INTRODUCTION
Severe traumatic brain injury (TBI) is a leading cause of neurological dysfunction and death in the pediatric population. After medical treatment, the second level is decompressive craniectomy in cases of intractable intracranial elevation (ICP)1. Often due to lack of resources in low-income countries, invasive intracranial pressure is no longer measured, but early decompressive craniectomy is chosen, which could lead to excessive surgery and long-term neurological sequelae. Decompressive craniectomy (DC) remains a controversial procedure due to its invasiveness and lack of clearly defined indications, the absence of an established surgical technique, the variability of its results, and the significant risk of complications2.
The mortality rate among survivors of gunshot wounds to the head is extremely high. Kaufman estimated that more than 90% of those who sustained gunshot wounds to the head ultimately died, two-thirds of whom died on the scene4,5, primarily due to respiratory arrest and circulatory arrest occurring within minutes6,7,8. The incident of gunshot wound to the head in a pediatric case is rarely reported in the literature.
Many times it is suggested that surgery should be performed immediately to avoid further injury and refractory cerebral edema due to injury, in any case, penetrating brain injury; and to achieve a good prognosis from early surgery and with adequate postoperative treatment9.
There are publications such as Matheus Manzolli et al 3, where they demonstrated a high incidence of neuropsychological deterioration in long-term follow-up in children who underwent decompressive craniectomy.
It is important to assess complications including the risk of brain infection after decompressive craniectomy in children, for which early neurological monitoring is necessary and sometimes requires external ventricular drainage and initiation of intrathecal antibiotic therapy 10.
The goal of communicating this case is to provide an individualized treatment approach in our child, especially since projectile injuries are different and unique. It highlights the urgency of further advancing pediatric neurocritical care research to positively impact the quality of life of survivors.
REPORT CASE
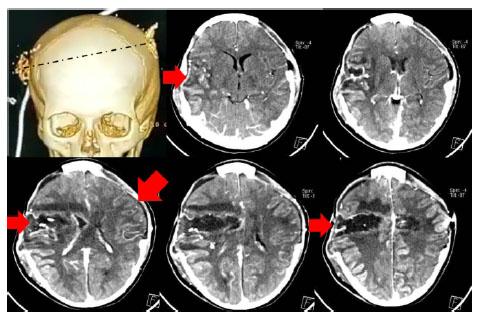
A 12-year-old boy was admitted to our hospital for a gunshot wound to the head. The patient was in a drowsy state, Glasgow 7. Physical examination revealed weak spontaneous breathing, and from the cranial puncture holes he presented hemorrhage, he presented vasoplegia and poorly reactive isochoric pupils. Computed tomography of the head showed an entry and exit hole of the bullet passing through both cerebral hemispheres with hematomas in the trajectory and with multiple bone fragments, with presence of signs of diffuse cerebral edema that led him to assisted mechanical ventilation and to the operating room. A bilateral fronto-temporo-parietal decompressive craniotomy was performed. He had elevated intracranial pressure and the brain enveloped by the dura was quite stiff and devitalized tissue from the entry site crossing both hemispheres. The entry site wound revealed small left frontoparietal hemorrhages associated with ischemic lesions in the left cerebellar hemisphere (Figure 1). In the immediate postoperative period, hemostatic, fluid infusion, hypertonic saline, analgosedation, vasoactives and metabolic correction were administered to prevent secondary lesions. After the febrile process, antibiotics were administered and an external lumbar drainage was performed as a treatment measure for the CSF fistula. Anticonvulsant treatment was administered, but the patient's condition was very unstable in the first 7 days. After improving circulatory hemodynamics, a gradual reduction of his analgosedation was started and he was assessed with Glasgow scale 7/15, poor cough reflex, swallowing defects, lower predominant flaccid quadriparesis, and hyperextension movements in the arms on painful examination. Brain TC at 17 days described a lesion in the brain showing a right herniation, hemorrhagic and ischemic areas in the left cerebellar hemisphere. After 1 month, the child evolves to a severe disability, with dependence on assisted mechanical ventilation through a tracheostomy, in medical treatment of readaptation.
Brain CT scan 17 days after injury describes bilateral fronto-temporo-parietal craniectomy with herniation of brain tissue predominantly on the right. Post-surgical changes, edema with small areas of left frontoparietal bleeding. Hypodense areas with high density elements probably right frontoparietal foreign bodies. Hypodense right frontoparietal triangular morphology compatible with ischemia and hypodense image suggestive of ischemia or focal edema in the left cerebellar hemisphere.
DISCUSSION
Penetrating skull injuries are rare in pediatric patients and the few cases encountered are caused by accident or child abuse. But the accompanying morbidity and mortality are high in children. The assessment of the Glasgow scale and tomographic images of the brain allow early decisions to be made in medical-surgical interventions. Although we often do not monitor intracranial pressure, the images are very useful in recognizing the type of penetrating lesion we are facing and that, due to its high mortality risk, early decompressive craniectomies are decided to be performed.
It is known that increased brain swelling is common in the first week after decompressive craniectomy (DC). Brain swelling may correspond to hyperperfusion, as detected on brain tomography perfusion imaging 11.
In our child, brain imaging, the type of lesion and the projectile trajectory at head level were very useful for neurosurgical intervention and to avoid cerebral circulatory arrest. Although post-decompressive craniectomy complications were frequent in our child, mortality was avoided, but he was left with severe neurological sequelae.
A recent systematic review of CD-related complications revealed that the overall complication rate was 13.4% and complications can be divided into three broad categories: hemorrhagic, infectious/inflammatory, and CSF dynamics alterations 12.
Regarding perioperative complications (first 7 days), external brain herniation is a phenomenon that occurs quite frequently (27.8% of cases in Yang et al.'s work, 51% in Honeybul's study, 14.6% in Ban et al.'s, and 25.6% in Honeybul and Ho's cohort), to the point that some authors posit that it can be considered as a natural sequela of CD 13.
A recommended CPP and ICP value has not been clearly studied for children treated with decompressive craniectomy (DC) and to avoid further complications, with the aim of maintaining optimal cerebral autoregulation and avoiding long-term neurological sequelae.
The phenomenon of increased cerebral edema, usually seen in the first week post-decompression, may be encountered. This increased edema may result from cerebral hyperperfusion, as well as a drop in interstitial hydrostatic pressure 14,15.
Ischemic phenomena, in turn, may maintain or augment the parenchymal herniation of the craniectomy through a breach in the dura, leading to the need for reoperation to resect the devitalized tissue and perform a wide dural plasty. One of the most important factors in minimizing external herniation is performing craniectomies wide enough to allow the brain to expand without constriction 16. There is little information on the approach and extent of decompressive craniectomies according to pediatric ages.
Generally, children with penetrating injuries with GCS scores <6 on admission, the presence of intraventricular hemorrhage on the first CT scan of the head, and the need for bilateral CD could be used to predict whether patients with post-CD traumatic brain injury will develop posttraumatic hydrocephalus 17.
Post-traumatic hydrocephalus (PTH) is common in patients undergoing decompressive craniectomy (DC) for traumatic brain injury (TBI), but the incidence, mechanisms, and risk factors have not been fully elucidated.
The long-term disabilities of post-decompressive craniectomy patients can be measured according to the Glasgow Scale (GOS). Under this grading system, a GOS score of 1 indicates death, 2 indicates a persistent vegetative state, 3 indicates severe disability (conscious but disabled), 4 indicates moderate disability (disabled but independent), and 5 indicates excellent recovery with return to functional baseline.
Other complications that can be seen after decompressive craniectomy are hemorrhagic injuries including new hematoma, remote hematoma and hemorrhagic progression of contusion, wound problems such as abscesses or empyema, meningitis fall into the infectious/inflammatory category and infected CSF fistulas.
Our child presented with an infected CSF fistula receiving antibiotic coverage, and it was decided to place a spinal drainage catheter for prevention and in the post-surgical period as a treatment for CSF leaks. Its usefulness lies in Poiseuille's Law: the reduction of CSF flow through the open dural defect can be slowed by decreasing the CSF pressure difference between the intradural and extradural space through the lumbar CSF shunt, allowing the dural gap to heal 18,19.
However, the use of spinal drainage catheter temporarily for 5-7 days allows the dura defect to heal, with a success rate of 85%-94% 20. This allowed us to improve the CSF fistula of our pediatric patient.
While decompressive craniectomy reduces mortality, it may not rescue neurologic function from devastating injury caused by primary impact or secondary damage that develops during the early resuscitation period. Survival risks with a persistent vegetative state outcome after decompressive craniectomy have been reported to range from 15-20% in many series.
Our limitation in this clinical case was not measuring intracranial pressure at admission, due to the risk of cerebral circulatory arrest, and not having a monthly follow-up of his neurological functional status and disability after hospital discharge. These points are key to making appropriate decisions in long-term management.
CONCLUSION
The indication for Decompressive Craniectomy should be individualized for each pediatric patient, assessing their previous health status, type of injury and disease, experience of the treatment team, and the decision should always be consensual between at least a pediatric intensivist and a neurosurgeon.