Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.62 no.2 Lima abr./jun. 2016
ARTÍCULO ORIGINAL
Barriers to acc ess to safe abortion in the full extent of the law in Peru
Barreras para el aborto seguro en el marco de la ley peruana
Luis Távara Orozco1, Pilar Macharé2, Segundo García Angulo2, Enrique Guevara2, Santiago Cabrera2, Julio Aguilar2, Ysoé Ramírez2, Luis Orderique2, Carlos Silva2, Sixto Sánchez2, Walter Leveau2, Jhonny Burela2
1 Coordinador Regional para América del Sur. Iniciativa FIGO Prevención del Aborto Inseguro. Presidente del Comité de Derechos Sexuales y Reproductivos de la Sociedad Peruana de Obstetricia y Ginecología.
2 Jefe de Departamento/Servicio Hospitales del Ministerio de Salud del Perú
Abstract
Purpose: To examine the historical process for institutionalization of therapeutic abortion in Peru and to explain its current condition. Methodology: Review of bibliographic information available in the country regarding the process conducted by many institutions to have the Ministry of Health approve the National Guide for Therapeutic Abortion. Subsequently, the lead researcher met with 10 heads of the Gynecology and Obstetrics Service/Department from the same number of hospitals, from whom he requested information, as they have been regulating the provision of therapeutic abortion services by means of local Guides or Protocols for the last 5 years. Results: The formalization of the National Guide for the provision of therapeutic abortion services by the Ministry of Health has been a persistent endeavor of many institutions of civil society, but the 10 convened hospitals have already been responding to the demand for the past 5 years. In these 5 years, 257 therapeutic abortions were performed. The frequency of therapeutic abortions is still low; however, there is a progressive increase over the years. The frequency of therapeutic abortions is predominant in the second trimester of pregnancy, with congenital anomalies incompatible with life being the most frequent cause. Misoprostol to evacuate the uterus has been used in 95% of the cases, and only 2% minor complications have been verified.
Keywords: Abortion, Legal; Abortion, Induced; Abortion, Therapeutic.
Resumen
Objetivo: Examinar el proceso histórico para institucionalizar el aborto terapéutico en el Perú y precisar su situación actual. Metodología: Revisión de la información bibliográfica existente en el país en relación al proceso seguido por muchas instituciones hasta conseguir que el Ministerio de Salud apruebe la Guía Nacional para el Aborto Terapéutico. Luego el investigador principal convocó a 10 jefes de servicio/departamento de Ginecología y Obstetricia de igual número de hospitales que tienen regulada la prestación de servicios de aborto terapéutico mediante Guías o Protocolos locales desde 5 años antes, a quienes se les solicitó información. Resultados: La oficialización de la Guía Nacional para la prestación de servicios de aborto terapéutico por parte del Ministerio de Salud ha sido un trabajo persistente de muchas instituciones de la sociedad civil, pero los 10 hospitales convocados ya venían respondiendo a la demanda desde 5 años atrás. En los 5 años se atendió 257 abortos terapéuticos. La frecuencia del aborto terapéutico es aún baja, sin embargo se aprecia un aumento progresivo conforme avanzan los años. Es predominante la frecuencia de abortos terapéuticos en el segundo trimestre del embarazo, siendo la causa más frecuente las anomalías congénitas incompatibles con la vida. El uso del misoprostol en la evacuación del útero ha alcanzado el 95% de los casos y no se ha verificado más de 2% de complicaciones leves. Conclusión: El aborto legal por causales de salud se viene ofertando en forma restringida en el Perú.
Palabras clave: Aborto, Legal; Aborto, Inducido; Aborto, Terapéutico.
Introduction
While therapeutic abortion (TA) is legal in Peru since 1924(1), only recently (June 2014) the Ministry of Health approved the National Guide for Voluntary Termination of Pregnancy for Therapeutic Reasons(2); however, Peruvian women still do not have an adequate access to these services in public hospitals. To a great extent, this is why indirect causes of maternal death are occurring more frequently each time(3).
Healthcare professionals of public facilities that provide sexual and reproductive health services lack sufficient information and are still biased against women who terminate their pregnancies and the professionals who take care of them; this takes place because there is no established standard care for women and professionals.
Civil society, the Peruvian Society of Obstetrics and Gynecology (SPOG), physicians, and women organizations, have displayed intense activity in Lima and in the country regions, in order to discuss and approve local guides and protocols for TA attention, having been able to follow through in 10 hospitals. Likewise, they carried out activities to improve attention in those facilities, to extend care and improve the quality of services.
From reviewing national literature, we have been able to learn that legalization of abortion for medical reasons exists in the Peruvian Criminal Code (CPP) since 1924(1), the foregoing being endorsed in the review of the same Code in 1991. Article 119 of the CPP reads as follows: "Abortion performed by a doctor, with the consent of the pregnant woman or her legal representative, if there is one, is not punishable if it is the only way to save her life or avoid serious and permanent damage to her health."
Despite the enactment of the law approved by the CPP, it has not been systematically applied due to the lack of a Clinical Guide or a Regulation that standardizes its implementation. On the other hand, notwithstanding this deficiency, in the past 50 years, some hospitals have been providing therapeutic abortion services, particularly in Hospital San Bartolomé and Instituto Nacional Materno Perinatal (former Maternidad de Lima).
Methodology
For carrying out this study, the main author reviewed national literature regarding therapeutic abortion and made use of his own experience; in addition, he requested the participation of heads of the Gynecology and Obstetrics Service/Department of 10 hospitals nationwide. It is worth mentioning, among the features of these hospitals that they are second- or third-level complexity hospitals, affiliated to national or private universities with a Medical School, and have had a Guide or Protocol for the provision of TA services 5 years ahead of this research.
Each of the local authors that participated in the study answered the following questions formulated by the main author:
-
Number of abortions performed in each service/department from 2010 to 2014
-
Number of legal abortions (therapeutic) performed from 2010 to 2014
-
Reasons for therapeutic abortion(4)
-
Pregnancy timeline at the time of termination
-
Methods for the termination of pregnancy(5)
-
Complications in the procedures for termination of pregnancy
All compiled information was received by the lead researcher, it was processed and subsequently, tables and graphs were made, which can be found in the Results section.
Ethical aspects
This study did not interview professionals, or users of the services, nor did it review the medical records in detail. Only the clinical records of the Gynecology and Obstetrics Service or Department were reviewed to determine the provision of therapeutic abortions. This was carried out with the authorization of the hospital authorities. None of the researchers received any sort of remuneration or economic stimulus.
Results
Review of National Literature
The revision of the national literature outlined that legalization of abortion for medical reasons exists in the Peruvian Penal Code (PPC) since 1924(1), which was endorsed on review of the same code in 1991(6). Article 119 of the code reads as follows "An abortion performed by a doctor with the consent of the pregnant woman or her legal representative, if she had it, is not punishable when it is the only way to save her life or avoid serious and permanent damage to her health".
Notwithstanding the enactment of the law which approves the PPC, this has not been systematically applied by lack of a Clinical guide or Regulations governing the application of the law. However, in spite of this lack, some hospitals have been providing therapeutic abortion in the last 50 years, particularly in the Hospital San Bartolomé and the Instituto Nacional Materno Perinatal (former Lima Maternity).
The improvement in knowledge regarding the number and causes of maternal mortality in Peru prompted the Peruvian Society of Obstetrics and Gynecology (SPOG) to highlight the issue of abortion, organizing a national event "Seminar – Workshop on Maternal Health and Reproductive Risk, Abortion, and Sterilization," sponsored by the Ministry of Health, the Peruvian Medical Association and the National Population Council, in the year 1983(7), in which the importance of abortion in women’s health and maternal mortality was emphasized.
Ten years later (in 1993), during the XI Peruvian Congress of Obstetrics and Gynecology, there was a chance to discuss the issue of abortion in Peru(8). In 1996, during the XII Peruvian Congress of Obstetrics and Gynecology, abortion was, for the first time, the Official Theme of the Congress and the following was discussed: the epidemiology of abortion, the role of abortion in demographic transition, techniques to treat in-complete abortions and abortion prophylaxis(9).
The SPOG, in the Extraordinary Congress of Obstetrics and Gynecology in 1997, developed the Official Theme "Abortion and Reproductive Health," with the participation of leading international speakers. Likewise, a keynote conference on "Abortion: Professional Responsibility of the Obstetrician-Gynecologist"(10) was held during the Congress.
The subsequent Peruvian Congresses included in their programs themes related to abortion. At the XX Congress, held in October 2014, abortion was an Official Theme, which included a representative of FIGO as speaker.
With the arrival of the 21st century, SPOG assumed the defense of Sexual and Reproductive Rights, sponsored by FIGO and FLASOG, and one of the themes incorporated was the defense of women’s right to terminate pregnancy within the legal framework(11). That is why in the year 2005, SPOG convened a workshop with other scientific societies in the country to discuss and develop the profile of Peruvian women that could undergo therapeutic abortion, profile which was finally obtained and submitted to the Peruvian Medical Association and the Ministry of Health(12). This workshop made it possible to draft the first Guide for the provision of TA services.
The Sexual and Reproductive Rights Committee of the Peruvian Society of Obstetrics and Gynecology (SPOG), with the active participation of Civil Society institutions, assumed the responsibility of promoting the provision of TA services through awareness and training activities, and the elaboration of work Guides or Protocols in 10 hospitals, which participated with full responsibility. These Guides or Protocols, after being implemented, were discussed again, in order to enhance in-hospital facilities. The first work Guide that was published was for Hospital San Bartolomé(13), the other nine came after that.
The Peruvian Medical Association (CMP), which represents all Peruvian physicians, played an important role in the process. The High-Level Commission on Reproductive Health, which was an excellent forum for the Association to establish its position on this issue, was created in 1999. In 2007, this Commission organized a National Workshop on Sexual and Reproductive Rights, with the participation of the President of the National Council of Presidents of Peruvian Professional Associations, and Regional Presidents and representatives, as well as the Sexual and Reproductive Rights Committee of SPOG. The favorable institutional position regarding TA was established in this workshop(14). Likewise, the Ethics and Deontological Monitoring Committee of the CMP assumed the responsibility to convene in 2009 a National Workshop on Ethical Aspects of Sexual and Reproductive Health, which determined the institutional position on therapeutic abortion, having concluded that the ethical conduct of the physician must incorporate the duty of providing TA services with absolute respect for the autonomy of women, displaying the utmost care to provide the maximum benefit and avoid doing harm, as well as acting with absolute respect for justice(15).
Civil Society, and particularly women’s organizations, has been greatly supportive and displayed a leading role in this process, not only sponsoring the different events mentioned, but also carrying out excellent advocacy work in private and public institutions. Among the latter, it is worth mentioning the National Parliament and the Executive Branch. They have also built valuable technical support in different activities for the elaboration of protocols or guides and implementation of research activities(16,17). It is only fair to highlight the participation at the beginning of this process, of the NGO Flora Tristán, organization that helped with the Hospital San Bartolomé Guide(13), and NGO Promsex, which has helped to perform all the other activities described herein.
The Ministry of Health, faced with the needs of women in the country and the advocacy carried out by civil society, took a first step in the year 2005 with the establishment of a working group for the drafting of a proposal for a TA Guide or Protocol. This multi-institutional group fulfilled the assignment and completed the proposal, which almost coincided with the change of government. The proposal was diverted to Instituto Nacional Materno Perinatal (INMP).
In 2007, the General Director of INMP(18) issued a Board Resolution formalizing the TA Protocol in use. However, the Ministry of Health invalidated the resolution, and the Director was removed. In 2010, the new General Director of INMP issued a Board Resolution updating the Obstetrics and Gynecology Rules and Procedures, which included therapeutic abortion(19). This was a very important step in the national process, because it served as an incentive for the other hospitals in-volved getting the technical and administrative support of a highly specialized institution.
Despite the setback in the year 2007, a new Minister of Health of the same Government restarted the work put on hold to develop the National Guide, not being able to approve it during his administration.
With the beginning of a new government in the year 2011, the quest for the approval of the TA Protocol or Guide was resumed. The Ministry of Health started working on the written text again and sent it for consultation to different public and private institutions. The opinion of the Ministry of Justice and Human Rights was key at this new stage, be-cause, as Legal Advisor of the Government, it upheld in detail the need for a Guide, since the provision of TA services is an obligation that the Ministry of Health should comply with(20).
In addition to the opinion of the Ministry of Justice, other sectors, almost in their entirety, stated the relevance of the National Guide. Therefore, on June 2014, the Ministry of Health issued resolution 486, which finally approved this normative document(2).
The approval of the Guide sparked favorable and contrary comments and statements. SPOG and FLASOG (Latin American Federation of Obstetrics and Gynecology Societies) publicly welcomed its approval and offered their technical support to the Ministry of Health. Former Ministers of Health, Former Presidents of the Peruvian Medical Association, and prestigious Peruvian physicians spoke out publicly in favor of the Guide.
These last developments, obviously, marked the beginning of a new era, in which the Ministry of Health, together with civil society institutions, scientific societies, cooperation agencies, and private Institutions, gathered a group of heads of the Obstetrics and Gynecology Departments of hospitals all over Peru, in order to discuss the scope of the Guide and its implementation at an operational level.
All the institutions involved are contributing to the cause so that Peruvian women can exercise their right to the termination of pregnancy for medical reasons, within the framework of the law.
Current state of therapeutic abortion in Peru
The professionals convened by the lead researcher answered carefully the questions formulated. The information corresponds to the implementation of local guides and protocols in each hospital and it represented an excellent source for the elaboration of the following tables and graph.
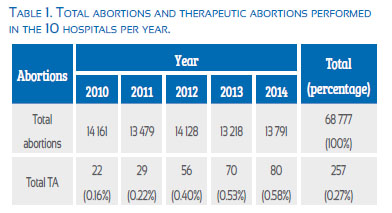
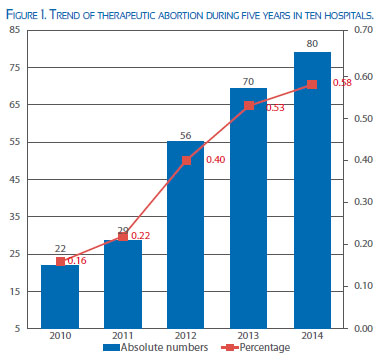
Frequency of abortion and therapeutic abortion treatment in the 10 healthcare services
As can be seen, from the total number of nearly 70 000 abortions performed in these 10 hospitals in the last 5 years, only 257 abortions have been therapeutic, which accounts for less than 1% of the total abortions. The hospital that presented the largest number of cases was INMP. Hospital de Piura presented cases in the last three years, Hospital de Pucallpa in the last two years and Hospital Dos de Mayo in Lima presented cases only in the last year. It is obvious that, as the years go by, the absolute number and the proportion of therapeutic abortions is increasing, as observed in the following graph.
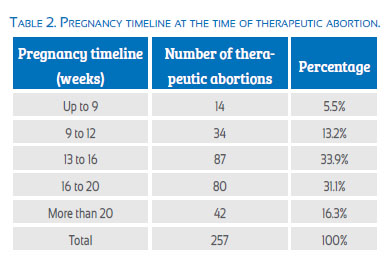
Almost 65% of the therapeutic abortions occurred between weeks 13 and 20. The TAs in the first trimester did not constitute 20% of the total.
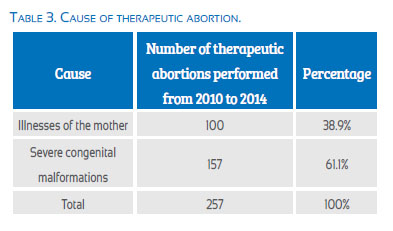
Cause of therapeutic abortion
It is worth noting that the greater amount of therapeutic abortions occurred due to congenital malformations incompatible with life, where the number of malformations dependent on the central nervous system was predominant. There were no therapeutic abortions that had rape as the cause.
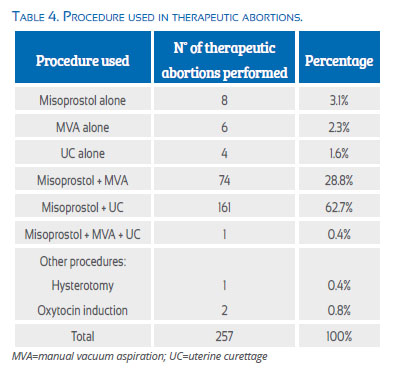
Methodology for therapeutic abortion
Table 4 presents the different forms that were used to terminate the pregnancy for medical reasons.
It can be observed that the procedures that used misoprostol + MVA and misoprostol + UC predominated. Only in 5.1% of the cases misoprostol was not used as a medical procedure.
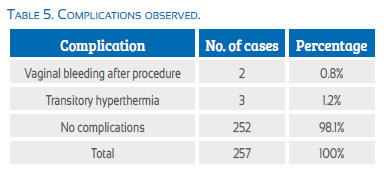
Complications
In Table 5 we can verify that the number of complications attributable to different procedures was very low. Only 2% of the cases presented some type of complication that was otherwise easy to solve. There were no severe complications or death attributable to the procedure. There wasnt any maternal death. During this period abortion was 10.7% cause of maternal mortality.
Discussion
This research study had two parts. The first consisted of a bibliographical search nationwide, which supported the different activities and participation of institutions that have been part of this long process for obtaining a National Guide. The second part has been to verify the current condition of therapeutic abortion in 10 public services that have their own guide or protocol.
Literature review shows that in Peru, despite having a law since 1924 that ensures the legality of abortion for therapeutic reasons(1), it has not been possible to provide services to women because, until recently, there was no Guide to regulate the provisions of law (first barrier)(2). This legislation puts us within the large majority of countries in the world that accept abortion when the life of the pregnant woman is in danger or when it is necessary to preserve her physical or mental health(21). It is worth mentioning that in Latin America, where unsafe abortion is very frequent and is still responsible for high maternal mortality, the abortion law is restrictive and there are 4 countries in the region where abortion is not permitted under any circumstance(22-25).
The final approval of the National Guide for provision of TA services became a valuable instrument, because the more clear and comprehensive the legal and administrative provisions are, regarding abortion permitted by law, women may have better access to services and professionals will see in these provisions support for their practice(26). There is no doubt that this approval of the Guide has been a long process that has taken many years and that it is primarily a result of the struggle of civil society. Among its long list of institutions, the Peruvian Society of Obstetrics and Gynecology has played a leading role.
During the 5 years that this study lasted, almost 70 000 abortions, of which 257 were therapeutic abortions (0.27% of total abortions), were performed in the 10 hospitals. It can be easily observed that the number and the proportion of TA are small, when compared with other reports(27). The explanation for this discovery is found in several reasons: the under-reporting of therapeutic abortion in health facilities, women’s lack of knowledge about their right to request an abortion for health reasons (second barrier)(4) and the resistance still experienced by health professionals to provide this service (third barrier).
However, when we study the frequency of TA, we encounter an interesting finding. Table 1 and Figure 1 express the way the absolute numbers and proportion of abortions are increasing every year. We have no doubt that now with the National Guide being available, the demand will be higher and, obviously, the delivery of services will be equally higher.
The examined table reveal that 65% of therapeutic abortions occurred between week 13 and 20 of pregnancy and that less than 20% of the cases were performed before week 12 (fourth barrier). This finding contrasts with what was reported in a study carried out in India where 82% of induced abortions occurred in the first trimester(28). It is known that fewer complications in abortion procedures occur when these are performed at an early gestational age. The delay in seeking a therapeutic abortion can be explained by women’s lack of education and information (fourth barrier)(29), for the causes that determined the termination of pregnancy mainly due to congenital anomalies incompatible with life, whose identification is frequently delayed until the second trimester (fifth barrier), and by the excessive paperwork that women must complete before the procedure takes place (sixth barrier).
Because of what we found, we verified if there were changes in the chronology of TA in different years, however we found no differences.
More than 60% of TA was caused by congenital malformations incompatible with life, which were located predominantly in the central nervous system. Nearly 40% of therapeutic abortions had a major illness in pregnant women as the cause. However, despite the frequency of rape in the country and the significant number of pregnancies(30,31) that arise from it, we have not found cases attended for this cause. There is no doubt that an important factor is the express prohibition of abortion for this cause in Article 120 of the Peruvian Criminal Code(6). We examined the occurrence of TA in a country like Australia and verified in a report that the most frequent causes were related to psychiatric indications, cancer, and heart diseases(32); and when we examined the TA performed in Italy, the most common causes in the second trimester were related to genetic and congenital anomalies of a structural nature(33).
Of the total cases of TA, 95% were solved with the administration of misoprostol and some other additional procedure. WHO recommendations were followed for the use of misoprostol(5). When there will be available more information on doctors and users, and when women will be empowered with respect to their right to therapeutic abortion, we have no doubt that the use of misoprostol will be more frequent and at an earlier gestational age, since this drug provides security and privacy to women. Women appreciate very much the possibility of keeping their abortions private, they are able to choose the day and place of their abortion, by means of a non-invasive procedure, without the use of surgery or anesthesia and with confidence in its effectiveness(34,35).
The TA performed in Peruvian hospitals constitutes a legal procedure and as such it is carried out in a transparent manner using the most appropriate medical and surgical procedures that avoid significant risk for women(5,34,35). The results obtained in this series confirm the safety of the medical and surgical procedures used. Of complications found, 2% confirm this statement, being these complications mild and expected when using misoprostol. No serious complication or maternal death was found, but during these 5 years, abortion was cause of 10.7% of maternal deaths(36). These findings increase confidence in users and providers.
After TA procedures were completed, the users received counseling and were offered contraceptives. Between 70% and 80% of them received a contraceptive when they were discharged, usually hormonal, to prevent the recurrence of a pregnancy and, as a result, of an abortion. Long-acting reversible contraception (LARC) that offers high efficiency was not used in the desired magnitude.
Final remarks
As it has been stated above, the approval of the National Guide for the provision of Therapeutic Abortion services is an achievement of Civil Society and should be used for the expansion and enhancement of services. The results of this study were largely obtained before the approval of the National Guide, only with the existence of Guides or Protocols discussed and approved previously at each hospital and with adherence to the law.
We have no doubt that dissemination of the National Guide should ensure an extension and improvement of the services; however, it is essential to perform some actions as soon as possible to achieve this goal:
-
Provide more information and education to the users, empowering them in their right to the legal termination of pregnancy for medical reasons. The participation of civil society organizations is key to achieve this aspect
-
Remove some administrative restrictions to facilitate access to therapeutic abortion
-
Train healthcare providers on the National Guide and provide detailed discussion of TA procedures
-
Reinforce providers’ knowledge on bioethical and value clarification aspects related to the provision of TA services, in accordance with recommendations from FIGO, FLASOG and experts in bioethics(37-39)
-
Enhance counseling and provision of post-abortion contraceptives, emphasizing the use of LARC
-
Incorporate misoprostol to the National List of Drugs for obstetric use
-
Strengthen the alliances between civil society and the Ministry of Health.
References
1. Código Penal Peruano 1924. [ Links ]
2. Ministerio de Salud. Resolución Ministerial 486. Guía Técnica Nacional para la Atención Integral de la gestante en la Interrupción Voluntaria, por Indicación Terapéutica, del embarazo menor de 22 semanas, con consentimiento informado en el marco de lo dispuesto en el Artículo 119 del Código Penal. Lima: Ministerio de Salud, Junio 2014. [ Links ]
3. Ministerio de Salud. Dirección General de Epidemiología. La Mortalidad Materna en el Perú 2002-2011. Lima, Perú: DGE, 2013. [ Links ]
4. FLASOG. La Mesa por la Salud y la Vida de las Mujeres, Andar. Causal Salud, interrupción legal del embarazo, ética y derechos humanos. México: Mesa por la salud y la vida de las mujeres, Alianza Nacional por el derecho a decidir, 2008. [ Links ]
5. WHO. Safe Abortion, second edition. Geneva: WHO, 2012. [ Links ]
6. Código Penal Peruano 1991. [ Links ]
7. Sociedad Peruana de Obstetricia y Ginecología. Seminario Taller Salud Materna y Riesgo Reproductivo, Aborto y Esterilización. Lima: SPOG, Enero 1983. [ Links ]
8. Sociedad Peruana de Obstetricia y Ginecología. XI Congreso Peruano de Obstetricia y Ginecología 1993. Tomo del Congreso. Lima: SPOG 1994. [ Links ]
9. Sociedad Peruana de Obstetricia y Ginecología. XII Congreso Peruano de Obstetricia y Ginecología 1996. Tomo del Congreso. Lima: SPOG 1997. [ Links ]
10. Sociedad Peruana de Obstetricia y Ginecología. Congreso Extraordinario de Obstetricia y Ginecología 1997. Lima: SPOG 1998. [ Links ]
11. Sociedad Peruana de Obstetricia y Ginecología. Responsabilidad Médica frente a la interrupción legal del embarazo. Lima, Perú: SPOG-CMP-Flora Tristán, 2004:38 pp. [ Links ]
12. Sociedad Peruana de Obstetricia y Ginecología. Taller de Sociedades Médicas para identificar el perfil clínico para el aborto terapéutico. Lima, Perú: Comité de derechos sexuales y reproductivos, Agosto 2005. [ Links ]
13. Hospital Nacional Docente Madre Niño San Bartolomé. Protocolo de Manejo de casos para la interrupción legal del embarazo. Lima, Perú: CMP-Flora Tristán, 2005. [ Links ]
14. Colegio Médico del Perú. I Taller Nacional sobre Derechos Sexuales y Reproductivos. Lima, Perú: Comisión de Alto Nivel de Salud Reproductiva del CMP 2007:27 pp. [ Links ]
15. Colegio Médico del Perú. Seminario Taller Bioética y Salud Sexual y Reproductiva. Lima, Perú: Comité de Vigilancia Ética y Deontológica del CMP 2009:47 pp. [ Links ]
16. Cabrera S, Gutierrez M, Mascaro P, Silva C, Távara L. El aborto terapéutico desde los servicios de salud. Lima, Perú: Promsex 2008:40 pp. [ Links ]
17. Ayala F, Cabrera S, Chumbe O, Mascaro P, Silva C, Távara L, Liviac V, Torres G. Interrupción terapéutica del embarazo por causales de salud. Lima-Perú: Promsex 2009:41 pp. [ Links ]
18. Instituto Nacional Materno Perinatal. Resolución Directoral 0031-DG-INMP- 2007 Guía para la atención integral del aborto Terapéutico. Lima, Perú 2007. [ Links ]
19. Instituto Nacional Materno Perinatal. Resolución Directoral 152-DG-INMP- 10. Guía de Práctica Clínica y de Procedimientos en Obstetricia y Perinatología. Lima, Perú 2010. [ Links ]
20. Ministerio de Justicia. Opinión sobre el proyecto Guía Técnica para la Atención Integral de la Interrupción Voluntaria por indicación terapéutica del Embarazo menor de 22 semanas, con consentimiento informado. Miraflores, Lima 29 abril 2013. [ Links ]
21. WHO. Maternal mortality 2000: estimates by WHO, UNICEF, UNFPA. Geneva: WHO 2003. [ Links ]
22. Molina R. Editorial. Aspectos bioéticos del aborto en Chile. Rev Chil Obstet Ginecol. 2013;78(4):259-61. [ Links ]
23. Romero M, Abalos E, Ramos S. La situación de la mortalidad materna en Argentina. El Objetivo de desarrollo del milenio 5. Hoja informativa N° 8. Buenos Aires: Observatorio de Salud Sexual y Reproductiva. Marzo 2013. [ Links ]
24. Ahman E, Shah IH. Unsafe abortion: global and regional estimates of the incidence of unsafe abortion and associated mortality 2008. Geneva: WHO 2011. [ Links ]
25. Kalonda JC. Sexual violence in Congo-Kinshasa: necessity of decriminalizing abortion. Rev Med Brux. 2012;33:482-6. [ Links ]
26. Boland R. Second trimester abortion laws globally: actuality trends and recommendations. Reprod Health Matters. 2010;18:67-89. [ Links ]
27. Piel B, Azria E, Oury JF, Carbillon L, Mandelbrot L. Termination of pregnancy for maternal indications in the Paris area: a retrospective multicenter study in the period between the 2011 French law on termination of pregnancy and the bioethics law. J Gynecol Obstet Biol Reprod (Paris). 2013;42(4):342-50. [ Links ]
28. Banerjee SK, Andersen KL, Warvadekar J. Consequences of unsafe abortion on morbidity and mortality. Pathways and consequences of unsafe abortion: A comparison among women with complications after induced and spontaneous abortion in Madhya, Pradesh, India. Int J Gynecol Obstet. 2012;118 (Supp 2): S113-S120. [ Links ]
29. de Toledo M, Drezzett J, et al. Factors associated to late term abortion after rape. Reproducao e Climatério. 2014. http:// dx.doi.org/10.1016/j.recli2004.08.003. [ Links ]
30. Távara L. Sexual violence. Best Practice & Research Clinical Obstetrics and Gynaecology. 2006;20(3):395-408. [ Links ]
31. Távara L, Jacay S, Dador MJ, Chávez S. Apuntes para la acción: El derecho de las mujeres a un aborto legal. Lima: PROMSEX/ IPAS/IWHC/PPFA, Setiembre 2007:110 pp. [ Links ]
32. Barrett HL, Lust K, Callaway LK, Fajermo N, Postman C. Termination of pregnancy for maternal medical indications: failings in delivery of contraceptive advice?. Aus NZ J Obstet Gynaecol. 2011;51(6):532-5. [ Links ]
33. Bastianelli C, Farris M, Aliberti C, Parenchini M. Second- trimester induced abortion in two tertiary centres in Rome. Eur J Contracep Reprod Health Care. 2014;19(2):121-7. [ Links ]
34. Ramos S, Romero M, Aizenberg L. Womens experiences with the use of medical abortion in a legally restricted context: The case of Argentina. Reproductive health Matters. 2014;Suppl 43:1-12. [ Links ]
35. Gomperts RJ, Jelinska K, Davies S. Using telemedicine for termination of pregnancy with mifepristone and misoprostol in setting where there is no access to safe services. BJOG. 2008;115(9):1171-5. [ Links ]
36. Ministerio de Salud. Dirección General de Epidemiología. La mortalidad materna en el Perú 2002-2011. Lima,Perú: Dirección General de Epidemiología 2013. [ Links ]
37. FIGO. Ethical Issues in Obstetrics and Gynecology. London, KU: FIGO Committee for study of Ethical aspects of Human Reproduction and Womens Health, Oct 2009. [ Links ]
38. Federación Latino Americana de Sociedades de Obstetricia y Ginecología. Taller Marco bioético y clarificación de valores en la prestación de servicios de salud sexual y reproductiva. Panama: FLASOG Junio 2010. [ Links ]
39. Cook R, Dickens BM, Fathalla MF. Salud Reproductiva y Derechos Humanos. Bogotá, Colombia: Profamilia 2003:605 pp [ Links ]
Correspondencia: Dr. Luis Távara Orozco Los Almendros 265-103. Residencial Monterrico, La Molina, Lima, Perú luis.tavara@gmail.com
Artículo recibido el 13 de abril de 2016 y aceptado para publicar el 27 de mayo de 2016.