Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Ginecología y Obstetricia
On-line version ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.66 no.2 Lima Apr-Jun 2020
http://dx.doi.org/10.31403/rpgo.v66i2255
Case report
Rupture of uterine artery pseudoaneurysm after cesarean section
1 Obstetrics and Gynecology Service, Central Hospital "Dr. Urquinaona", Maracaibo, Zulia State, Venezuela
Postpartum hemorrhage is an important cause of maternal mortality. The rupture of a uterine artery pseudoaneurysm, a rare vascular lesion of unknown prevalence, produces secondary postpartum hemorrhage without an evident cause. If not properly diagnosed and treated, it can be life threatening. Etiology includes vascular trauma during cesarean section, vaginal delivery, curettage or hysterotomy. Its clinical presentation is varied and often associated with other more frequent gynecological and obstetric pathologies. Patients may present no symptoms, vaginal bleeding or even postpartum hemorrhage and hypovolemic shock. To prevent fatal bleeding, a rapid and accurate diagnosis must be made, based on non-invasive imaging studies. Angiographic embolization is a safe and effective method to control hemorrhage in hemodynamically stable patients and should be an option before resorting to surgery in selected cases. We describe a case of rupture of uterine artery pseudoaneurysm following a cesarean section.
Key words: Uterine artery; pseudoaneurysm; Postpartum hemorrhage; Angiography
Introduction
A pseudoaneurysm is a collection of extraluminal blood in an arterial wall defect, contained by the adventitia or by surrounding perivascular soft tissue1. A uterine artery pseudoaneurysm is a rare complication of unknown prevalence, in which a lacerated wall of the uterine artery presents inadequate sealing. It may manifest as severe hemorrhage in the late post-operative period, depending on size of the lesion and intramural pressure2. It may also be asymptomatic, or cause vaginal bleeding, abdominal pain, hypovolemic shock or fever, if it is infected. It must be considered as a differential diagnosis in cases of late genital bleeding without evident cause and history of gynecologic or obstetric surgery1-4. We describe the case of a patient who presented rupture of uterine artery pseudoaneurysm after a C-section.
Case report
A 26-year-old patient, gravida 3, para 2, with history of previous cesare- an section, was admitted for heavy genital bleeding with blood clots that had started in the last 24 hours, accompanied by dizziness, after 5 days of fever. The patient had undergone a C-section due to breech presentation without complica- tions 16 days before; the newborn weighted 3 200 g and had Apgar scores of 7 and 9 at min- ute one and five, respectively. On the third day postpartum, the patient had been discharged, asymptomatic. Her pregnancy had been normal and she denied history of coagulation disorders.
At admission, physical examination showed fe- ver (38.3°C), blood pressure of 122/70 mmHg and heart rate of 145 bpm. The patient present- ed breast swelling; her abdomen was bland, de- pressible and slightly painful, without bloating nor rigidity. Uterine size resembled that of a 10 weeks’ gestation; uterine tone was normal. At vaginal examination, the external os was closed, and there were moderate bright red blood and some clots in vagina. Adnexa mobilization was painless; there were no palpable tumors. White blood cell count was 14 100 cells/mL, neutrophils 85%, platelets 395 000/L and hemoglobin 8,6 g/dl. Liver and renal function tests, coagulation profile and electrolytes were normal. Upon admission, the patient was treated with tranexamic acid, methylergometrine, crystalloids, blood products and antibiotics. To limit bleeding, uterine com- pression by urinary catheter was applied. Her di- agnosis was secondary postpartum hemorrhage.
Abdominopelvic ultrasound showed hypoecho- ic material inside the uterine cavity consistent with clots; however, in the lower left quadrant of the lower uterine segment, it revealed a small oval anechogenic image measuring 12 x 10 mm close to the endometrial cavity, with a hyperin- tense border near the zone of hysterorrhaphy, accompanied by a small amount of free intra- cavitary fluid. Doppler ultrasound evidenced turbulent blood flow inside the lesion (Figure 1). These studies suggested the possible diagnosis of uterine artery pseudoaneurysm, which was confirmed by pelvic CT angiography (Figure 2).
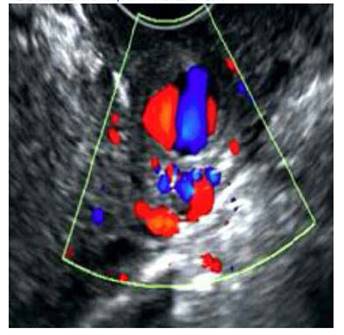
Figure 1 Color doppler image of the cystic lesion in uterus, measuring 12 x 10 mm, with turbulent flow.
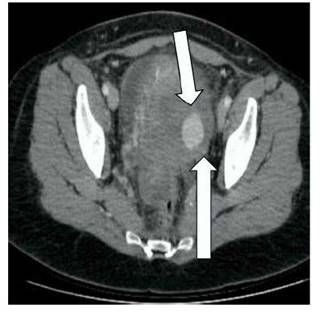
Figure 2 Coronal image of ct angiography. the lower arrow points to the left uterine artery and the upper arrow points to the pseudoaneurysm of the left uterine artery.
Because of these findings, the persistent bleed- ing despite pharmacological and mechanical measures, and the potential risks of hysterec- tomy, it was advised to perform arterial embolization. The patient was transferred to the interventional radiology service, where, by means of a digital subtraction angiography, the internal iliac vessels were removed to reveal an irregular collection of contrast (approximately 2 cm in diameter) inside the pseudoaneurysm, in the distal end of the left uterine artery. The contrast did not enter the vagina. Selective catheterization of uterine arteries and embolization with a microcatheter were performed, without complications. Genital bleeding decreased significantly. CT angiography and angiogram after treatment showed thrombosis of the pseudoaneurysm, with preservation of the other branches of the internal iliac arteries (Figure 3).
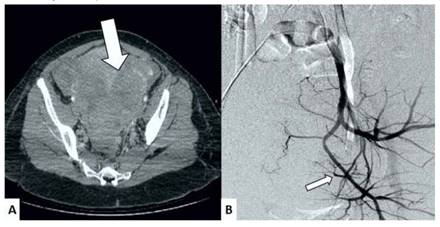
Figure 3 Images after the embolization. a) ct scan; the arrow points to the thrombosed pseudoaneurysm. b) angiography; the arrow points to the occlusion of the left uterine artery.
After the embolization, genital bleeding disappeared and the patient said she was feeling well. A follow-up ultrasound showed no pseudoaneurysm.
White blood cell count returned to normal values by the fifth day post procedure and the patient was discharged after completing antibiotic therapy.
11 days after embolization, the patient returned with a new episode of heavy genital bleeding followed by hypovolemic shock due to intraabdominal hemorrhage. At laparotomy, the anterior uterine surface was densely adhered to the abdominal wall. Because the peritoneal surface was swollen and friable, subtotal abdominal hysterectomy with conservation of both adnexa was performed. The patient was discharged on the fifth postoperative day. After a 16-month follow-up, the patient has not presented complications nor new episodes of genital bleeding.
Pathological examination of the surgical specimen reported a higher number of blood vessels, with thickened vascular walls and hyalinization throughout the myometrium, accompanied by hemorrhage in the basal layer of the endometrium and scarce inflammatory reaction. The uterine artery showed a pouch 15 mm in diameter, with a 5 mm defect in its surface. At microscopy, we found that the pseudoaneurysm wall was composed exclusively of adventitia.
Discussion
Postpartum hemorrhage is an important cause of maternal morbidity and mortality. Secondary postpartum hemorrhage is defined as excessive bleeding from 24 hours until six weeks after delivery. If the cause is unknown, it can be mortal. Possible etiologies include placental retention, endometritis, subinvolution of the placental bed, uterine artery pseudoaneurysm, arteriovenous malformations and choriocarcinoma1,2.
A pseudoaneurysm, also called false aneurysm, is an extravascular blood collection similar to a hematoma, produced outside the arterial wall, characterized by leaking of arterial blood contained by surrounding tissue, which may break and cause severe hemorrhages. Most cases present after gynecologic surgery4-6. The proposed pathophysiological mechanisms for vascular injury are massive artery ligation or puncture wounds when a suture is passed between two vessels. This leads to an expanding periarterial hematoma, vein drainage or both, which would result in a secondary aneurysm or pseudoaneurysm lacking a complete arterial wall with three layers (intima, media, adventitia)(4. This vascular lesion may occur spontaneously or secondary to inflammation, trauma or local infection5.
Clinical manifestations are various, unspecific and unpredictable. It may be asymptomatic or present as a late postpartum or postoperative hemorrhage, and be potentially mortal up to two years after surgery3,7. Diagnostic difficulties arise from its unknown frequency and variable presentation of vaginal bleeding. By sustained pressure, blood dissects the tissue around the damaged artery, creating a perfused pouch. While in contact with the originating vessel, the blood continues dissecting, establishing a connection with the uterine cavity that leads to late hemorrhage, usually massive and unexpected8.
Pseudoaneurysms can be identified by ultrasound, CT scan or angiography. Ultrasound and CT scan are used as initial diagnostic techniques. At grayscale ultrasound, this lesion appears as an anechoic cystic lesion, with turbulent arterial flow at Doppler evaluation. Pathognomonic signs have been proposed: the "to-and-fro" waveform in the neck and the "yin-yang sign" in the main body of the pseudoaneurysm. During systole, blood enters because of the higher blood pressure; in diastole, pressure falls and the blood returns through the neck of the pseudoaneurysm9. Contrast CT scan may rule out other more frequent causes of secondary postpartum hemorrhage and identify the aneurysm. Besides, CT angiography may show the originating artery. Nevertheless, conventional angiography remains as the gold standard for diagnosing and treating vascular anomalies. The precise diagnosis of secondary postpartum hemorrhage avoids unnecessary interventions, thus limiting blood loss that puts the patient’s life at risk10.
Initial treatment includes volume replacement and blood transfusions, as well as mechanical compression on vagina or uterus. Since rupture is unpredictable, conservative treatment is not a viable option2. If the bleeding persists, treatment options include hysterectomy, surgical ligation or selective embolization of the uterine artery. Embolization, first described in 1979, is useful to control the bleeding; its success rate is circa 97%(11). In comparison, success rates for ligation of the internal iliac artery vary from 42% to 100%12). Furthermore, embolization has advantages such as less morbidity and the possibility of locating the site of hemorrhage. With this technique, the occlusion can be more distal than with surgical ligation, thus preserving fertility, unlike hysterectomy13). Complications are rare because of the abundant vasculature of the pelvis; they include postoperative fever and transitory ischemia (both respond to symptomatic treatment), sciatic and perineal nerves neuropathy, muscle pain and post-embolization syndrome. The procedure has to be practiced bilaterally to ensure its effectiveness and prevent reperfusion(14). Surgery must be performed if embolization has failed15.
In conclusion, uterine artery pseudoaneurysm is a rare but important cause of secondary postpartum hemorrhage. In cases with history of C-section, this hemorrhage may lead to hypovolemic shock. Uterine artery pseudoaneurysm can be mortal and must be considered as a differential diagnosis. For these cases, angiographic embolization is a treatment option to consider before surgery.
REFERENCES
1. Subramaniam S, Nadarajan C, Aziz ME. Role of uterine artery embolization in pseudoaneurysm of uterine artery: a rare cause of secondary postpartum hemorrhage. Cureus. 2018;10(2):e2220. doi: 10.7759/cureus.2220 [ Links ]
2. Isono W, Tsutsumi R, Wada-Hiraike O, Fujimoto A, Osuga Y, Yano T, et al. Uterine artery pseudoaneurysm after cesarean section: case report and literature review. J Minim Invasive Gynecol. 2010;17(6):687-91. doi: 10.1016/j.jmig.2010.06.004 [ Links ]
3. Jennings L, Presley B, Krywko D. Uterine artery pseudoaneurysm: a life-threatening cause of vaginal bleeding in the emergency department. J Emerg Med. 2019;56(3):327-31. doi: 10.1016/j.jemermed.2018.12.016 [ Links ]
4. Usman R, Jamil M, Rasheed M. True aneurysm of the uterine artery in a young nulliparous female: an extremely rare vascular entity. Ann Vasc Dis. 2018;11(4):542-4. doi: 10.3400/avd.cr.18-00066 [ Links ]
5. Takeda A, Kato K, Mori M, Sakai K, Mitsui T, Nakamura H. Late massive uterine hemorrhage caused by ruptured uterine artery pseudoaneurysm after laparoscopic-assisted myomectomy. J Minim Invasive Gynecol. 2008;15(2):212-6. doi: 10.1016/j.jmig.2007.09.006 [ Links ]
6. Feld Z, Rowen T, Callen A, Goldstein R, Poder L. Uterine artery pseudoaneurysm in the setting of deep endometriosis: an uncommon cause of hemoperitoneum in pregnancy. Emerg Radiol. 2018;25(1):107-10. doi: 10.1007/s10140-017-1560-0 [ Links ]
7. Pérez-Ezquerra BR, Carazo-Hernández B, Arribas-Marco T, Guardia-Dodorico L. Pseudoaneurisma de arteria uterina después de una cesárea. Ginecol Obstet Mex. 2013;81(3):166-70. [ Links ]
8. Wan AY, Shin JH, Yoon HK, Ko GY, Park S, Seong NJ, et al. Post-operative hemorrhage after myomectomy: safety and efficacy of transcatheter uterine artery embolization. Korean J Radiol. 2014;15(3):356-63. doi: 10.3348/kjr.2014.15.3.356 [ Links ]
9. Mahmoud MZ, Al-Saadi M, Abuderman A, Alzimami KS, Alkhorayef M, Almagli B, et al. To-and-fro waveform in the diagnosis of arterial pseudoaneurysms. World J Radiol. 2015;7(5):89-99. doi: 10.4329/wjr.v7.i5.89 [ Links ]
10. Ludwin A, Martins WP, Ludwin I. Managing uterine artery pseudoaneurysm after myomectomy. Ultrasound Obstet Gynecol. 2018;52(3):413-5. doi: 10.1002/uog.18963 [ Links ]
11. Singhal S, Singh A, Raghunandan C, Gupta U, Dutt S. Uterine artery embolization: exploring new dimensions in obstetric emergencies. Oman Med J. 2014;29(3):217-9. doi: 10.5001/omj.2014.53 [ Links ]
12. Su CW. Postpartum hemorrhage. Prim Care. 2012;39(1):16787. doi: 10.1016/j.pop.2011.11.009 [ Links ]
13. McLucas B, Voorhees WD 3rd, Elliott S. Fertility after uterine artery embolization: a review. Minim Invasive Ther Allied Technol. 2016;25(1):1-7. doi: 10.3109/13645706.2015.1074082 [ Links ]
14. Kaur R, Singh R. Effective management of early cervical pregnancy with bilateral uterine artery embolization followed by immediate evacuation and curettage: A case report. J Obstet Gynaecol India. 2017;67(1):66-9. doi: 10.1007/s13224-016-0943-6 [ Links ]
15. Hongsakul K, Songjamrat A, Rookkapan S. Transarterial embolization for the treatment of massive bleeding in gynecologic and obstetric emergencies: a single center experience. Emerg Radiol. 2014;21(4):333-9. doi: 10.1007/s10140-014-1198-0 [ Links ]
Received: May 16, 2019; Accepted: November 01, 2019











 text in
text in 


