Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.62 no.4 Lima oct. 2016
SIMPOSIO EMERGENCIAS Y COMPLICACIONES SEVERAS OBSTÉTRICAS
Maternal mortality
Mortalidad materna
Rebecca Wineland, MD1
1 Clinical Instructor, Maternal Fetal Medicine Fellow, Division of Obstetrics and Gynecology, Medical University of South Carolina
Abstract
The maternal mortality ratio (MMR) for each population is an indicator of medical and surgical quality control. The World Health Organization has committed to decreasing maternal mortality worldwide. Access to care remains an important facet of improving overall health of populations. Quality control and excellent communications among health care providers is equally important. Standardization of obstetric emergency protocols will further decrease maternal mortality.
Keywords: Maternal Mortality; Health Service Utilization; Postpartum Hemorrhage; Obstetric Emergency; Evidence-based Medicine; Quality Improvement
Resumen
La razón de mortalidad materna (RMM) representa un control de calidad médico y quirúrgico para cada población. La Organización Mundial de la Salud se ha propuesto disminuir la mortalidad maternal en el mundo. El acceso al cuidado médico sigue siendo una faceta importante para mejorar la salud poblacional. Es igualmente importante el control de la calidad y la excelente comunicación entre los profesionales de la salud. La estandarización de los protocolos de emergencia obstétrica permitirá una mayor disminución de la mortalidad materna.
Palabras clave: Mortalidad Materna; Servicios de Salud, Utilización; Hemorragia Posparto; Emergencia Obstétrica; Medicina Basada en la Evidencia; Mejoría de la Calidad.
Introduction
The maternal mortality ratio (MMR) is the annual number of maternal deaths per 100 000 pregnant women. The MMR for each population is an indicator of the quality of antepartum, intrapartum, and postpartum care. The inclusion and exclusion criteria for MMR varies significantly among international organizations. The Centers for Disease Control (CDC) and the American College of Obstetricians and Gynecologists (ACOG) have updated their definition of MMR to include any duration or location of the pregnancy(1). This new definition includes all pregnancy related mortality up to 365 days after miscarriage, termination, ectopic, intrauterine demise, or viable birth 1. The inclusion of maternal deaths up to 1 year after pregnancy reflects the increase in underlying chronic morbidities in resource-rich countries. The World Health Organization (WHO), an agency of the United Nations, differs from the CDC and ACOG definition of MMR because it limits the timing of death after pregnancy to 42 days(2).
Although decreasing in number worldwide, maternal death is still a risk during pregnancy and childbirth. Globally, approximately 303 000 women die each year due to pregnancy related complications(3). It is thought that approximately 50% of these maternal deaths are avoidable(2). With the advent of medications such as uterotonics, safe transfusion of blood products, and access to trained medical providers, the global MMR has been decreasing. At the Millennium Summit of the United Nations, one of the target goals included a commitment to improve maternal health with the aim to decrease the MMR by 75% by 2015(3). To achieve this end, monetary resources were used to increase the births attended by skilled practitioners, increase access to contraception (particularly for adolescents), and increase prenatal care visits. Meeting again in 2015 in New York, the United Nations reviewed the data and healthcare progress since 1990. Due to the work of in ternational health organizations, particularly the WHO, the worldwide MMR has dropped 45% from 1990 to 2015(4). Although not at the target goal of a 75% reduction, it is a change in the right direction.
The WHO reported that 157 of 183 countries had decreases in their MMR between 2000-2013(5). Unlike the majority of countries worldwide, the United States noted a 26.6% increase in MMR from 2000-2014(6). Racial disparities continue to increase the risk for a pregnancy-related death in the United States and non-Hispanic black women are at the highest risk(7) . This increase in the MMR in the United States is attributed to the higher number of women with maternal age >35, chronic cardiovascular disease, and at risk for violence/trauma(8).
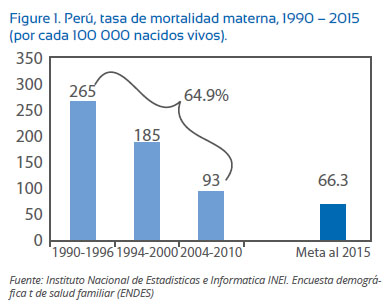
Public health resources are the best predictor of a country’s MMR. Access to care, recognition of a medical emergency, and adequate and appropriate treatment are the most important parameters leading to this ratio(9). In the South Sudan, where more than 50% of the population lives in poverty and medical care is scarce, the MMR was 789 in 2015. However, this rate is markedly improved from a prior MMR of 1703 in 1990(4). In 2015, the MMR in Peru was 66 which is a significant drop of 65% compared with the rate of 265 in 1990 (Figure 1).
National civil registration and vital statistic data (CRVS) records all births and causes of death within a country. In some populations, a portion of maternal deaths is unreported or misclassi fied which adversely affects the quality of data reporting. In countries where CRVS systems may not be accurate, the WHO uses alternative methods of data collecting to adjust the reported rate. The MMR in countries with scant birth and death records is not as reliable given this amount of uncertainty. Peru created an updated CRVS system in 2000 and has since produced higher quality data reporting(4).
Causes of maternal morbidity
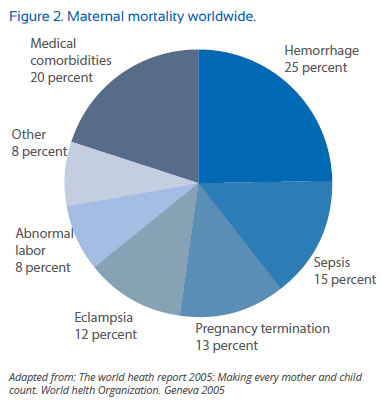
Hemorrhage, sepsis, and eclampsia are the most common causes of preventable maternal death in both resource-rich and resource-poor countries (Figure 2)(11). Postpartum hemorrhage remains the leading cause of maternal death globally with approximately 140 000 deaths annually(12).
In resource-rich countries such as the United States and Europe, cardiovascular events leading to maternal deaths are increasing in incidence, especially within the first year after childbirth. Cardiovascular events include stroke due to hypertension, cardiomyopathy, ruptured aneurysm, myocardial infarction, and pulmonary embolus. The MMR for cardiovascular events in the United States and the United Kingdom has increased in frequency over the past twenty years(7,13). This is attributed to increased maternal obesity, advanced maternal age, use of assisted reproductive technology, and increased incidence of type II diabetes and hypertension.
Improving maternal outcomes
In an effort to reduce maternal mortality in the United States, the National Partnership for Maternal Safety (NPMS) was established in 2012(14). This collaborative group focuses on systematic change through evidence-based medicine to prevent maternal deaths. This systems-based approach addresses each medical topic (i.e. obstetrical hemorrhage, severe hypertension, prevention of venous thromboembolism) in relation to the 4 R’s: readiness of the medical unit, recognition of high risk patients, standardized team response to the emergency, and reporting with a post-event debrief to assess for systems issues(14).
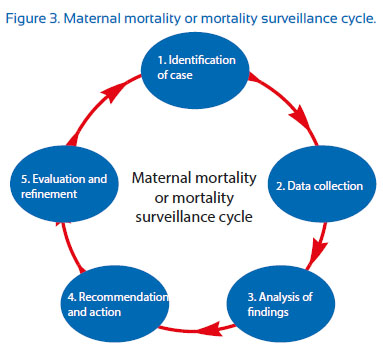
Quality improvement in maternity hospitals and outpatient clinics is imperative to decrease the MMR. Quality improvement is a formal analysis with a focus on decreasing healthcare morbidity and mortality. Each medical facility should organize a case review of every maternal death in order to identify ways in which clinical care should be improved. In addition to deaths, all cases of maternal morbidity, or ‘near misses’, should be evaluated with a root cause analysis to assess the need for policy change. A root cause analysis is used to examine adverse events to assess how they can be avoided in the future. This thorough review of a patient’s clinical presentation, hospital course, and medical interventions is an invaluable educational tool that will reduce adverse outcomes. The WHO has urged health organizations and providers to closely monitor maternal mortality in a regimented fashion (Figure 3)(15).
The non-profit organization in the United States that accredits health care organizations, The Joint Commission, found that the most common cause for a sentinel event on the labor and delivery floor was poor communication. Barriers to effective communication were cited as hierarchy and lack of training(16). The SBAR (Situation-Background-Assessment-Recommendation) technique was developed in the United States Navy and now provides a framework of communication between medical providers(17):
- Situation: "What is going on with the patient?"
- Background: "What is the clinical background?"
- Assessment: "What do I think the problem is?"
- Recommendation: "What would I do it correct it?"
Enhancing communication between all providers is paramount and should be practiced regularly with roll playing scenarios. Evidence based standardization in the form of a protocol for high risk maternal complications such as hemorrhage and severe hypertension will also improve patient safety. Obstetrical emergency guidelines should be formulated by a committee and be easily accessible to the physician, nursing, and administrative teams. A beneficial eclampsia protocol may include IM and IV magnesium dosages, second line anticonvulsants, vital sign parameters, and lab evaluation.
Recognition of patients at risk for serious pregnancy complications will allow the medical team to be on high alert. In Latin America, the risk of pregnancy related death is highest for women under 15 years old(18). Populations at high risk for maternal mortality need sexual health education and access to reliable forms of contraception.
Similar to airline pilot training, medical simulation in a controlled setting has demonstrated to strengthen skillsets, knowledge, and communication. For example, having an obstetrical hemorrhage protocol and then practicing it as a training drill in a team approach will markedly increase patient safety. Team simulation training facilitates communication and identifies common roadblocks to optimal patient care.
In areas where access to health care providers is poor and simulation of obstetric emergencies is not feasible, basic education of abnormal vital signs and clinical symptoms (i.e. severe headache, hypertension, right upper quadrant pain) will assist with recognizing the need for transport and a higher level of care. In resource poor countries, basic education of community providers leads to early diagnosis of high risk conditions. After 2 weeks of basic ultrasound training, midwives in Nepal were able to correctly identify malpresentation, multiple gestation, fetal viability and placenta previa with a portable ultrasound during home prenatal visits(19). With a goal of at least four prenatal visits as well as 1-2 postpartum visits, there are increased opportunities to recognize the warning signs of preeclampsia, diabetes, infection, and thromboembolism(3). With targeted interventions, education, and in-creases in health care resources, we can aim for a further reduction in the global MMR.
Summary
A paradigm shift over the past 30 years has decreased maternal mortality worldwide. Education, increase in the number of skilled providers, evidence based clinical protocols, and access to care has lowered the MMR. Not all maternal deaths are preventable. However, as healthcare providers, we are responsible for facilitating quality improvement in our hospitals, educating our communities of obstetrical warning signs, and leading simulation drills. Practicing a framework for communication, such as SBAR, will have a profound impact on patient care(20). Implementing evidence based medical protocols improves confidence in decision making for both entry level and highly skilled practitioners(21). It is also imperative to be willing to acknowledge and identify the system based failures in our healthcare systems. As a team, problem solving and analysis of our most difficult cases will prevent recurrence of a similar adverse outcome.
References
1. Berg C, Daniel I, Atrash H. Strategies to reduce pregnancy-related deaths. Atlanta: Centers for Disease Control. 2001. Available at: www.amchp.org. Accessed August 2016. [ Links ]
2. Hoyert DL. Maternal mortality and related concepts. Vital Health Stat. 2007;3:1-13. [ Links ]
3. United Nations Development Program. The Millennium Development Goals Report 2000. Available at: www.undp.org. Assessed August 2016. [ Links ]
4. World Health Organization. Trends in maternal mortality: 1990 to 2015. Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva (Switzerland): World Health Organization; 2015. [ Links ]
5. World Health Organization. Trends in maternal mortality: 1990 to 2013. Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva (Switzerland): World Health Organization; May 2014. [ Links ]
6. MacDorman M, Declercq E, Cabral H. Recent increases in the U.S. maternal mortality rate. Obstet Gynecol. 128:447-55. doi: 10.1097/AOG.0000000000001556. [ Links ]
7. Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Pregnancy-related mortality in the United States; 2006- 2010. Obstet Gynecol. 2015 Jan;125(1):5-12. doi: 10.1097/ AOG.0000000000000564. [ Links ]
8. Koch AR, Rosenberg D, Geller S. Higher risk of homicide among pregnant and postpartum women aged 10-29 year in Illinois, 2002-2011. Obstet Gynecol. 2016;128:440-6. doi: 10.1097/AOG.0000000000001559. [ Links ]
9. Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Social Science and Medicine. 1994;38:1091-110. doi: 10.1016/0277-9536(94)90226-7. [ Links ]
10. Instituto Nacional de Estadística e Informática - INEI. Encuesta Demográfica y de Salud Familiar (ENDES). 2015. Available at: http://dhsprogram. com/pubs/pdf/FR284/FR284.pdf. Accessed August 2016. [ Links ]
11. World Heath Organization. Making every mother and child count. The World Health Report. Geneva. 2005. Available at: www.who.int/whr/2005/en. Accessed July 2016. [ Links ]
12. World Health Organization. WHO recommendations for the prevention and treatment of postpartum hemorrhage. Geneva: WHO. 2012. Available at: apps.who.int/iris/bitstre am/10665/75411/1/9789241548502. Accessed July 2016. [ Links ]
13. Berg CJ, Callaghan WM, Syverson C, Henderson Z. Pregnancy- related mortality in the United States, 1998 to 2005. Obstet Gynecol. 2010 Dec;116(6):1302−9. doi: 10.1097/AOG. 0b013e3181fdfb11. [ Links ]
14. D’Alton ME, Main EK, Menard MK. The National Partnership for Maternal Safety. Obstet Gynecol. 2014;123:973-7. doi: 10.1097/AOG.0000000000000219. [ Links ]
15. World Health Organization: Beyond the numbers: reviewing maternal deaths and complications to make pregnancy safer. Geneva: WHO. 2004. [ Links ]
16. Joint Commission on Accreditation of Healthcare Organizations. Sentinel event alert #30: preventing infant death during delivery. https://www.jointcommission. org/sentinel_event_alert_issue_30_preventing_infant_ death_and_injury_during_delivery. Accessed August 2016. [ Links ]
17. Heinrichs WM, Bauman E, Dev P. SBAR flattens the hierarchy among caregivers. Studies in health technology and informatics. 2011 Dec;173:175-82. [ Links ]
18. Conde-Agudelo A, Belizan JM, Lammers C. Maternal-perinatal morbidity and mortality associated with adolescent pregnancy in Latin American: Cross-sectional study. Am J Obstet Gynecol. 2004;192:342-9. [ Links ]
19. Kozuki N, Mullany L, Khatry S, Ghimire RK, Paudel S, Blakemore K, Bird C, Tielsch JM, LeClerq SC, Katz J. Accuracy of home-based ultrasonographic diagnosis of obstetrical risk factors by primary-level health care workers in rural Nepal. Obstet Gynecol. 2016. Sep;128(3):604-12. doi: 10.1097/ AOG.0000000000001558. [ Links ]
20. Risser D, Rice M. The potential for improved teamwork to reduce medical errors in the Emergency Department. Annals of Emergency Medicine. 1999;34:373-83. http://dx.doi. org/10.1016/S0196-0644(99)70134-4. [ Links ]
21. Rosenberg W, Donald A. Evidence based medicine: an approach to clinical problem solving. BMJ. 1995 Apr 29;310:1122-6. http://dx.doi.org/10.1136/ bmj.310.6987.1122. [ Links ]
Disclosure: No conflicts of interest
Recieved: September 10, 2016 Accepted: September 30, 2016
Correspondence Address: Rebecca Wineland, MD Department of Obstetrics and Gynecology 96 Jonathan Lucas Street Suite 634 Charleston, SC 29425