Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.66 no.2 Lima abr-jun 2020
http://dx.doi.org/10.31403/rpgo.v66i2245
Original Articles
Maternal and perinatal characteristics of pregnant women with COVID-19 in a national hospital in Lima, Peru
1Department of Gynecology and Obstetrics, Edgardo Rebagliati Martins National Hospital, Social Health Insurance System - EsSalud,Lima, Peru
Introduction
: The pandemic of coronavirus disease 2019 (COVID-19) has spread to more than 100 countries. Specific information about its behavior in pregnancy is still limited. Objective: To describe the maternal and perinatal characteristics of pregnant patients infected with COVID-19 and their newborns in a tertiary referral hospital.
Methods
: Descriptive study. Subjects were all pregnant patients admitted to the OB/ GYN Emergency Department of the Edgardo Rebagliati Martins National Hospital from March 24 to May 7, 2020, who were diagnosed with SARS-CoV-2 infection by rapid test or by RT-PCR test. Medical and hospital records were reviewed to retrieve sociodemographic data, patient’s history, clinical manifestations, maternal serology, obstetric complications, delivery mode and perinatal aspects.
Results
: 41 patients diagnosed with SARS-CoV-2 were identified. 9.2% of all admissions had a positive rapid test. The most common symptoms were cough in 84.6%, fever in 76.9% and sore throat in 61.5%. 68.2% of the patients were asymptomatic, 19.5% had mild illness and 7.3 %, moderate. 2 cases progressed to severe pneumonia requiring non-invasive ventilation. No maternal deaths were recorded. 21.7% were vaginal deliveries, while 78.3% were C-sections. One baby born in a vaginal delivery had a positive PCR result on day 8.
Conclusions
: A large percentage of asymptomatic pregnant patients had a positive PCR test. Implementing universal screening among patients in labor as part of the pregnant patient flow protocol is necessary for all institutions.
Key words: Cesarean delivery; COVID-19; Neonatal outcome; SARS-CoV-2; Vaginal delivery
Introduction
By the end of 2019, a rise in pneumonia cases in Wuhan, province of Hubei, China, was recorded1. Epidemiological surveillance detected a common exposition to a wholesale market in the city of Wuhan, where live animals were sold. Transmission and spread of this pneumonia, which caused up to 7 severe cases, was attributed to a new virus of the Coronaviridae family called SARS-CoV-2, and the disease it causes has been named, by international consensus, COVID-19. Spread during the following months was fast, reaching all inhabited continents soon. On March 11, 2020, the World Health Organization declared the outbreak by the new coronavirus a pandemic, after it spread to over 100 countries worldwide.
In Peru, the index case (or first case) of COVID-19, reported on March 6, 2020, was a Peruvian male who had travelled to Spain, France and the Czech Republic. The virus spread to 8 first-generation confirmed cases (direct contacts), 2 second-generation cases (contacts of a confirmed first-generation case) and 2 third-generation cases (contacts of a confirmed second-generation case). Our country has the second highest infection rate in South America, with estimations of 58 526 laboratory-confirmed cases and 1 627 deaths (2.8% lethality) at the time we submitted this paper2. Currently, our country has regions with high rates of infection and mortality. Lima, with the highest infection rate, is considered a vulnerable or red area due to its large percentage of laboratory-confirmed cases. 35 299 cases and a substantial burden of disease have been reported in the eastern, northern and southern parts of Lima ("conos"), with a positive test rate of 14.9%, which shows a high level of contagion2. The seriousness of the situation caused the Peruvian government to declare a country-wide health emergency by supreme decree.
According to current evidence, the incubation period is 5 days (range 2 to 14 days). The disease affects mainly people over 30 years old, especially patients with comorbidities such as obesity and hypertension3. While new data on COVID-19 continue to help us daily increase our understanding of the disease, specific information about pregnancy is still limited. In previous pandemics like SARS and H1N1 influenza, pregnant women were more susceptible to develop more severe cases and had higher mortality rates than the general population4. The clinical profile of pregnant women with SARS-CoV-2 infection remains unclear, with limited data.
The Peruvian Social Health Insurance System (EsSalud) currently manages 32% of all hospitalized cases in the country. Attending circa 6 100 deliveries per year, the Edgardo Rebagliati Martins National Hospital is one of the biggest health centers in the country belonging to EsSalud. It is currently one of the main centers for treating COVID-19 at the national level.
We present our experience with pregnant patients diagnosed with COVID-19 by rapid and PCR tests, and their maternal and perinatal characteristics.
Methods
For this study, we selected all pregnant patients hospitalized in the OB/GYN emergency department between March 24 and May 7, 2020 who were diagnosed with SARS-CoV-2 infection by rapid test (Orient Gene COVID-19 IgG/IgM Rapid Diagnostic Test) in maternal blood or by RT-PCR testing of nasopharyngeal swabs after a positive rapid test or in cases with respiratory symptoms, regardless of rapid test status on admission. All pregnant women were evaluated for COVID-19 symptoms (fever, cough, sore throat, dyspnea, headache, muscle pain, diarrhea), upon which they were classified as asymptomatic or with mild, moderate or severe disease, according to the guidelines established in the technical document "Prevention, Diagnosis and Treatment of Persons Infected with COVID-19 in Peru (approved by Ministerial Resolution N° 193-2020 / National Health Ministry MINSA)5. The following maternal variables were considered: age, gestational age, parity, status on admission (pregnant or postpartum), indication for C-section if it was performed, leukocytosis, lymphopenia, platelet count, C-reactive protein, creatinine, liver function tests, imaging findings when appropriate and respiratory and obstetric outcomes. Neonatal variables were delivery mode, sex, weight, Apgar score at birth and RT-PCR results for SARS-CoV-2. The information was entered to a digital data sheet, processed with SPSS v26.0 and presented in tables and figures for further analysis.
Results
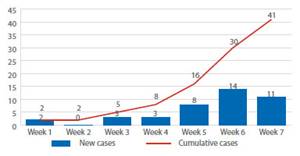
During the study period, 41 hospitalized patients were diagnosed with SARS-CoV-2, of which 37 were pregnant women and 4, postpartum mothers (Figure 1). The first infected pregnant woman was diagnosed on March 24; after this, screening was progressively implemented, starting with patients with respiratory symptoms and those undergoing surgery, until universal screening with rapid test was established for all patients admitted to our hospital on April 14.
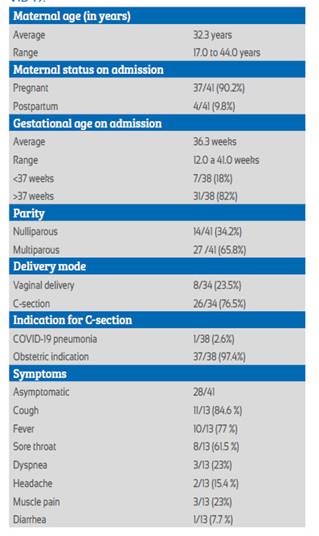
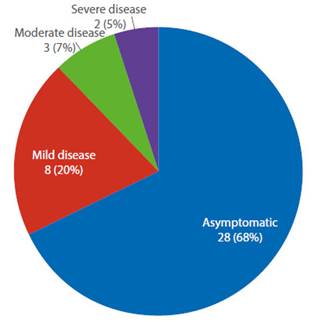
Maternal clinical characteristics are summarized in Table 1. The most common symptoms were cough in 84.6%, fever in 76.9% and sore throat in 61.5%. 20% of cases (8/41) had mild disease, 7.3% (3/41), moderate disease and 2 cases (4.8%, 2/41) had severe pneumonia that required admission to the intensive care unit (ICU) to receive non-invasive ventilation (Figure 2). No maternal deaths were registered. The prematurity rate (under 37 weeks) was 18% (7/38); all cesarean sections were due to an obstetric indication except for one patient 32 weeks pregnant, whoseindication was COVID-19 pneumonia. 2 pregnant patients aged 30 and 34 developed severe pneumonia. The first was 32 weeks pregnant and had consolidation and an infiltrate in the right hemithorax; she was in the ICU for 9 days and underwent a C-section due to the need to optimize maternal ventilation. The second case presented at 31 weeks gestation with bilateral ground-glass opacity and stayed in the ICU for 8 days. Currently, she is still hospitalized in our hospital’s center for COVID-19-infected pregnant patients. Both women had lymphopenia, PCR > 10mg% and mild transaminasemia, and required non-invasive ventilation.
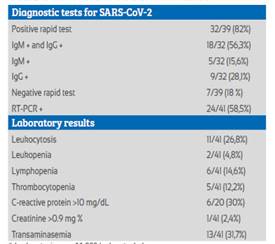
Out of the 41 total patients with SARS-CoV-2, rapid blood tests were carried out in 39 of them, obtaining 32 positive results. Among the 7 patients with a non-reactive blood test, symptoms persisted in 5 of them, 1 had fever during hospitalization and 1 reported having had contact with a case. Because of this, nasopharyngeal swabs were obtained, yielding positive results for SARS-CoV-2 at the RT-PCR test.
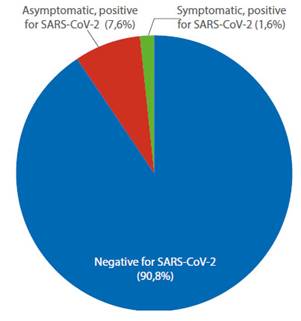
Table 2 shows the characteristics of the maternal laboratory and diagnostic tests. Since universal screening was implemented as a requirement upon admission, 316 rapid tests have been performed by May 7, obtaining 29 (9.2%) reactive and 287 (90.8%) non-reactive results. Among the reactive cases, only 5 (17.2%) presented symptoms on admission, while 24 (82.8%) were asymptomatic (Figure 3).
Delivery was vaginal in 23.5%, the remaining 76.5% underwent a C-section (Table 2). The most frequent cause for surgery was history of 1 to 3 previous C-sections with 48.3%, followed by malposition and malpresentation with 20.7%, hypertensive disorders of pregnancy with 10.3%, and premature membrane rupture with 17.2%. One third of the vaginal deliveries were associated to other obstetric conditions such as previous C-section, preeclampsia and premature membrane rupture.
Regarding neonatal outcomes, the 41 mothers gave birth to 35 newborns either vaginally or by C-section, including one cesarean section due to a twin pregnancy of 34 weeks and severe preeclampsia. 71% of newborns were male, with an average weight of 3 200 g (1 775 to 4 625 g). Of the total, only three had a low Apgar score at minute one and all of them recovered fast after 5 minutes. All the newborns were tested for SARS-CoV-2 with RT-PCR, following our institution’s protocol and, until submission date, only one baby born vaginally tested positive with a swab sample obtained at day 8. His mother had a negative rapid test on admission and, later, a positive PCR result, performed due to mild symptoms in the postpartum, so horizontal transmission is assumed.
Discussion
The clinical characteristics of pregnant women with COVID-19 pneumonia in our study were similar to those of adults with COVID-19 pneumonia, as previously reported by Guan and Wu(6,7). 68.2% (28/41) of pregnant women positive for SARS-CoV-2 did not present any symptoms and most were diagnosed on admission with rapid tests. Only 4.8% (2/41) of the infected pregnant women progressed to a severe pneumonia, which required admission to the ICU; none of them died. According to small case series8,9 with a total of 38 pregnant women diagnosed with COVID-19 during the second and third trimester, the most common symptoms were fever and cough, like in our study; cough was present in 84.6% and fever in 76.9% of cases.
In Peru, according to the dispositions of the Ministry of Health, positive cases are those with a positive result either to the rapid or to the RTPCR test. Implementing rapid blood tests as a screening method particularly enables us to identify asymptomatic patients, whose proportion is similar to that reported in New York10 and double that from London11. This could happen because the socioeconomic characteristics of our population determined the intensity of the community spread in Lima to resemble that of the American city, where no measures of early confinement were adopted.
This is the first study to use rapid blood tests as a screening method, which is a cost-effective strategy to face the pandemic and, particularly, to detect asymptomatic patients12. Benefits consist in the early isolation of the pregnant woman with COVID-19 from her newborn to prevent horizontal transmission, and in the adequate use of the personal protective equipment (PPE) by the health care team during attention, especially in a resource-limited context, such as the current global one13.
Nevertheless, one severe case presented symptoms for two weeks and had two negative rapid tests, despite which she was admitted to the ICU as clinically suspicious. Diagnosis was confirmed with the RT-PCR test. There was also a false negative in an asymptomatic patient who tested positive with RT-PCR some days later, which could explain contagion of her newborn. Clinical judgement must always prevail and one must also consider that both tests have a false negative rate with important maternal-fetal implications14.
Regarding delivery mode, the hospital where the study was performed is a reference center for high risk patients, which could explain the higher rate of C-sections due to an obstetric indication in 96.2% of the cases. This rate is similar to that reported by Mehree15 of 75% (44/58) and to that by Li16 of 87% in confirmed cases. Both studies had controls with high C-section rates, 70% and 47.1%, respectively. Regarding etiology, our research’s findings are similar to those published. Yang reported that the majority of patients (91%) underwent a C-section due to various indications, such as preeclampsia, fetal distress and previous C-section, as well as lack of knowledge regarding the risk of transmission to the newborn17. Recently, a case series of 10 infected pregnant women reported that 5 of them had an emergency C-section due to fetal distress, premature membrane rupture and fetal death, and that their COVID-19 severity was considered mild to moderate, except for one case of severe pneumonia18. Related studies have selection bias, small samples, and varying staging criteria for the infection. Nevertheless, to date, no definitive study about vertical transmission to the newborn has been found; this missing information would suggest the best delivery mode. Obstetric conditions persist as the main indications for C-section.
This study is the first one in our country to describe a high rate of asymptomatic pregnant women with positive PCR after implementing a universal screening program. We believe that these results can be extrapolated to hospitals and centers with realities similar to ours. The potential benefits of a universal testing approach include the possibility of using a positive result to determine practices of hospital isolation and bed allocation, to inform about neonatal management and to guide the use of personal protective equipment. Access to these tests grants an important opportunity to protect mothers, newborns and health care teams during these hard times combatting the pandemic.
REFERENCES
1. Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential domestic and international spread of the 2019nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;395(10225):689-97. doi:10.1016S0140-6736(20)30260-9 [ Links ]
2. Ministerio de Salud. MINSA: @gobpePCM; 2020 [Available from: https://www.gob.pe/minsa.] [ Links ]
3. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). 16-24 February 2020. https://www.who.int/docs/default-source/coronaviruse/who-china-jointmission-on-covid-19-final-report.pdf [ Links ]
4. Wong SF, Chow KM, Leung TN, Ng WF, Ng TK, Shek CC, et al. Pregnancy and perinatal outcomes of women with severe acute respiratory syndrome. Am J Obstet Gynecol. 2004;191(1):292-7. https://doi.org/10.1016/j.ajog.2003.11.019 [ Links ]
5. Resolución Ministerial 084-2020/MINSA que aprueba el documento técnico: Atención y manejo de casos clínicos de COVID-19. Ministerio de Salud. 7 de marzo 2020. [ Links ]
6. Guan WJ, Ni ZY, Hu Y, Liang W-H, Ou C-Q, He J-X, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708-1720. doi:10.1056/NEJMoa2002032 [ Links ]
7. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;10.1001/jama.2020.2648. doi:10.1001/jama.2020.2648 [ Links ]
8. Liu Y, Chen H, Tang K, Guo Y. Clinical manifestations and outcome of SARS-CoV-2 infection during pregnancy. J Infect. 2020; doi:10.1016/j.jinf.2020.02.028 [ Links ]
9. Zhang L, Jiang Y, Wei M, Cheng BH, Zhou XC, Li J, et al. [Analysis of the pregnancy outcomes in pregnant women with COVID-19 in Hubei Province]. Zhonghua Fu Chan Ke Za Zhi 2020 Mar 25;55(3):166-71. doi: 10.3760/cma.j.cn112141-20200218-00111 [ Links ]
10. Sutton D, Fuchs K, D'Alton M, Goffman D. Universal screening for SARS-CoV-2 in women admitted for delivery. N Engl J Med. 2020 Apr 13;NEJMc2009316 doi: 10.1056/NEJMc2009316 [ Links ]
11. Khalil A, Hill R, Ladhani S, Pattisson K. SARS-CoV-2 in pregnancy: symptomatic pregnant women are only the tip of the iceberg. [published online ahead of print, 2020 May 6]. Am J Obstet Gynecol. 2020;S0002-9378(20)30529-9. doi:10.1016/j.ajog.2020.05.005 [ Links ]
12. Vintzileos WS, Muscat J, Hoffmann E. AM. Screening all pregnant women admitted to labor and delivery for the virus responsible for COVID-19. Am J Obstet Gynecol. 2020 Apr 26;S0002-9378(20)30472-5. doi: 10.1016/j.ajog.2020.04.024 [ Links ]
13. Sethuraman N, Jeremiah SS, Ryo A. Interpreting diagnostic tests for SARS-CoV-2. JAMA. 2020 May 6 doi: 10.1001/jama.2020.8259 [ Links ]
14. Kelly JC, Dombrowksi M, O'neil-Callahan M. False-negative COVID-19 testing: Considerations in obstetrical care. Am J Obstet Gynecol MFM. 2020 Apr 28;100130 doi: 10.1016/j.ajogmf.2020.100130 [ Links ]
15. Zaigham, M., Andersson, O. (2020). Maternal and perinatal outcomes with COVID-19: a systematic review of 108 pregnancies. Acta Obstet Gynecol Scand. 2020;10.1111/aogs.13867. doi:10.1111/aogs.13867 [ Links ]
16. Li N, Han L, Peng M, Lv Y, Ouyang Y, Liu K, Yue L, et al. Maternal and neonatal outcomes of pregnant women with COVID-19 pneumonia: a case-control study. Clin Infect Dis. 2020 Mar 30;ciaa352. doi: 10.1093/cid/ciaa352. [ Links ]
17. Yang Z, Wang M, Zhu Z, Liu Y. Coronavirus disease 2019 (COVID-19) and pregnancy: a systematic review,. J Matern Fetal Neonatal Med. 2020;1-4 DOI: 10.1080/14767058.2020.1759541 [ Links ]
18. Karami P, Naghavi M, Feyzi A, Aghamohammadi M, Novin MS, Mobaien A, et al. (2020). Mortality of a pregnant patient diagnosed with COVID-19: A case report with clinical, radiological, and histopathological findings. Travel Med Infect Dis. 2020;101665. doi:10.1016/j.tmaid.2020.101665 [ Links ]
5The contents of this article are original and have not been presented previously to any other biomedical journal All the patients provided consent to use their data, which were obtained anonymously for this research
Received: May 11, 2020; Accepted: May 14, 2020











 texto en
texto en