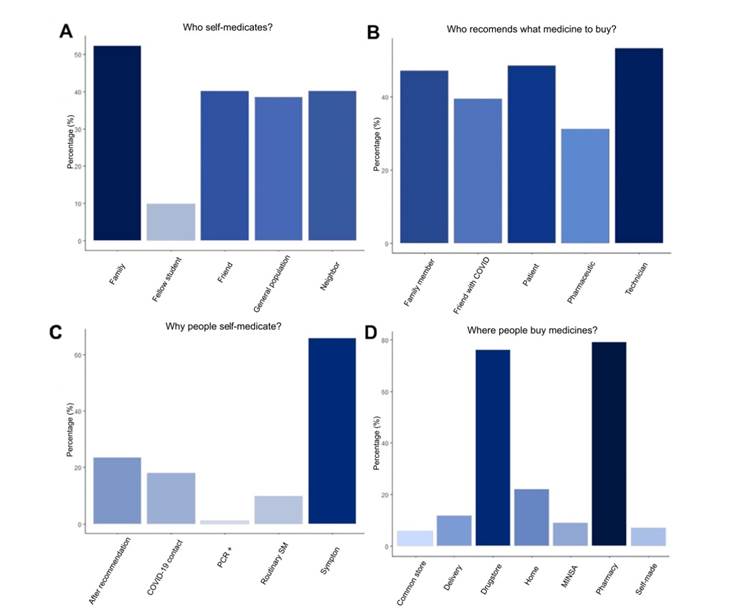
Figure 1 Legends of figures. Pharmacy students’ perceived reasons regarding who self-medicates the most (A), the person recommending the medicines (B), reasons for self-medication and places where people buy medicines (D) in the context of the COVID-19 pandemic. SM: Self-medication, MINSA: Peruvian Minister of Health.
The main symptoms for which a person self-medicates are sore throat (68.3%), cough (61.1%) and general malaise (46.7%). 96.4% consider that COVID-19 increased self-medication. The main causes identified by respondents are lack of treatment (47.2%), lack of vaccine availability (48.7%) and the belief that there are no effects associated with self-medication (59.9%). No respondent considered lack of awareness of self-medication as a reason for the phenomenon.
Ivermectin (79.2%), azithromycin (71.2%), paracetamol (69.3%) and dexamethasone (62.4%) are considered the most consumed drugs in the pandemic by COVID-19. To a lesser extent, hydroxychloroquine (38.7%), vitamins and minerals (32.5%), chlorine dioxide (31.3%) and warfarin (22.9%). The most frequent adverse effects were vomiting (58.3%), diarrhea (46.4%), renal (33.2%), respiratory (30.6%) and hepatic (30.1%) failures. Perceptions of the students on the effects of self-medication on the treatment of COVID-19 are also presented (see table 2).
Table 2 Perceptions of the adverse effects of self-medication and consequences of medication on COVID-19 treatment
| Adverse effect | Yes | No | % Yes |
|---|---|---|---|
| Nausea/Vomiting | 114 | 160 | 58.39 |
| Diarrhea | 127 | 147 | 46.35 |
| Renal failure | 91 | 183 | 33.21 |
| Acute hepatic failure | 82 | 191 | 30.04 |
| Respiratory failure | 84 | 190 | 30.66 |
| Caustic esophagitis | 54 | 171 | 24 |
| Severe dehydration | 44 | 227 | 16.24 |
| Dehydration induced hypotension | 41 | 233 | 14.96 |
| Methemoglobinemia | 27 | 187 | 12.62 |
| QT prolongation | 37 | 237 | 13.50 |
| Electrolyte disorders | 28 | 245 | 10.26 |
| Hemolytic anemia | 26 | 248 | 9.49 |
| Myocardial injury | 19 | 255 | 6.93 |
| Depends on the medicine | 5 | 267 | 1.84 |
| Anxiety | 5 | 269 | 1.82 |
| Headaches | 4 | 269 | 1.47 |
| Lower immune response | 2 | 240 | 0.83 |
Regarding the consequences, the respondants believed that antibiotic resistance was a major aftermath of the increased self-medication (74.4%). The worsening of COVID-19 symptoms (52.55%) was perceived as the second major consequence followed by lower immune response (45.26%) and delayed medical care (39.78%) (Table 3).
DISCUSSION
The study aimed to characterize Pharmacy faculty and student’s perception of self-medication in the Peruvian population in the context of the COVID-19 pandemic. A significant majority considered that self-medication increased significantly during the pandemic due to the general feeling of anguish towards a new disease with no available treatment. These results are consistent with other studies that identify anxiety about the new disease as the main cause of self-medication6,12,16.
In our study, respondents reported that it is the onset of symptoms associated with COVID-19 that triggers self-medication. As is well known, the symptoms of the disease are diverse17. This result is consistent with other findings in Peru12, Bangladesh9 and Togo10. However, these studies found people who reported self-medicating even without having symptoms9.
In the study, respondents identified pharmacies and drugstores as the places where medicines are most frequently obtained, and it is the pharmacy technician who prescribes the medicine to take, followed by a family member or acquaintance who has had COVID-19 and pharmacists. The adverse effects of self-medication may be unknown to the community; however, health professionals and pharmacy technicians do acquire competencies on these issues throughout their training. A study of pharmacy technicians found a high level of knowledge of adverse drug reactions to ivermectin, azithromycin and dexamethasone for the treatment of COVID-1918.
In the study, ivermectin and azithromycin were identified as the most frequently used by the population. Other studies show that hydroxychloroquine is the most frequently used drug19-21. A study in Peru regarding pre-hospital medication revealed that 85.8% of patients used antibiotics and 66.9% used ivermectin22; However, studies on the indiscriminate use of dexamethasone, enoxaparin or chlorine dioxide have not yet been reported, despite empirical evidence to the contrary.
Regarding the adverse effects and consequences of self-medication, given the nature of the drugs perceived as most commonly used, serious adverse effects are likely to occur23. Especially anticoagulants or drugs not recommended for use in the pandemic24.
It is necessary for future pharmacists to be prepared to deal with self-medication in the community, especially if it puts people's health and lives at risk by delaying medical attention or worsening COVID-19 conditions. Community pharmacists play a vital role in the provision of medicines and health education, in response to the demands of the population who seek help in pharmacies, drugstores, etc. This is corroborated in a study conducted in Zambia, analyzing this role and concluding that pharmacists were prepared to participate in the front line against the COVID-19 pandemic25.
The study concludes that Pharmacy and Biochemistry students in Lima, Peru; perceive that self-medication practices have increased in the general population during the COVID-19 pandemic. The role of pharmacists in disseminating the risks of self-medication and indiscriminate use of drugs through health education campaigns is important. National surveillance of self-medication during the COVID-19 pandemic is needed.















