Introduction
Preterm delivery (PD) is an obstetric problem and an important cause of perinatal morbimortality1. Threatened preterm delivery is often treated with tocolytics to delay delivery and to improve perinatal outcomes2. Various studies have shown that this treatment is associated with pregnancy prolongation, but not with reducing perinatal complications3,4.
A meta-analysis showed that the incidence of imminent preterm delivery (during the following seven days) varies from 2% to 29%5) and that the ability to forecast it is limited. One of the challenges in the management of threatened preterm delivery is identifying the at-risk group of pregnant women. If we could recognize this group in a precise manner, interventions like hospitalization, tocolysis and corticosteroid administration could be used more efficiently.
There are prediction models that consider demographic and clinical factors at the time of evaluation6-8. The combination of cervical length (CL), maternal characteristics and obstetric history has proven to be useful for predicting9. However, these models lack enough sensitivity to be implemented. Furthermore, access to biochemical markers is not always possible10. Therefore, there is a need for strategies to identify the group at high risk of imminent preterm delivery.
A uterine artery Doppler study is efficient to detect conditions related to placental insufficiency. There is evidence that the altered remodeling of uteroplacental arteries might be associated to preterm delivery11,12. An increase in the uterine artery pulsatility index (IP-AUt) during the second pregnancy trimester has been associated with a higher risk for preterm delivery(13,14). Similarly, there is an increase in the intraplacental vascular impedance associated to PD in in vitro pregnancies15. However, two studies did not confirm this association16,17. Consequently, it is unknown if measuring the IP-AUt could contribute to predicting imminent PD.
The objective of this study was to establish the prognostic utility of cervical length and the uterine artery pulsatility index for imminent preterm delivery in symptomatic patients.
Methods
This was a case-control study performed at the Central Hospital "Dr. Urquinaona", Maracaibo, Venezuela, from June 2014 to March 2018. We evaluated women with single pregnancies with a gestational age between 24 and 35 weeks who had been diagnosed with threatened preterm delivery, presenting up to three uterine contractions in 30 minutes, a cervical dilatation of up to 3 cm and a cervix effaced to 80% or less, with intact membranes. The study was approved by the ethical review boards of the Medical Faculty of the University of Zulia and of the hospital. Written informed consent was obtained from each participant upon selection.
We excluded patients with the following conditions: multiple pregnancies, history of use of progesterone or any other tocolytic during the present pregnancy, cervical insufficiency diagnosis or history of cervical cerclage, premature membrane rupture or amniotic fluid alterations, uterine anomalies, abnormal placentation, history of maternal cardiac pathologies, active inflammatory or infectious disease, hypertension and pre-gestational or gestational diabetes, intrauterine growth restriction, congenital fetal anomalies, acute chorioamnionitis and unknown gestational age. We also excluded from the study the patients who declined to participate.
In the hour following admission, and before starting any treatment, the participants underwent speculoscopy, and the fern and Nitrazine tests to rule out membrane rupture. Immediately after this, we performed a digital exam to evaluate cervical dilatation, consistency and position, followed by a fetal ultrasound evaluation to determine the placental insertion site, fetal head and abdominal circumferences, femur length and amniotic fluid index. Fetal cardiac frequency and uterine contractions were monitored by external tocodynamometry.
The evaluation of cervical length by transvaginal ultrasound was performed with the Voluson® V730 Expert (GE Healthcare, USA). Patients were placed in dorsal lithotomy position with an empty bladder, and the 7,5 MHz transducer was positioned in the anterior vaginal fornix. Measurements were made orienting the transducer to show the external and internal cervical os in the same sagittal plane, with both labia, posterior and anterior, of equal width. After the image was amplified, cervical length was measured as a straight line between the electronic markers, identified by the cervical canal’s sonolucency. If the endocervical canal was too curved, we measured two portions and added them up. We obtained three images and used the one that showed the shortest length.
We obtained the transabdominal measurement of the IP-AUt with a 7,5 MHz transducer, at the optimal setting for Doppler gain. Iliac and uterine arteries were identified by visualizing the color Doppler flow, establishing the flow waveforms and velocimetry of both uterine arteries with an insonation angle below 25° 16. After identification, we used pulsed wave Doppler with a sampling window of 2 mm to show the vessel, with an insonation angle below 30°, one centimeter distal to the crossing point and a maximum systolic velocity of 30 to 50 cm/second for selective identification. When we obtained three similar consecutive waveforms with a diastolic notch, we measured the IP-AUt, calculating the average of both uterine arteries. For the cases with lateral placenta, we chose the ipsilateral IP-AUt value to represent the uteroplacental circulation better. In cases with central placenta, we picked the lowest index for representation(18).
Participants were indicated rest in left lateral decubitus position and hydration with 500 mL of Ringer solution. If we observed cervical changes or if contractions persisted two hours after treatment, the patients were hospitalized and started tocolytic therapy with nifedipine. During hospitalization, we administered intramuscular betamethasone to induce fetal lung maturity. Tocolytics were suspended 48 hours after the first corticosteroids dose. We did not use tocolytics nor corticosteroids in pregnancies past week 34.
The main study variable was the frequency of imminent delivery (within seven days after evaluation). All data were stored for subsequent analysis and were not available during hospitalization.
Data are presented as absolute and relative values. Qualitative variables were analyzed using the chisquare test. Quantitative variables with a normal distribution were compared with Student’s t-test.
Variables with a non-normal distribution were compared with the Wilcoxon-Rank test. We used a Receiver Operating Characteristic curve to determine the best cut-off point and evaluate the diagnostic precision of cervical length, IP-AUt and the combination of both for predicting imminent preterm delivery. We used Hanley and McNeil’s methodology to compare the difference in the tests’ areas under the curve. We also calculated the prognostic parameters with a 95% confidence interval. The statistical significance level was p < 0,05. All analyses were performed with the statistical package SPSS® version 22.0 (SPSS Inc, USA).
Results
For the study, we selected 518 patients, of which we excluded 21 because they had premature membrane rupture, five because of preeclampsia and one because of uterine anomalies diagnosed during follow-up. Ten patients were excluded due to incomplete data. For the final analysis, we selected 481 pregnant women, of which 119 (24.8%) delivered prematurely in the seven days following the evaluation (group A) and 362 patients (75.2%) who gave birth after seven days (group B).
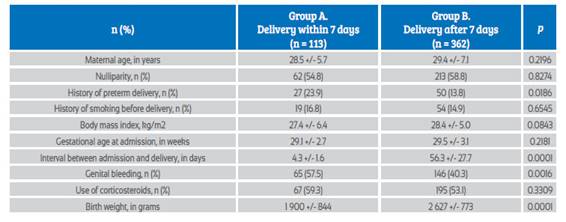
The groups’ characteristics are shown in Table 1. The frequency of history of preterm delivery and genital bleeding were significantly higher in the patients in group A compared to the patients in group B (p < 0.05). The interval between evaluation and delivery was 4.3 +/1.6 days in group A and 56.3 +/27.2 days in group B (p < 0.0001). We did not find significant differences in the rest of general characteristics (p = ns).
The average value of cervical length in group A was 18.4 +/5.9 mm, and it was 34.3 +/5.6 mm in group B (Figure 1). Meanwhile, the IP-AUt values were 2.24 +/0.51 and 1.57 +/0.36 for the patients in groups A and B, respectively (Figure 2). These differences were significant (p < 0.0001).
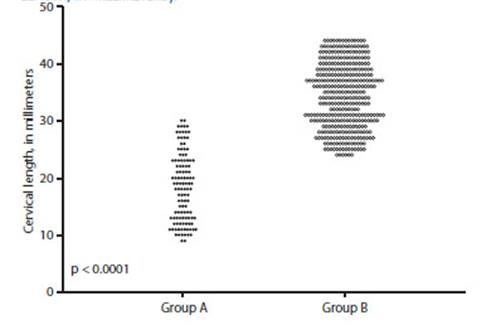
Figure 1 Cervical length values obtained by ultrasound in each of the groups (X axis: Group A, Group B; Y axis: cervical length, in millimeters).
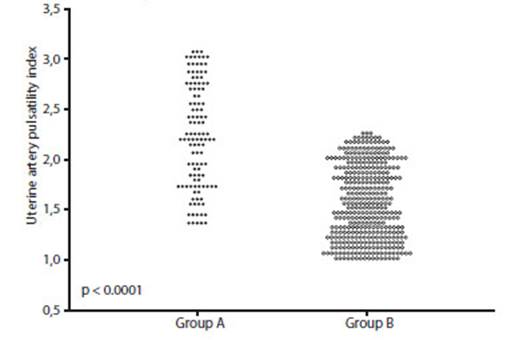
Figure 2 Values of the uterine artery pulsatility index in each of the groups (X axis: Group A, Group B; Y axis: uterine artery pulsatility index).
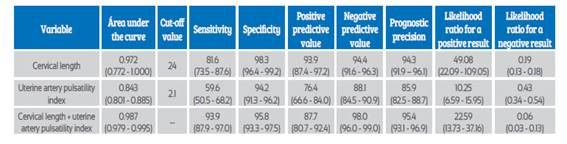
In Figure 3, we show the receiver operating characteristic curve for cervical length, IP-AUt and the combination of both measurements. Cervical length (CL) presented an area under the curve of 0.972 (95% confidence interval (CI) 0.772 to 1.000), while the area under the curve of IP-AUt was 0.843 (95% CI 0.801 to 0.885). The difference between both was considered significant (p < 0.001). Nevertheless, the combination of measurements with the formula X = (9.982671 + ((3.464345 * IP-AUt) (0.661065 * CL)) had a significantly superior value (0.987; 95% CI 0.979 a 0.995) compared with IP-AUt and cervical length (p < 0,0001) individually. The rest of predictive values for imminent preterm delivery are shown in Table 2.
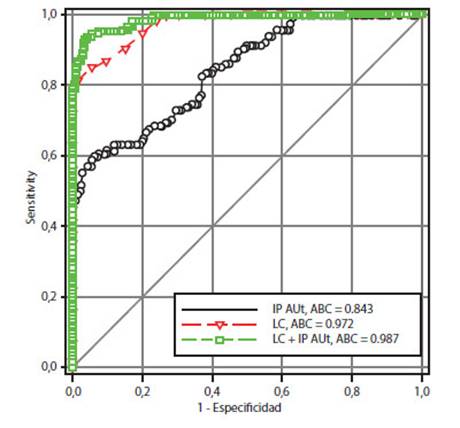
Figure 3 Receiver operating characteristic curve for cervical length, uterine artery pulsatility index and their combination, for predicting imminent preterm delivery (X axis: “1 - specificity”; Y axis: sensitivity).
Discussion
Our results show that cervical length is superior to IP-AUt for predicting imminent preterm delivery. Nevertheless, the combination of both measurements presents significant differences and a superior discriminating capacity, compared with the individual measurements. This suggests that they can be useful for predicting imminent preterm delivery, contributing to a timely treatment for this high-risk group.
Preterm delivery is a global health problem. Research in useful prediction models may reduce health care costs and perinatal complications. Cervical length is a sensitive and simple method to predict the risk for PD19. While a short CL is associated with a higher risk for PD, its application potential to identify which pregnant women with uterine contractions will present imminent preterm delivery is limited20.
The cut-off value for CL that predicts imminent PD in our study was 24 mm. Previous studies have evaluated its utility in patients with threatened PD. The first showed that patients with PD had on average a shorter CL compared with those who delivered at term21. Another study in symptomatic patients receiving tocolytic treatment found that this was successful in patients with an average CL of 27 mm22. It has also been observed that over half of patients with deliveries in the following 28 days have a CL below 20 mm, while only 7% of those who give birth after 28 days present such values23. Finally, another study showed that a CL under 20 mm presented in over two thirds of the cases with preterm delivery, but only in 21% of the patients who delivered at term24. Nevertheless, CL is not always associated to PD, and it is not useful for distinguishing between high and low-risk groups. This is supported by the lack of correlation between CL and time of delivery, even after adjusting for confounding factors25.
The possible relationship between placental insufficiency and PD is endorsed by studies that show less remodeling of uteroplacental arteries in samples obtained from women who delivered prematurely(12). It has been also described that IP-AUt is highest in patients who deliver before week 3314. These findings support our present results, where patients with imminent PD presented higher IP-AUt values. However, a previous study did not find differences between patients who delivered prematurely and at term16.
Our study’s findings suggest that IP-AUt increases the predictive performance of CL, so it can be used alone or combined with CL to aid in the prediction of imminent PD in symptomatic patients with intact membranes. These measurements detect different components of PD, so the IPAUt would allow to identify high-risk groups that present minimal changes in CL18,23.
Olgan et al.18) performed the only previous study that evaluated the combination of CL and IP-AUt for predicting PD. Their research showed that both individual measurements were useful for predicting imminent PD (area under the curve of 0.83 for CL and 0.72 for IP-AUt). Findings suggest that both measurements combined help to identify the group of patients at a higher risk for PD, regardless of whether they have received tocolytics or not. In this study, the area under the curve of CL increased when combined with IP-AUt, improving its prediction capacity for imminent PD. This improvement in its discriminating capacity might be because women with PD conform a heterogeneous group regarding underlying pathogenic mechanisms and the combination may facilitate their identification.
The advantage of this evaluation is that it obtains non-invasive measurements with fast, objective and quantitative results that are easy to interpret. However, in cases of placental insufficiency, the IP-AUt might be elevated since the increase in intrauterine pressure may affect the uterine blood flow13,18.
This study has several strengths. Participants were followed until delivery. The treating physicians did not know the results of the ultrasound and Doppler evaluations, which limited possible biases.
On the other hand, some selected patients had an imminent PD, which could have also decreased the possibility of errors in the analysis. The study also has weaknesses, such as a lack of inter-observer variability analysis in the measurements. This research took place in a single center with a homogeneous population, which may hinder the generalization of our results.
In conclusion, the combined use of CL and IP-AUt is useful for predicting imminent preterm delivery in symptomatic patients. The combination of both tests increases the discriminating capacity, compared with both measurements individually.