Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Ginecología y Obstetricia
On-line version ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.66 no.2 Lima Apr-Jun 2020
http://dx.doi.org/10.31403/rpgo.v66i2254
Case Report
Fetal ovarian cyst torsion. A case report
1. National Institute of Perinatology. Mexico City, Mexico
2. Mexican Social Security Institute, Poza Rica, Veracruz, Mexico
Fetal ovarian cysts are the most frequent fetal abdominal tumors. With an incidence of 1 in 2 500 live births and unilateral predominance, these cysts are generally diagnosed after 29 weeks’ gestation, when the hypothalamic-pituitary-gonadal axis has reached maturity. They are usually small, self-resolving and have limited clinical impact. Follow-up every two weeks is recommended; cysts larger than 4 cm have the highest complication rates. If it consistently presents the features of a simple cyst, it is recommended to wait until term for resection. We report the case of a fetus with an abdominal tumor diagnosed as fetal cyst, which prompted weekly monitoring of fetal hemodynamic parameters and cesarean section at 37 weeks. The newborn underwent laparotomy with left salpingo-oophorectomy. Fetal ovarian cyst torsion was diagnosed by histological examination.
Key words: Ovarian neoplasms; mechanical torsion; Fetus
Introduction
Fetal ovarian cysts are abdominal tumors frequently diagnosed after 29 weeks’ gestation, upon activation of the hypothalamic-pituitary-gonadal axis1. Of unilateral predominance, their incidence is 1 in 2 500 live births.
Most cases are small and resolve spontaneously without clinical problems. However, some may present complications such as torsion, thus requiring an emergency C-section2.
Etiology is unknown; hormone stimulation, in the form of beta-hCG, fetal gonadotropins and maternal estradiol, is considered the main cause. In most cases, the interruption of hormone stimulation at birth leads to spontaneous regression1.
Case report
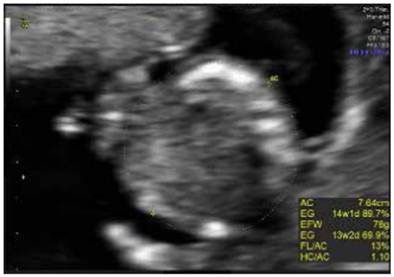
We present the case of a 33-year-old woman, gravida 2, with one prior cesarean delivery at 38 weeks of a healthy fetus and no other relevant medical history. The patient came at 13.3 weeks for her first trimester screening, in which the ultrasound scan found no fetal alterations (Figure 1).
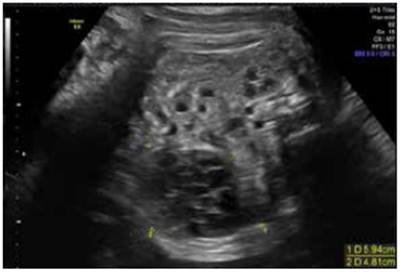
The pregnancy evolved normally. Structural ultrasound at 20.3 weeks showed anatomical integrity without anomalies and an abdominal circumference in the 74th percentile, one week larger than expected at fetometry (21.3 weeks gestation) (Figure 2).
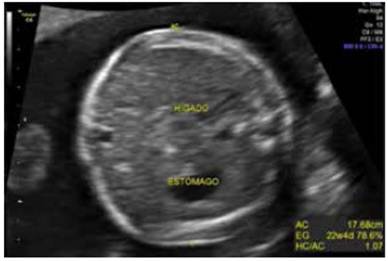
Figure 2 Abdominal perimeter at 20.3 weeks, one week older than expected when dated by last menstrual period
In the follow-up ultrasound scan at 27.5 weeks, the estimated weight was 1 548 g, in the 68th percentile. The abdominal circumference, in the 85th percentile, was 2 weeks and 4 days larger than expected when dated by last menstrual period (30.2 weeks).
At 32.3 weeks, we observed an abdominal fetal tumor. The evaluation by maternal-fetal medicine reported the abdominal circumference was in the 94th percentile, two weeks larger than expected when dated by last menstrual period (34.3 weeks). It also evidenced a well-defined abdominal tumor in the left flank under the stomach measuring 3.83 x 4.7 cm, with probable diagnosis of meconium peritonitis. It was decided to monitor the fetus, with no indication for surgery (Figure 3).

Figure 3 Abdominal tumor in left flank under the stomach, measuring 3.83 x 4.7 cm, at 32.3 weeks gestation.
In the following week, abdominal circumference was over the 97th percentile, two weeks and 3 days larger than expected at fetometry (35.3 weeks). The tumor in the left flank had grown to 5.53 x 4.52 cm, with adjacent bowel wall thickening, unaltered hemodynamics, normal amniotic fluid, and a reactive nonstress test. Given these findings, it was decided to continue monitoring until term (Figure 4).
One week later, tumor diameter remained stable and fetal wellbeing tests were within normal ranges, so cesarean delivery was programmed at 37 weeks. Surgery was performed without complications; the female newborn weighted 3 150 g, measured 48 cm, had an Apgar score of 8 out of 9, and a Silverman score of 2, without need for supplemental oxygen.
Within the first 24 hours after birth, an abdominal ultrasound of the newborn revealed a septated cystic mass in the left lower quadrant, which was diagnosed as probable meconium peritonitis. A CT scan showed an abdominal mass withnprobable diagnosis of left meconium peritonitis versus complex left ovarian cyst.
The patient was programmed for a left exploratory laparotomy. Upon finding a cystic mass dependent of the left ovary, left salpingo-oophorectomy was performed. On the second day, the newborn was discharged without complications; she presented no late complications in the pediatric follow-up.
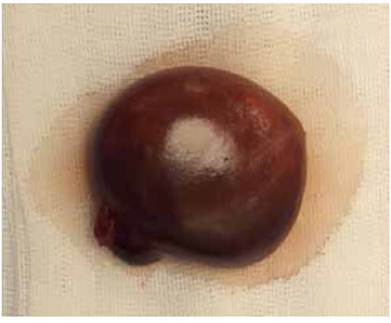
The pathology report described a cystic nodule measuring 4.5 x 3.0 x 3.0 cm; its histological section revealed a unilocular cyst with smooth internal walls and friable blood-like contents. The de finitive histopathologic diagnosis was left ovarian serous cystadenoma with torsion (Figure 5).
Discusion
Risk factors for fetal ovarian cyst formation include a disruption in blood flow to the primary gonad, fetal hypothyroidism, and congenital adrenal hyperplasia. Maternal and fetal cysts may coexist, which could support a shared etiology1.
Probable diagnoses for a fetal abdominal mass include hydronephrosis, megacystis, anal atresia, urachal cyst, meconium pseudocyst, hydrometrocolpos or fetal cyst3.
While cysts may cause fetal anemia or compression, or present rupture during the prenatal period, the most common complication is intracystic hemorrhage, followed by torsion. To date, consensus has not been reached on how to properly manage this condition, nor on the opportune moment for surgery4.
In order to evaluate the torsion of a fetal ovarian cyst in abdomen (not in pelvis), measuring the peduncle is more effective than measuring the cyst’s diameters. However, these values have to be obtained by abdominal ultrasound of the patient, which is a complex, unavailable technique in the antenatal period5.
Follow-up is recommended every two weeks after diagnosis; cysts larger than 4 cm present the most complications. If the ultrasound features are those of a simple cyst, it is preferable to wait until after delivery for surgery4.
Intracystic hemorrhage is an important parameter to predict torsion. Possible scenarios that could prompt surgery while acting in the best interest of our patients include complications of torsion, suspicion of an adnexal mass and abdominal obstruction. Performing a C-section after lung maturation in ovarian torsion may save the fetus’ life and ovary from necrosis; the time between diagnosis and surgery must be no longer than two weeks4.
In conclusion, fetal ovarian cysts have a low frequency, despite being the main cysts diagnosed in the prenatal period. The case we presented illustrates the difficulty of obtaining an antena-tal diagnosis, as well as the importance of close monitoring until term, in the absence of complications. Finally, it also highlights the need for a comprehensive neonatal assessment at birth.
REFERENCES
1. Erol O, Erol MB, Isenlik BS, Özkiraz S, Karaca M. Prenatal diagnosis of fetal ovarian cyst: case report and review of the literature. J Turk Ger Gynecol Assoc. 2013;14(2):119. doi: 10.5152/jtgga.2013.58855 [ Links ]
2. Kwak DW, Sohn YS, Kim SK, Kim IK, Park YW, Kim YH. Clinical experiences of fetal ovarian cyst: diagnosis and consequence. J Korean Med Sci. 2006 Aug 1;21(4):690-4 doi: 10.3346/jkms.2006.21.4.690 [ Links ]
3. Tyraskis A, Bakalis S, David AL, Eaton S, De Coppi P. A systematic review and meta-analysis on fetal ovarian cysts: impact of size, appearance and prenatal aspiration. Prenat Diagn. 2017 Oct 1. doi: 10.1002/pd.5143 [ Links ]
4. Yilanlioglu NC, Semiz A, Akpak YK, Sarimurat N, Tutak E, Cekmez Y, Ozben M, Karaca N. Fetal ovarian cyst torsion: Antenatal evaluation and management. Bezmi Sci. 2016;2:80-2 doi: 10.14235/bs.2016.764 [ Links ]
5. Trinh TW, Kennedy AM. Fetal ovarian cysts: review of imaging spectrum, differential diagnosis, management, and outcome. Radiographics. 2015 Mar 12;35(2):621-35. doi: 10.1148/rg.352140073 [ Links ]
Received: September 20, 2019; Accepted: January 24, 2020











 text in
text in