Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.65 no.3 Lima jul./dic 2019
http://dx.doi.org/10.31403/rpgo.v66i2186
COMUNICACIÓN CORTA
Effectiveness of the FIGO protocol for medical management of first-trimester abortion
Eficacia del esquema FIGO para el manejo médico del aborto en el primer trimestre
Cintia María Sepúlveda Rivera1,a, Osvaldo Miranda Araujo1,a, Jessica Aideé Mora Galván1,a, Arturo Maximiliano Ruiz Beltrán2,b, Diego Arturo González Vásquez1,a, Jefsi Argelia León Domínguez1,a
1 Instituto Nacional de Perinatología, Mexico City, Mexico
2 Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico City, Mexico
a Department of Obstetrics
b Department of Internal Medicine
ABSTRACT
Objective: To determine the effectiveness of misoprostol using the International Federation of Gynecology and Obstetrics (FIGO) 2017 protocol for medical management of first trimester abortion. Methods: A cross-sectional study was performed between March and September 2018. Seventy-six patients diagnosed with first trimester spontaneous abortion were managed following the FIGO 2017 protocol for medical management of first trimester abortion. Results: Main indications for inclusion of the 76 patients were missed abortion 57.9%, incomplete abortion 25%, and anembryonic pregnancy 17.1%. Medical induction with misoprostol followed the FIGO 2017 protocol for medical management of first trimester abortion. The most frequent side effect reported was abnormal uterine bleeding associated with pelvic pain (72.3% of patients). Complete uterine evacuation was accomplished in 98.6% of the patients. Conclusion: Misoprostol use in patients with first trimester abortion following the FIGO 2017 protocol was a safe and cost-effective therapeutic option.
Key words: Abortion, spontaneous, Management, medical, Efficacy.
RESUMEN
Objetivo. Evaluar la eficacia del manejo con misoprostol al emplear el esquema de la Federación Internacional de Ginecología y Obstetricia (FIGO) 2017 para el abordaje de abortos de primer trimestre. Métodos. Estudio transversal realizado entre marzo y septiembre 2018, que incluyó 76 pacientes con diagnóstico de aborto espontáneo en el primer trimestre de gestación y que tuvieron manejo de acuerdo al esquema recomendado por FIGO 2017. Resultados. Las principales indicaciones para la inclusión de las 76 pacientes fueron aborto diferido 57,9%, aborto incompleto 25% y embarazo anembrionado 17,1%. La inducción con misoprostol siguió las indicaciones de FIGO 2017 para el manejo del aborto del primer trimestre. El efecto adverso más frecuente fue el sangrado vaginal asociado a dolor pélvico en 72,3% de las pacientes. Se logró la evacuación uterina completa en 98,6% de los casos. Conclusión. El manejo médico del aborto del primer trimestre de gestación con el uso del misoprostol de acuerdo al esquema FIGO 2017 ofreció una opción terapéutica altamente segura y costo-efectiva.
Palabras clave. Aborto espontáneo, Tratamiento médico, Eficacia.
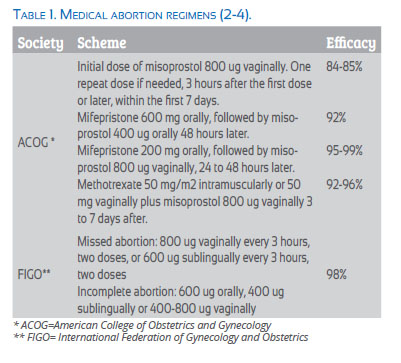
Spontaneous abortion occurs in 20% of all pregnancies. Therapeutic options include expectant, medical and surgical management. Medical induction is used in nearly 30% of patients with no signs of infection, hemorrhage, severe anemia or coagulation disorders. The most frequently used drugs are mifepristone, misoprostol and methotrexate(1). There are different regimens recommended in the literature, as shown in Table 1(2-4).
Methods
This cross-sectional study included all patients with first trimester spontaneous abortion attended at the Emergency Department of the Instituto Nacional de Perinatología in Mexico City, from March through September 2018. Transvaginal ultrasound was performed to confirm early pregnancy loss, and the FIGO protocol for misoprostol was used(4). A follow-up ultrasound evaluation was scheduled 7 days after treatment and earlier if warning signs appeared. In case a gestational sac was still present, a second dose of the protocol was indicated. Medical management was considered successful when no gestational sac was found. The institutional review board of the Instituto Nacional de Perinatología approved the study.
Results
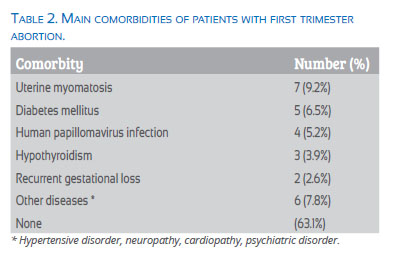
A total of 76 patients with diagnosis of first trimester abortion were included. Of these, 44 (57.9%) were diagnosed with missed abortion, 19 (25%) had complete abortion, and 13 (17.1%) an anembryonic pregnancy. The patients’ average age was 28 years, and the average gestational age was 7.9 weeks. Main comorbidities found were uterine myomatosis, diabetes mellitus, human papillomavirus, hypothyroidism, and recurrent pregnancy loss (Table 2).
The most frequent clinical manifestations were light vaginal bleeding and pelvic pain in 55 patients (72.3%). Ten patients (13.1%) were asymptomatic; nine (11.8%) had only vaginal bleeding, and two (2.6%), mild pelvic pain.
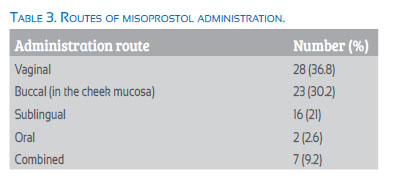
All patients were treated with the FIGO 2017 protocol, and administration routes of misoprostol varied according to physician’s preference (Table 3).
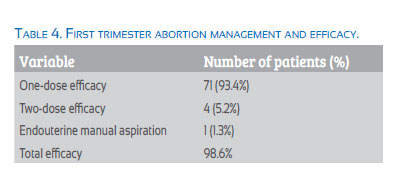
The efficacy of one misoprostol dose was 93.4% and that of 2 doses, 5.2%. Only one patient did not respond to treatment and presented vaginal hemorrhage and hypovolemic shock; she underwent surgical management. Overall efficacy was 98.6%.
Discussion
The FIGO scheme was proposed in 2017 for medical management of early pregnancy loss and reported an efficacy of 98%(4), similar to the value we obtained at the Instituto Nacional de Perinatología. In 2018, Khurshid et al. evaluated this scheme, reporting an efficacy of 41.8%. It is possible that they obtained this low result because ultrasonographic control was performed within 12 hours after the misoprostol administration, while most evaluations take place a week or two after the procedure(5).
In 2012, two reviews by the Cochrane Library and the Society of Obstetricians and Gynaecologists of Canada aimed to evaluate the need of antibiotic prophylaxis. These reviews did not find any randomized trial of the medical management of abortion nor the antibiotic prophylaxis; only surgical managements were considered(6). The last update of the American College of Obstetricians and Gynecologists, in November 2018, stated that antibiotic prophylaxis is not indicated in this group of patients(7). In accordance with these recommendations, our patients did not receive antibiotic prophylaxis before the medical management.
In 2011, Grossman et al.(3) determined alternatives to ultrasound in the follow-up of this condition. They concluded that the combination of either urine pregnancy test or human chorionic gonadotropin, and the clinical history and medical ability to determine the expulsion of the gestational sac, detected 90-99% of completed abortions as compared with transvaginal 2D ultrasound. Therefore, this would be appropriate in centers without ultrasound equipment(5). At our center, all patients received weekly ultrasound follow-up until absence of gestational sac was confirmed. In case of unsuccessful result, the misoprostol regimen was indicated for a second time.
Finally, the American College of Obstetricians and Gynecologists recommends that ultrasound follow-up is enough; when not available, human chorionic gonadotropin determination is acceptable.
ACOG also recommends prophylaxis with at least 50 micrograms anti-D immunoglobulin in candidate patients. To determine reproductive prognosis, patients should be evaluated after two losses(7).
A limitation of our study is the restricted number of patients. A prospective study with a larger sample will yield better results. We observed that creating documents for the institutional care of patients with this condition is an important area of opportunity. These include an informed consent form and a follow-up form, as well as handouts explaining possible side effects and therapeutic options for patients to solve the problem at home, warning signs for patients to go to an emergency room, and a questionnaire evaluating patient satisfaction with the medical management of abortion.
In conclusion, the FIGO protocol for the medical management of first trimester abortion with misoprostol resulted in a safe and effective strategy. This regimen also offers a lower-cost therapeutic option by not including mifepristone.
Conflict of interest: The authors report no conflict of interest.
Financing: The authors received no financial support for this article
Previous publication of the article: None.
Cite: Sepúlveda Rivera CM, Miranda Araujo O, Mora Galván JA, Ruiz Beltrán AM, González Vázquez DA, León Domínguez JA. EffectivenessoftheFIGOprotocolformedical management of first trimester abortion. Rev Peru Ginecol Obstet. 2019;65(3):305-307. DOI: https://doi.org/10.31403/rpgo.v66i2186
References
1. Soon JA, Costescu D, Guilbert E. Medications used in evidence-based regimens for medical abortion: An overview. J Obstet Gynaecol Can. 2016 Jul;38(7):636-45. doi: 10.1016/j.jogc.2016.04.005. [ Links ]
2. Prager S, Dalton VK, Allen RH; Committee on Practice Bulletins-Gynecology. Practice Bulletin Number 150, May 2015. Early pregnancy loss. https://www.acog.org/-/media/Practice-Bulletins/Committee-on-Practice-Bulletins----Gynecology/Public/pb150.pdf. [ Links ]
3. Creinin MD, Grossman DA; Committee on Practice Bulletins-Gynecology and the Society of Family Planning. Practice Bulletin Number 143, March 2014. https://www. acog.org/-/media/Practice-Bulletins/Committee-on-Practice-Bulletins----Gynecology/Public/pb143.pdf?dmc=1. [ Links ]
4. Morris JL, Winikoff B, Dabash R, Weeks A, Faundes A, et al. FIGO’s updated recommendations for misoprostol used alone in gynecology and obstetrics. Int J Gynaecol Obstet. 2017 Sep;138(3):363-366. doi: 10.1002/ijgo.12181.
5. Khurshid N, Awan AS, Akhtar N, Riaz M. Efficacy of misoprostol for miscarriages using FIGO Protocol: Initial experience at Fauji Foundation Hospital. J Soc Obstet Gynaecol Pak. 2018;8(2):76-80. http://jsogp.net/new/index.php/jsogp/article/view/147. [ Links ]
6. Van Eyk N, van Schalkwyk J, INFECTIOUS DISEASES COMMITTEE. Antibiotic prophylaxis in gynaecologic procedures. J Obstet Gynaecol Canada. 2012 Apr;34(4):382–91. doi: 10.1016/S1701-2163(16)35222-7. [ Links ]
7. Prager S, Dalton VK, Allen RH; ACOG Committee on Practice Bulletins-Gynecology. Early pregnancy loss. Committee on Practice Bulletins-Gynecology Number 2000. https://www.acog.org/-/media/Practice-Bulletins/Committee-on-Practice-Bulletins----Gynecology/Public/pb200.pdf?dmc=1&ts=20181026T2344588485. [ Links ]
Correspondence:
Cintia María Sepúlveda Rivera, MD
Departamento de ginecología y obstetricia del Instituto Nacional de Perinatología, Ciudad de México, México Calle Montes Urales 800, Lomas Virreyes, Lomas de Chapultepec IV Secc, 11000 Ciudad de México, CDMX
+52 (64) 49 979908
Received: 7 March 2019
Accepted: 12 May 2019
Published online: 22 July 2019