Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.62 no.4 Lima oct. 2016
SIMPOSIO EMERGENCIAS Y COMPLICACIONES SEVERAS OBSTÉTRICAS
The burden of severe maternal morbidity in contemporaneous Obstetrics
El lastre de la morbilidad materna severa en la Obstetricia contemporánea
Julio Mateus, MD, PhD1
1 Assistant Professor, Medical University of South Carolina, Charleston, South Carolina, USA
Abstract
Maternal health is deteriorating across the world due to multiple factors including increasing rates of obesity, chronic medical conditions such as chronic hypertension, type II diabetes, and cardiovascular disease, as well as advanced maternal age by the time of conception. These factors summed to the increasing cesarean delivery rate, lack of standardization of clinical practices, and inappropriate care during obstetrical urgencies are all major contributors to the rising rates of major obstetrical complications and maternal death. In recent years, national and international health care organizations have proposed new definitions of major maternal morbidity. The World Health Organization (WHO) defines "near maternal miss" (NMM) as the series of events leading from good health to a life-threatening complication associated with organ dysfunction or failure. Conversely, the Centers for Disease Control and Prevention (CDC) in United States classify "severe maternal morbidity" (SMM) if a pregnancy is complicated by one or more of twenty five ICD-9 clinical complications/procedures associated with a high maternal mortality risk. Although, each organization uses a different approach, existing data indicate that diagnostic criteria used for the CDC or the WHO accurately predicts pregnancies complicated with a "true" life-threatening maternal complication. These definitions are essential to better understand the burden of the disease. Each hospital providing maternal health care should adopt the definition that better fits its own health care system and is urged to incorporate initiatives that can reduce preventable major maternal complications. A fundamental step to address this issue is the establishment of a standardized review or audit process conducted by a multidisciplinary team that assesses systematically cases of severe maternal morbidity and mortality, evaluates deficiencies of health care at the provider, institution, and system levels, and adopts programs to improve quality of care. Maternal warning systems, composed by a set of abnormal physiological parameters that alert the provider about the deterioration of the patient’s condition and prompt immediate bedside assessment, have shown to be effective in reducing maternal morbidity and mortality. Of importance, it has been recently demonstrated that linking these warning systems to standardized evidence-based clinical guidelines that address the most common obstetrical clinical pathways provides further benefits to the patient’s care and improves outcomes. Despite the advances in the early detection and management of major maternal morbidity, there is a concise need of further research to standardize definitions at regional, national and international levels, validate the effectiveness of early warning systems in different clinical settings, improve long-term outcomes, and incorporate other preventive measures initiated even prior to conception to further decline the rates of serious maternal complications and death.
Keywords: Cardiovascular Disease; Obstetrical Hemorrhage; Preeclampsia; Severe Maternal Morbidity; Maternal Near Miss; Maternal Mortality
Resumen
La salud materna se está deteriorando en el mundo debido a múltiples factores, entre los cuales se encuentran el incremento de las tasas de obesidad, las enfermedades crónicas como la hipertensión crónica, la diabetes mellitus tipo II y la enfermedad cardiovascular, así como la edad materna avanzada al momento de la concepción. Estos factores sumados a la mayor tasa de cesáreas, la falta de estandarización de la práctica clínica y la atención inapropiada de las urgencias obstétricas son las que contribuyen tremendamente al incremento de complicaciones obstétricas graves y muerte materna. En años recientes, las organizaciones de salud nacionales e internacionales han propuesto nuevas definiciones de la morbilidad materna severa. La Organización Mundial de la Salud (OMS) define ‘morbilidad materna extrema’ (MME) como una serie de ocurrencias que parten de la buena salud y se complican al punto de poner en riesgo de muerte por disfunción o falla orgánica. Al contrario, los Centros para el Control y Prevención de las Enfermedades (CDC) en los Estados Unidos clasifican como ‘morbilidad materna grave’ (MMS) si un embarazo se complica con una o más de las veinticinco complicaciones/procedimientos clínicos de la Clasificación Internacional de Enfermedades (ICD-9) asociados con un riesgo alto de mortalidad materna. Aunque cada organización emplea una aproximación diferente, la información existente indica que los criterios diagnósticos utilizados por el CDC o la OMS predicen con mucha precisión aquellas gestaciones complicadas con una ‘verdadera’ complicación materna que amenaza su vida. Estas definiciones son esenciales para comprender mejor la dimensión de la enfermedad. Cada hospital que provee atención de la salud materna deberá adoptar la definición que mejor se adapte a su propio sistema de salud y es urgido a incorporar iniciativas que puedan reducir las complicaciones maternas severas. Un paso fundamental para resolver este aspecto es establecer una revisión estandarizada o proceso de auditoría conducido por un equipo multidisciplinario que analice sistemáticamente los casos de morbilidad y mortalidad materna grave. Este equipo está encargado de evaluar las deficiencias de los proveedores de salud, de la institución y de los niveles del sistema. Además, tiene la obligación de implementar programas que mejoren la calidad de la atención. Los sistemas de alarma materna, compuestos por un grupo de parámetros fisiológicos anormales, han sido creados con el objetivo de alertar al proveedor sobre el deterioro de las condiciones de la paciente, exigiendo una pronta evaluación, reduciendo así la morbimortalidad materna. Recientemente se ha demostrado que al unir estos sistemas de alarma a las guías clínicas estandarizadas y basadas en la evidencia que están dirigidas a las complicaciones clínicas obstétricas más comunes permite mayores beneficios para el manejo de la paciente y mejora los resultados clínicos. A pesar de los avances en la detección y manejo temprano de la morbilidad materna severa, existe una necesidad de mayor investigación para estandarizar las definiciones a nivel regional, nacional e internacional y validar la efectividad de los sistemas de alarma temprana en diferentes escenarios clínicos. Además, es necesario implementar nuevas estrategias para mejorar los resultados maternos a largo plazo e incorporar otras medidas preventivas iniciadas aún antes de la concepción, de manera que se logre disminuir aún más las tasas de complicaciones graves y la muerte materna.
Palabras clave: Enfermedad Cardiovascular; Hemorragia Obstétrica; Preeclampsia; Morbilidad Materna Severa; Morbilidad Materna Extrema; Mortalidad Materna.
Introduction
Recent evidence suggests that maternal health has been progressively worsening worldwide leading to increasing rates of major maternal morbidity and mortality(1-5). There are multiple risk factors associated with the rise of serious maternal morbidity including pregnancy at advanced age, obesity, primiparity, ethnicity, women with pre-existent conditions such as diabetes, chronic hypertension, cardiovascular disease, prior cesarean delivery, and multiple gestation(6). For instance, the trend to postpone pregnancy in high income countries comes along with a higher rate of pre-existent disease resulting in higher risks for complications(7). In Canada, for example, the rate of major maternal morbidity was 24.3 per 1 000 births in women with pre-existent disease compared with only 4.3 per 1 000 births in those without a pre-existent condition(8). The increasing rate of obesity in several countries, especially in the United States (US), is associated with increased rates of pre-existent diseases and maternal complications such as preeclampsia, gestational diabetes, and venous thromboembolism, as well as primary cesarean delivery(7,9-11).
Maternal morbidity has become an obstetric quality indicator mainly because of the extremely low maternal mortality ratio in high income countries(7,12). In the Netherlands, obstetric hemorrhage was the most frequent cause of major maternal morbidity in a recent nationwide survey, but only led to maternal mortality in exceptional cases(6). Overall, major maternal morbidity occurs in 0.5% to 1.0% of all births in high income countries and that rate is expected to increase in the coming years(7). In the US, it is estimated that 50 000 cases of serious maternal morbidity occur annually(3) and the conditions responsible for most adverse maternal outcomes include hemorrhage, venous thromboembolism, hypertensive diseases of pregnancy, sepsis, and cardiovascular causes(13-14). The rate of it in this country increased by 75% and during postpartum hospitalizations by 114% in the period of 2008-2009 compared with 1998-1999(14,15). Particularly, there were growing rates of blood transfusion, acute renal failure, acute myocardial infarction, respiratory distress syndrome, aneurysms, and cardiac surgery(14,15). The burden of severe maternal disease translates into higher health care costs, longer hospitalization, and extended post-hospitalization rehabilitation(3).
The measurement of maternal morbidity remains challenging in populations with low access to obstetric care because of lack of consensus with the definition and the unknown incidence of it at the population level. It has been recently proposed to use the term of ‘absolutely life-threatening’ to define severe maternal morbidity in these regions based on the principle that women experiencing organ failure or need life-saving surgery either make it to the hospital and survive or do not reach the hospital and die(16). Although promising, this approach needs further testing in populations with different levels of care, disease epidemiology, and care access.
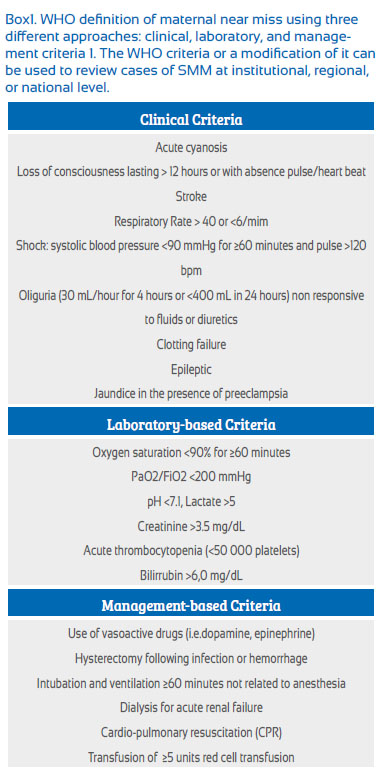
Maternal MorbIdIty - Definitions
One of the most difficult issues in this topic is the lack of a consensus in the definition of maternal morbidity. Severe maternal morbidity or ‘maternal near miss’ refers to a life threatening obstetrical complication that nearly dies but survives and occurs during pregnancy or within 42 days after termination of the pregnancy(1,17). The World Health Organization (WHO) working group on maternal mortality and morbidity recommends to use the term ‘maternal near miss’(1) because this concept describes better the series of events leading from good health to a life-threatening complication associated with organ dysfunction or failure. The criteria used by the WHO are illustrated in Box1. The WHO definition has a high prediction of ‘true’ severe morbidity with a reported sensitivity and specificity of 100% and 92%, respectively(18).
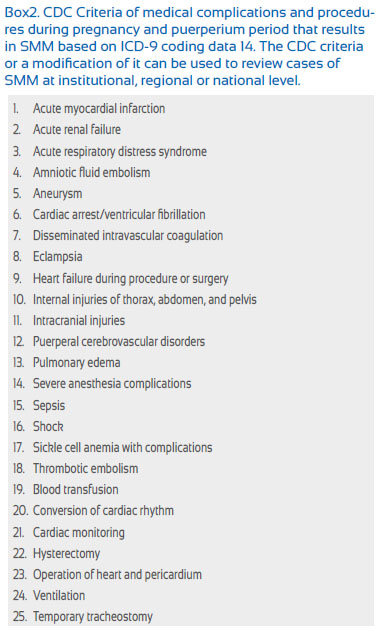
The Centers for Disease Control and Prevention (CDC) in the US uses the term ‘severe maternal mortality’ (SMM) based on the International Classification of Diseases – 9 (ICD-9) codes of twenty-five clinical complications and procedures associated with a high maternal mortality risk (Box2)(14). The CDC ICD-9 criteria use administrative data alone and among the morbidity indicators, blood transfusion has been the commonest in this country since 1998. In the 2-year period of 2010-2011, disseminated intravascular coagulopathy (DIC) was the second most frequent SMM indicator (32 per 10 000 delivery hospitalization) whereas heart failure during a procedure or surgery was the third occurring in 18 per 10 000 delivery hospitalization(5,14). The performance of the CDC criteria reported in a recent study showed a sensitivity and positive predictive value (PPV) of 77% and 44%, respectively(2). Adding prolonged postpartum hospital staying to the CDC definition, the sensitivity improves to 86%, but the PPV is reduced to 38%. Experts in the US recommend using the CDC ICD-9 criteria at regional and state level(19,20), but they propose to use maternal intensive care unit (ICU) admission and transfusion of ≥ 4 units of blood as indicators of SMM for multidisciplinary review at the institutional level(20). This practical approach has shown to have a high performance when it is used individually (specificity and sensitivity of 63% and 86%, respectively), but the performance increases significantly if both indicators are combined(19,21).
Although there are multiple definitions of severe maternal morbidity reported in the literature including the above-described CDC and WHO criteria, it is recognized that each institution needs to adopt the definition that better fits to its own health care system and ideally the criteria should undergo internal validation. The term SMM will be used in the following sections of this article for practical reasons.
Review process of SMM
Comprehensive review of SMM cases facilities implementation of quality programs that should be measured by consistent data tracking(18-21). To optimize prospective surveillance efforts on severe complications, each hospital should list of potentially life-threatening conditions. A difference of life-threatening conditions identified at hospital admission or in the first (3-6) hours, those that occur during longer hospitalizations reflect better the quality of intra-hospital care. Each hospital should have an assessment obstetrical care process to address any identified weakness or failure within the system through an established committee (i.e. obstetric quality committee) or periodic audits (20).
The review process should be carried out by an institutional multidisciplinary SMM committee that reflects the professional make-up of clinicians and staff who provide or support maternity care such as obstetricians, midwifes, residents, fellows, anesthesia personnel, members of the hospital quality improvement team and administration(20). The Committee reviews all cases of SMM according with the standardized institutional criteria. For each case of SMM, a debriefing with involved care providers is recommended, ideally proximate to the SMM. Information obtained from the debriefing can be retained for the standardized review process. The review process can be performed by partner institutions or individually. Data abstraction should follow a standardized process that assures a comprehensive review(20). An example of the SMM Abstraction and Assessment form is available online: www.safehealthcareforeverywoman. org. Each review should draw a conclusion of whether there were opportunities to improve the outcome. If identified, these opportunities are enumerated, and specific recommendations for potential alterations in the outcome should be suggested to the appropriate responsible institutional person or department(20).
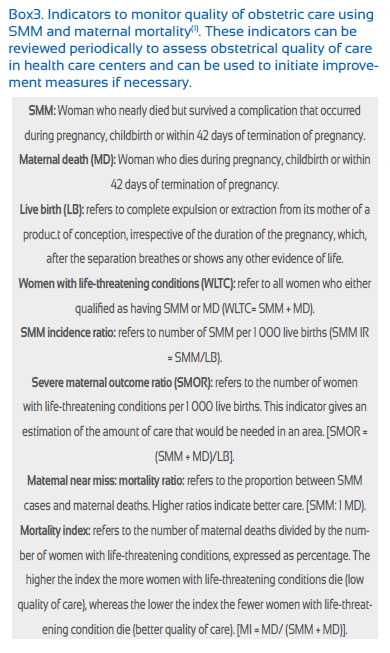
In addition, a number of indicators can be calculated from the collection of data to assess the quality of obstetrical care (Box3)(1). For example, reduction in mortality index calculated as the number of maternal deaths divided by the number of women with life-threatening conditions would indicate improvement in the quality of emergency care. The indicators listed in Box3 have been used to assess quality of obstetrical care in several studies. A large multicenter cross sectional study performed in 27 referral hospitals in Brazil evaluated the clinical performance of these institutions by determining the standardized mortality ratio (SMR = the ratio between observed mortality in the population and expected mortality by mortality prediction based on severity of the case expressed by maternal severity index (MSI)). The higher the SMR score the lower quality of care was noted(22). Those institutions with high SMR scores were found to have deficient obstetrical care services, which were driven by difficult access to health care, absence of blood products, difficult communication between the health services, and delays in patient’s care(22). Advantages of assessing SMM using indicators listed in Box3 include: 1) allows an analysis of the emergency obstetric emergency programs; 2) failures of the health care system are identifiable; and 3) the indicators can be compared with other institutions and countries and changes overtime. In another study conducted in Argentina and Uruguay, a group of investigators found that there were deficiencies in the health care provided in 42% of 26 maternal mortality cases and 80 cases of SMM(23).
Maternal warning systems
To prevent cases of SMM and mortality, several investigators have proposed the implementation of clinical tools that can alert care providers about abnormal physiological parameters preceding serious illness(15,24-26). The primary goal of these early warning systems is to identify patients who can become critically ill and perform early interventions to improve outcomes. The essential characteristics the system should have are: 1) easy to use; 2) has the ability to identify relevant clinical markers of patient deterioration; and 3) guides management that ultimately can reduce maternal morbidity and mortality(15,24-26).
The modified early obstetric warning system (MEOWS) was created in Great Britain, a system that uses a combination of physiologic and neurologic parameters to identify in-patient obstetric patients who require urgent evaluation by a care provider(24). This system seeks to identify patients with complications such as hypertensive disorders, hemorrhage, thromboembolism, sepsis, cardiovascular disease, and cerebrovascular events that account for more than 50% of all maternal deaths and SMM(24). Based on this system, the National Council of Patient safety in the US recently proposed the use of the maternal early warning criteria (MEWC)(24). As in MEOWS, any abnormal parameter listed in MEWC requires the prompt evaluation at the bedside by the provider. It is recommended that each facility that uses MEWC or other maternal warning systems creates a process or protocol (i.e. chain of command protocol) delineating the responsibilities of the personal responding to the immediate assessment request(15,25).
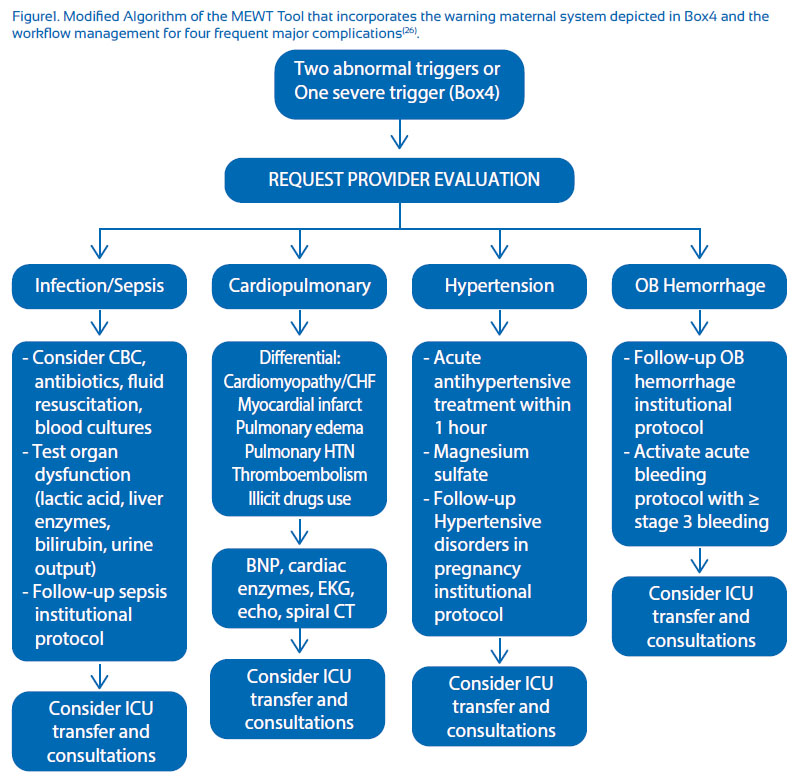
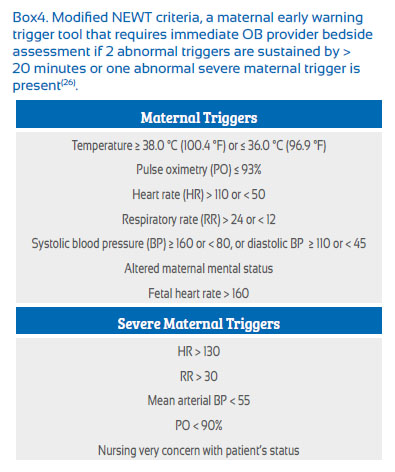
Recently, a group of investigators in the US proposed another clinical tool named the Maternal Early Warning Trigger (MEWT) addressing four common etiologies of maternal morbidity: sepsis, cardiovascular dysfunction, severe preeclampsia-hypertension, and severe hemorrhage accompanied by their respective assessment and clinical guidelines(26). The system is activated in two levels. In most settings, the system is activated with 2 non-severe abnormal parameters sustained for > 20 minutes or one severe parameter (Box4). A modified flow diagram of the MEWT system parameters with the corresponding activation criteria and maternal management pathways is illustrated in Figure1. A pilot study of the MEWT system implemented in 6 hospitals with a delivery volume between 860-3000 in US demonstrated a significant reduction in both: SMM based on the CDC criteria (-18.4%, P=.01) and composite maternal morbidity defined as SMM CDC criteria with the addition of hemorrhage (>500 mL after vaginal delivery or >1 000 mL after cesarean delivery), dilatation and curettage, and ICU admission (-13.6%, P=.01)(26). The authors also made the following remarks: 1) the alarm frequency of the system was relatively low; 2) there was a good prediction about which patients required ICU admission; and 3) the system was tested in hospital with large variation of delivery volume suggesting the high probability of successful implementation in a large variety of health care centers(26).
Although, the results of this study are promising, further research is needed to confirm the effectiveness of early warning parameters connected to the corresponding management guidelines in reducing preventable maternal morbidity and mortality at regional and national levels. It is likely that hospitals will require modifying warning parameters, response protocols, and clinical guidelines according to physician staffing, nurse’s experience, bed capacity, consultation services, critical care availability, and other factors. In summary, available data support the implementation of maternal warning systems carefully designed in accordance to individual hospital settings. Those systems should be accompanied by optimal response strategies and evidence-based clinical guidelines that support the clinician in the management of critically ill patients.
Consequences of sMM
Unfortunately, the risks of SMM go far beyond the acute time period when the complication occurs. A study showed that women who experienced severe obstetric complications were at significant risk to die after hospital discharge compared with those who have uncomplicated pregnancies and deliveries(27). In addition, wom en exposed to a SMM event are at significant risk of depression, anxiety, and suicidal thoughts(28,29). Redshaw et al.(30) have found that women who experience SMM have feeling of disempowerment for several months after the complication and that is associated with lack of communication or miscommunication during the emergency situation. These long-term consequences are added to personal financial distress that many of these women experience secondary to the elevated costs related to the emergency obstetrical care. Debriefing sessions involving the mother and her partner should take a few weeks after of the acute event occurs allowing the couple to have a better understanding of how difficult was that experience and mitigating any perception of guilt, fear, and powerlessness(27-30). Further research is needed to better understand how to address the needs of women with severe obstetrical complications not only in the acute period, but also in the long-term.
Summary
The incidence of ‘severe maternal morbidity’ or ‘near maternal miss’ as defined by the CDC and the WHO, respectively is increasing in low, medium, and high income countries. Maternal factors, lack of rapid response and resources to appropriately manage obstetrical emergen cies, deficient training to obstetrical health care providers, and absence of comprehensive clinical guidelines to manage maternal complications are the main contributors to preventable major maternal morbidity and mortality. It has been recently demonstrated that periodic multidisciplinary review or audit of SMM cases is an effective approach to assess and improve obstetric quality of care. Furthermore, the use of maternal warning clinical systems, as those described in this article, accompanied by evidence-based clinical management guidelines reduces maternal morbidity significantly. Existing evidence supports validation and implementation of these clinical tools in hospitals providing obstetrical services. However, much more work needs to be done on this relevant public health issue. Future investigation should be focused in unifying definitions and national and international levels, and assessing innovative strategies and interventions that can decrease further the rates of major maternal complications affecting the pregnant population worldwide as well as the long-term sequela that theses complications cause to the mother and her baby.
References
1. Say L, Souza JP, Pattinson RC; WHO working group on maternal mortality and morbidity classifications. Maternal near miss—towards a standard tool for monitoring quality of maternal health care. Best Pract Res Clin Obstet Gynaecol. 2009;23(3):287-96. doi: 10.1016/j.bpobgyn.2009.01.007. [ Links ]
2. Main EK, Abreo A, McNulty J, Gilbert W, McNally C, Poeltler D, et al. Measuring severe maternal morbidity: validation of potential measures. Am J Obstet Gynecol. 2016;214(5):643. e1-643.e10. doi: 10.1016/j.ajog.2015.11.004. [ Links ]
3. Callaghan WM, Creanga AA, Kuklina EV. Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstet Gynecol. 2012;120(5):1029-36. doi: http://10.1097/AOG.0b013e31826d60c5. [ Links ]
4. Martin JA, Hamilton BE, Ventura SJ, Osterman MJ, Mathews TJ. Births: final data for 2011. Natl Vital Stat Rep. 2013 Jun 28;62(1):1-69,72. [ Links ]
5. Agency for Healthcare Research and Quality. Overview of the National (Nationwide) Inpatient Sample (NIS). Available from http://www.hcup-us.ahrq.gov/nisovreview.jsp [ Links ]
6. Zwart JJ, Richters JM, Ory F, de Vries JI, Bloemenkamp KW, van Roosmalen J. Severe maternal morbidity during pregnancy, delivery and puerperium in the Netherlands: a nationwide population-based study of 371,000 pregnancies. BJOG. 2008 Jun;115(7):842-50. doi: 10.1111/j.1471-0528.2008.01713.x. [ Links ]
7. van Roosmalen J, Zwart J. Severe acute maternal morbidity in high-income countries. Best Pract Res Clin Obstet Gynaecol. 2009;23(3):297-304. doi: 10.1016/j.bpobgyn.2009.01.004. [ Links ]
8. Wen SW, Huang L, Liston R, et al; ; Maternal Health Study Group, Canadian Perinatal Surveillance System.. Severe maternal morbidity in Canada, 1991-2001. CMAJ. 2005;173(7):759-64. [ Links ]
9. Cerdegren MI. Maternal morbid obesity and the risk of adverse pregnancy outcome. Obstet Gynecol. 2004;103(2):219-24. [ Links ]
10. O’Brien TE, Ray JG, Chan WS. Maternal body mass index and the risk of preeclampsia: a systematic overview. Epidemiology. 2003;14(3):368-74.
11. Campbell KH, Savitz D, Werner EF, Pettker CM, Goffman D, Chazotte C, Lipkind HS. Maternal morbidity and risk of death at delivery hospitalization. Obstet Gynecol. 2013;122(3):627- 33. doi: 10.1097/AOG.0b013e3182a06f4e. [ Links ]
12. Hill K, Thomas K, AbouZahr C, Walker N, Say L, Inoue M, Suzuki E; Maternal Mortality Working Group. Estimates of maternal mortality worldwide 1990 and 2005: an assessment of available data. Lancet. 2007;370(9595):1311-9. [ Links ]
13. Berg CJ, Callaghan WM, Henderson Z, Syverson C. Pregnancy- related mortality in the United States, 1998 to 2005. Obstet Gynecol. 2011;117(5):1230. [ Links ]
14. Centers for Disease Control and Prevention. Severe maternal morbidity in the United States. Available from http://www. cdc.gov/reproductivehealth/maternalinfanthealth/severematernalmorbidity. htlm. [ Links ]
15. Friedman AM. Maternal early warning systems. Obstet Gynecol Clin North Am. 2015;42(2):289-98. doi: 10.1016/j. ogc.2015.01.006. [ Links ]
16. Ronsmans C, Scott S, Adisasmita A, Deviany P, Nandiaty F. Estimation of population-based incidence of pregnancy-related illness and mortality (PRIAM) in two districts in West Java, Indonesia. BJOG. 2009;116(1):82-90. doi: 10.1111/j.1471- 0528.2008.01913.x. [ Links ]
17. Geller SE, Rosenberg D, Cox SM, Kilpatrick S. Defining a conceptual framework for near-miss maternal morbidity. J Am Med Womens Assoc. 2002;57(3):135-9. [ Links ]
18. Souza JP, Cecatti JG, Haddad SM, Parpinelli MA, Costa ML, Katz L, Say L; Brazilian Network for Surveillance of Severe Maternal Morbidity Group; Brazilian Network for Surveillance of Severe Maternal Morbidity. The WHO maternal nearmiss approach and the maternal severity index model (MSI): tools for assessing the management of severe maternal morbidity. PloS One. 2012;7(8):e44129. doi: 10.1371/journal. pone.0044129. [ Links ]
19. Geller SE, Rosenberg D, Cox SM, Brown M, Simonson L, Kilpatrick S. A scoring system identified near-miss maternal morbidity during pregnancy. J Clin Epidemiol. 2004;57(7):716-20. [ Links ]
20. Kilpatrick SJ, Berg C, Bernstein P, Bingham D, Delgado A, Callaghan WM, et al. Standardized severe maternal morbidity review: rationale and process. Obstet Gynecol. 2014;124(2 Pt 1):361-6. doi: 10.1097/AOG.0000000000000397. [ Links ]
21. You WB, Chandrasekaran S, Sullivan J, Grobman W. Validation of a scoring system to identify women with near-miss maternal morbidity. Am J Perinatol. 2013;30(1):21-4. doi: 10.1055/s-0032-1321493. [ Links ]
22. Haddad SM, Cecatti JG, Souza JP, Sousa MH, Parpinelli MA, Costa ML, et al. Applying the maternal miss approach for the evaluation of quality of obstetric care: a worked example from a multicenter surveillance study. Biomed Res Int. 2014;2014:989815. doi: 10.1155/2014/989815. [ Links ]
23. Karolinski A, Mazzoni A, Belizan JM, M, Althabe F, Bergel E, Buekens P. Lost opportunities for effective management of obstetric conditions to reduce maternal mortality and severe morbidity in Argentina and Uruguay. Int J Gynaecol Obstet. 2010;110(2):175-80. doi: 10.1016/j.ijgo.2010.05.002. [ Links ]
24. Singh S, McGlennan A, England A, Simons R. A validation study of the CEMACH recommended modified early warning system (MEOWS). Anesthesia. 2012;67(1):12-8. doi: 10.1111/j.1365-2044.2011.06896.x. [ Links ]
25. Mhyre JM, D’Oria R, Hameed AB, Lappen JR, Holley SL, Hunter SK, Jones RL, King JC, D’Alton ME. The maternal early warning criteria: a proposal from the national partnership for maternal safety. J Obstet Gynecol Neonatal Nurs. 2014;(6):771-9. doi: 10.1111/1552-6909.12504.
26. Shields LE, Wiesner S, Klein C, Pelletreau B, Hedriana HL. Use of maternal early warning trigger tool reduces maternal morbidity. Am J Obstet Gynecol. 2016;214(4):527.e1-6. doi: 10.1016/j.ajog.2016.01.154. [ Links ]
27. Filippi V, Alihonou E, Mukantaganda S, Graham WJ, Ronsmans C. Near misses: maternal morbidity and mortality. Lancet. 1998;251(9096):145-6. [ Links ]
28. Borg Curen N, McNeill J, Murray K. A systematic review of midwife-led interventions to address post partum post-traumatic stress. Midwifery. 2014;30(2):170-84. doi: 10.1016/j. midw.2013.09.003. [ Links ]
29. Meaney S, Lutomski JE, O’Connor L, O’ Donoghue K, Greene RA. Women’s experience of maternal morbidity: a qualitative analysis. BMC Pregnancy Childbirth. 2016; 16(1):184. doi: 10.1186/s12884-016-0974-0.
30. Redshaw M, Hockley C. Institutional processes and individual responses: women’s experiences of care in relation to cesarean birth. Birth. 2010;37(2):150-9. doi: 10.1111/j.1523536X.2010.00395.x.
I do not declare any conflict of interest
Recieved: September 10, 2016 Accepted: September 29, 2016
Correspondence: Julio Mateus, MD, PhD Medical University of South Carolina 96 Jonathan Lucas St MSC 619, Suite 634 Charleston, South Carolina, United States