Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.66 no.2 Lima abr-jun 2020
http://dx.doi.org/10.31403/rpgo.v66i2246
Original Articles
Frequency and indications of cesarean delivery in a public teaching hospital in Lima, Peru
1Universidad Peruana Cayetano Heredia, Lima, Perú
2Hospital Nacional Cayetano Heredia, Lima, Perú
Introduction
: Cesarean delivery was an option initially reserved for cases where vaginal delivery could compromise the life of the pregnant woman or the fetus. Due to diverse socioeconomic or cultural causes, cesarean delivery has become more accepted as an elective birth procedure. The WHO has established a marginal cesarean rate of 15% in primary cesarean deliveries, as higher rates do not decrease fetal morbidity and mortality. Worldwide, there have been rates as high as 21% (European countries), and 36% in Peru in 2015.
Objectives
: To determine the frequency of cesarean section and the most frequent indications in a public teaching hospital.
Methods
: Descriptive, retrospective series of case studies of patients who underwent elective or emergency cesarean section between January 2013 and December 2017 at a public teaching hospital in Lima, Peru.
Results
: The frequency of cesarean section was of 50.2%, and the most frequent indications were previous cesarean delivery and cephalopelvic disproportion.
Conclusions
: In the Peruvian public hospital studied, the rate of cesarean section exceeded that recommended by the WHO. The most frequent indication was repeat cesarean section.
Key words: Cesarean section; repeat
Introduction
The cesarean section is a procedure consisting in extraction of the fetus and placenta through an incision in the uterus1. The indications for cesarean section may be maternal, fetal and placental. The most frequent indications are repeat cesarean section, cephalopelvic disproportion and fetal compromise2.
An increase in the frequency of cesarean sections has been observed in the past years. This increase could be associated to economic, social and cultural factors, litigation to healthcare professionals, changes in maternal characteristics (pregnancy in older age) or diverse medical reasons3. In 1985, the World Health Organization (WHO), concluded that the acceptable national rate for primary cesarean deliveries should not exceed 10 to 15%4). The study conducted by Beltrán et al., and published in 2016, analyzed 150 countries and concluded that 1 in 5 women in the world delivers by cesarean section, and the global cesarean rate was 6.7% for the year 1990 and became 19.1% in 2014, with an absolute global increase of 12.4%. If only developing countries were considered, the absolute global increase would comprise 14.6% in 14 years5.
In Peru, a study by Vilma Tapia, et al., in 2013, found a cesarean delivery rate of 25.5% in the year 2000 and of 29.9% in 20106. The INEI (National Institute for Statistics and Information Technology) published a cesarean rate of 45.4% for the year 20177.
The objective of the present study was to know the frequency and indications for cesarean deliveries at a public teaching hospital during a period of five years, with the purpose of planning strategies to reduce it.
Methods
This is a descriptive, series of cases study that included all patients who underwent a cesarean section, either as an emergency or elective procedure, in our public teaching hospital, from January 2013 through December 2017. Patients with incomplete information were excluded.
The information was collected from prenatal clinical records, using the following variables: maternal age, gestational age, prenatal control, level of education, marital status, parity, type and indications for cesarean delivery. The information was organized in tables of frequency, with mean, median and corresponding measures of dispersion for quantitative variables, graphics and tables for posterior statistical analysis of the quantitative continuous variables. The student’s t-test and Kruskal Wallis test were used for parametric distribution in case of non-parametric
data. For the chi-square test for qualitative variables we used the STATA v.14 program.
Ethical approval for this study was obtained from the Ethics Committee of the Universidad Peruana Cayetano Heredia, as well as from the Ethics Committee of the Hospital Nacional Cayetano Heredia.
Results
A total of 21 810 deliveries were registered, 49.8% (n=10 867) were vaginal deliveries and 50.2% (n=10 943) by cesarean section; 76 patients were excluded due to incomplete data. Total living newborns were 21 689, with a cesarean rate of 50.5 per 100 living newborns.
The annual frequency of cesarean sections was 49.4% (n=2 216), for the year 2013, 48.4% (n=2 156) for 2014, 51.3% (n=2 213) for 2015, 52.5% (n=2 157) for 2016, and 49.5% (n=2 201) for 2017.
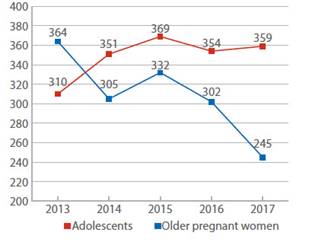
The average maternal age was 26.5 years (range 12 to 53 years); 14.2% of the studied population was under 19 years-old, 16% was over 35, and 69.8% was 20-34 years old (Table 1). Figure 1 shows decrease in frequency of cesarean sections in adolescents whereas it increased in patients over 35 years. In addition, 29% (n=449) of adolescents presented cephalopelvic disproportion (CPD) as the most frequent indication, whereas previous cesarean (28.2%) was the most frequent in mothers older than 35, with statistically significant difference (p=0.01).
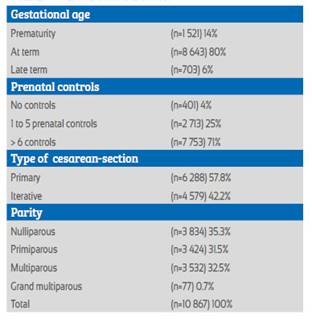
69% of the population reported high school education, 12.8% non-university higher education and 1.1% were analphabets. As of marital status, 71.3% declared living with a partner, 17.6% were single and 10% married (Table 1). 71% had 6 or more prenatal controls and 4% had no prenatal control.
Most cesarean sections were performed at 37-41 weeks of gestation (80%), 14% were preterm and 6% late-term (41 weeks of gestation). 57.8% underwent primary cesarean section, 60.6% of which were nulliparous and 19.2% (n=1 208) multiparous; 42.2% were repeat cesarean sections, 51.7% in multipara (p<0.01) (Table 2). Cesarean section in nulliparous women comprised 35.3% (n=3 834), 31.5% (n=1 207) in primipara, 5% (n=197) in adolescents and 5% (n=197) in advanced age. 66.7% (n=7 293) was hospitalized between 1 and 3 days, 30.4% more than 4-7 days, and 97 patients (0.9%) between 15 and 20 days. The difference was not significant.
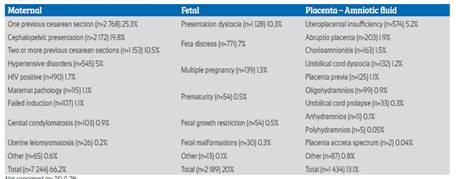
25.3% (n=2 768) of patients had a previous cesarean and 34% (n=940) had previous vaginal delivery, with significant difference (p=0.01). Cephalopelvic disproportion (CPD) was in second place with 19.8% (n=2 172), which included stationary active phase (n=389), small pelvis (n=180), arrest of descent (n=157), fetal macrosomia (n=406), prolonged second phase (n=178) and prolonged latent phase (n=4) of labor.
The patients with history of two or more previous cesareans were in the third place with 10.5% (n=1 153); 86.3% patients had two previous (n=995) and three previous cesarean sections (n=149). Fetal presentation dystocia occurred in 10.3% (n=1 128), of which 98% was divided in 66% for breech presentation (n=744), 25.5% for transverse lie (n=288) and 6.5% for oblique presentation (n=73). 73% of these patients declared more than 6 prenatal controls (p>0.05). In 7% (n=771), the indication for the cesarean section was fetal distress (Table 3).
Throughout the five years of study, the history of a previous cesarean was the most frequent indication, that increased 2% from 2013 to 2015, decreased in 2016 and increased again in 2017 (27%). The second indication was CPD, which exceeded 20% during 2013, 2014 and 2016, was highest in 2014 and lower in 2017 (17.2%).
Fetal dystocia was the third indication in the two first years of the study. However, in the rest of the period the indication was previous cesarean in 12.6% in 2017. The indication for uteroplacental insufficiency decreased from 6% in 2013 to 2.6% in 2017. The indication for fetal distress increased 4% in the years studied.
Table 3 shows that 66.2% of indications were maternal factors, mainly 25.3% due to previous cesarean section, followed by CPD in 19.8%. Fetal indication was fetal dystocia in 10.3% of the population, followed by fetal distress (7%). Both combined (17.3%) represented 86.5% of fetal indications.
Discussion
The frequency of cesareans performed in the hospital largely exceeded the rate recommended by the WHO(4). Our hospital’s rate compares to that of Latin America and the Caribbean, which comprises 40.5% for 2014, thus representing a 19.4% growth compared to the information available for the year 1990 (22.8%)(5). These rates contrast with those of the African continent (7.3%), which are probably caused by deficiency in the healthcare system and lack of resources.
Some of the possible reasons for the increase in the region are: fear of pain, worries about genital modifications after vaginal delivery, the erroneous idea that this procedure is the safest for the baby, a lower tolerance to possible complications or adverse results with the baby, and fear of medical litigation5.
The frequency of cesareans in our hospital has risen, partly because it serves as a reference hospital in the northern part of Lima and a large number of complicated deliveries are attended there. In addition, it is located in the coastal region, where rates are generally higher than in the mountain and rainforest regions6.
In a study conducted by Quispe et al, that analyzed data from 7 hospitals in the period 20012008, the cesarean rate was 36.9% and, compared to our rate, has increased 13.6%8). This difference is larger than the one found by Wynn et al., in the year 2013, who analyzed data from Hospital Arzobispo Loayza and Instituto Nacional Materno Perinatal, where a cesarean rate of 50.2% was recorded9).
The increase in cesarean procedures is multifactorial. On a worldwide scale, women in advanced age are more likely to choose to become pregnant than before, even with higher probability for cesarean section because of age itself10,11 as for maternal and neonatal complications, including obstetrical bleeding, hypertensive disorders, maternal sepsis, reduction in myometrial contractions, increase in maternal and fetal hospitalization in intensive care unit, low Apgar score at 5 minutes, fetal distress12.
This adds up to sociocultural aspects, such as parent anxiety, previous infertility, doctors’ preference and the number of lawsuits for medical negligence that, in Asian countries, for example, increased 58.5% since 199511. In our study on cesarean sections we found 16% of patients with advanced maternal age, which compares with the 15.2% found in a study by Lin CH, et al11.
We found a slight decrease in the number of cesarean procedures in adolescents, similar to data from Hospital Nacional Santa Rosa from Lima, Peru, for the year 2010, in which percentages fell from 44.6% to 38.8% from 2010 to 201213. This differs from the WHO reports that claim there has been an increase in developing countries14.
The percentage of primary cesarean procedures is striking. In a consensus from the American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal Fetal Medicine (SMFM) published in 2014, the rate of primary cesarean section increased from 2002 to 2011 (from 27% to 24%), the major indication causes being arrest of descent, fetal distress and fetal presentation15. In contrast to our study, the frequency of indications varied, CPD as the first cause, including arrest of descent, followed by fetal presentation dystocia and fetal distress15.
The hospitalization time in our patients was similar to that recommended, i.e., 24 hours post-partum when the mother does not present complications, as this period represents the biggest risk for the puerperal woman and the newborns1,16.
In our study, the main indications for cesarean section were previous cesarean and CPD, that compare with findings from the Instituto Nacional Materno Perinatal, in 2016, when the major causes were previous cesarean, abnormal fetal position and CPD17.
At present, the success rate for vaginal delivery after cesarean fluctuates between 60 and 80% 18. Amongst the characteristics described, we found the precedent of having vaginal labor after a cesarean or an adequate Bishop score at the moment of hospitalization19. It is noteworthy that, in our study, 940 patients with history of cesarean were multiparous (p<0.05) and, in case of complying with the necessary characteristics, they would have a high rate of success if submitted to vaginal labor20. In our population, a significant statistical association was found between advanced maternal age and a precedent of cesarean21.
There was an increase in cesareans for abnormal fetal position. This could be due to the higher risk of perinatal morbidity and mortality when giving birth vaginally in case of breech presentation. However, Cochrane suggests decision-taking according to mother’s wishes, obstetrician’s experiences, conditions of safety and other rigorous selection criteria22,23. The ACOG and the Royal College of Obstetricians and Gynecologists recommend the practice of external cephalic version (ECV)24,25). The patient must be evaluated from the 36th week of gestation and offered ECV from week 37 0/724. Patients with this kind of presentation can be identified during prenatal controls, to refer them to specialized institutions in which trained gynecologists-obstetricians can undergo the procedure.
Given the increase in cesarean rates in the last years, several entities have conducted studies about reduction alternatives. The ACOG, in consensus with the Society for Maternal-Fetal Medicine, recommend redefinition of the indications given for arrest of descent, and a reminder that a prolonged latent phase and a prolonged active phase associated to maternofetal well-being do not represent indications for cesarean section15. It is also important to increment the access to non-surgical medical interventions, such as a continuous support during labor, ECV for non-cephalic presentations, instrumental delivery and labor test for twin gestations when the first fetus is in cephalic presentation15). In addition, they emphasize on the importance of high-quality constant audits in all health establishments, truthful recordings of pregnant sociodemographic characteristics, newborn data and main indication for submitting a pregnant woman to cesarean section in uniform terms, in order to know the institutional, national and world realities in an actualized and trustworthy manner26.
There were some limitations in our study, including the information was based in data collected from perinatal clinical charts where some information was illegible or incomplete. The evaluations and indications were conducted by different specialists, which could condition lack of uniformity in indications terminology. The clinical histories are discarded after 5 years, limiting studies over 5 years. The complications associated to surgical interventions were not recorded, limiting the analysis of length of hospitalization. Previous procedures conducted before the indication for cesarean were also not included. The mentioned factors could be reduced through prospective studies.
In conclusion, the frequency of cesarean section in the Hospital Nacional Cayetano Heredia from January 2013 to December 2017 was 50.2%, largely above the recommendation of the WHO. According to the social and epidemiological characteristics, patients were between 20 and 34 years of age, had secondary school education and currently lived with their partners. As to maternal characteristics, term pregnancies and patients with adequate prenatal control were relevant, and the percentages were similar in nulliparous, primiparous and multiparous women. Primary cesarean was more frequent than repeat cesarean section. The most frequent indication was a history of a previous cesarean delivery. Most patients were hospitalized for less than four days.
REFERENCES
1. Cunningham FG, Leveno KJ, Bloom SL, Hauth JC, Rouse DJ, Spong CY. Williams Obstetricia. 23ª edición. McGraw-Hill; 2011. [ Links ]
2. ACOG Practice Bulletin No. 205: Vaginal birth after cesarean delivery. Obstet Gynecol. 2019;133(2):e110-e127. doi:10.1097/AOG.0000000000003078 [ Links ]
3. Ben-Haroush A, Melamed N, Kaplan B, Yogev Y. Predictors of failed operative vaginal delivery: a single-center experience. Am J Obstet Gynecol. 2007;197(3):308.e1-308.e3085. doi:10.1016/j.ajog.2007.06.051 [ Links ]
4. Organización Mundial de la Salud. Declaración de la OMS sobre la tasa de cesáreas. Suiza. HRP; 2015:8 p. [ Links ]
5. Betrán AP, Ye J, Moller AB, Zhang J, Gülmezoglu AM, Torloni MR. The increasing trend in caesarean section rates: global, regional and national estimates: 1990-2014. PLoS One. 2016;11(2):e0148343. Published 2016 Feb 5 doi:10.1371/journal.pone.0148343 [ Links ]
6. Gonzales GF, Tapia VL, Fort AL, Beltran AP. Pregnancy outcomes associated with cesarean deliveries in Peruvian public health facilities. Intern J Womens's Health. 2013;5(18):16878. DOI: 10.2147/IJWH.S46392 [ Links ]
7. Instituto Nacional de Estadística del Perú. Perú Encuesta demográfica y de salud familiar - ENDES 2017, Nacional y Departamental. Perú. 2017:137p. [ Links ]
8. Quispe AM, Santivañez-Pimentel A, Leyton-Valencia I, Pomasunco D. Cesáreas en siete hospitales públicos de Lima: análisis de tendencia en el periodo 2001-2008. Rev peru med exp salud publica. 2010;27(1):45-50. [ Links ]
9. Wynn A, Cabeza J, Adachi K, Needleman J, García PJ, et al. Frequency of maternal and newborn birth outcomes, Lima, Perú, 2013. PLoS One. 2013;10(3):e0116102 DOI: 10.1371/journal.pone.0116102 [ Links ]
10. Herstad L, Klungsoyr K, Skajaerven R, Forsén L, Abyholm T, et al. Elective cesarean section or not? Maternal age and risk of adverse outcomes at term: a population-based registry study of low risk primiparous women. BMC Pregnancy Childbirth. 2016;16:230. DOI: 10.1186/s12884-016-1028-3 [ Links ]
11. Lin HC, Sheen TC, Tang CH, Koa S. Association between maternal age and the likelihood of cesarean section: a population-based multivariate logistic regression analysis. Acta Obstet Gynecol Scand. 2004;83:1178-83. [ Links ]
12. Richards MK, Flanagan MR, Littman AJ, Burke AK, Callegari LS. Primary cesarean section and adverse delivery outcomes among women of very advanced maternal age. J Perinatol. 2016;36(4):272-277. doi:10.1038/jp.2015.204 [ Links ]
13. Albornoz L. Cesáreas en adolescentes atendidas en el Hospital Nacional Santa Rosa durante el periodo 2010 - 2012. [tesis]. Peru. Universidad Nacional Mayor de San Marcos. 2013. [ Links ]
14. Organización Mundial de la Salud. Adolescent pregnancy-issues in adolescent health and development. Ginebra. 2004:92p. [ Links ]
15. The American College of Obstetricians and Gynecologists, Society for Maternal-Fetal Medicine. Obstetric Care Consensus No. 1: Safe prevention of the primary cesarean delivery. Obstet Gynecol. 2014 Mar;123(3):693-711. DOI: 10.1097/01.AOG.0000444441.04111.1d [ Links ]
16. Campbell OM, Cegolon L, Macleod D, Benova L. Length of stay after childbirth in 92 countries and associated factors in 30 lowand middle-income countries: compilation of reported data and a cross-sectional analysis from nationally representative surveys. PLoS Med. 2016 Mar 8;13(3):e1001972. DOI: 10.1371/journal.pmed.1001972 [ Links ]
17. Ayala FD, Rios EG, Rodriguez MA, Ayala R, Quiñones LA, et al. Edad materna avanzada y morbilidad materna. Rev Peru Investig Matern Perinat. 2016;5(2):9-15. [ Links ]
18. Ramos MM, Rolland AS, Feitosa AM. Indicações de cesariana baseadas em evidencias: parte I. Femina. Agosto 2010;38(8). [ Links ]
19. Royal College of Obstetrician & Gynaecologists. Birth after previous caesarean birth (Green-top Guideline No. 45). Reino Unido. October 2015:31p. [ Links ]
20. Metz TD, Stoddard GJ, Henry E, Jackson M, Holmgren C, et al. Simple, validated vaginal birth after cesarean delivery prediction model for use at the of admission. Obstet Gynecol. 2013 Sep;122(3):571-8. DOI: 10.1097/AOG.0b013e31829f8ced [ Links ]
21. Vargas AT, Lévano JA, Lazo MA. Parto vaginal después de una cesárea, aplicando un puntaje al momento del ingreso en un hospital. Rev peru ginecol obstet. 2013;59:261-6. [ Links ]
22. Ferreira A, Ayres-de-Campos D. Vaginal breech delivery - is it still an option? Acta Obstet Ginecol Port. 2016;10(2):142-7. [ Links ]
23. Hofmeyr GJ, Hannah M, Lawrie TA. Planned caesarean section for term breech delivery. Cochrane Database Syst Rev. 2015;2015(7):CD000166. Published 2015 Jul 21. doi:10.1002/14651858.CD000166.pub2 [ Links ]
24. Royal College of Obstetricians and Gynaecologists. Caesarean section (NICE clinical guideline 132). Published date: 23 November 2011:282 p. [ Links ]
25. The American College of Obstetricians and Gynecologists. Practice Bulletin No. 161: External cephalic version. Washington (US). Obstet Gynecol. 2016 Feb;127(2):e54-61. DOI: 10.1097/AOG.0000000000001312 [ Links ]
26. Robson M, Hartigan MB, Murphy M. Methods of achieving and maintaining an appropriate caesarean section rate. Best Pract Res Clin Obstet Gynaecol. 2013 Apr;27(2):297-308. DOI: 10.1016/j.bpobgyn.2012.09.004 [ Links ]
Received: October 28, 2019; Accepted: April 02, 2020











 texto en
texto en