Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista Peruana de Ginecología y Obstetricia
versão On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.66 no.3 Lima jul-sep 2020
http://dx.doi.org/10.31403/rpgo.v66i2265
Original Articles
Gestation in times of COVID-19 pandemic. Hospital Nacional Docente Madre Niño San Bartolomé, Lima, Peru
1 Departament of Gynecology and Obstetrics , Hospital Nacional Docente Madre Niño San Bartolomé, Lima, Perú
2Universidad Nacional Mayor de San Marcos, Lima, Perú
Introduction: COVID-19 and pregnancy is a new intercurrence in risk assessment for the care of the pregnant woman. Since the beginning of the pandemic in the country, cases have been increasing. The first case attended at the San Bartolomé Hospital was on April 12. Since the first reports of COVID+ pregnant women in China, to date, there is more important information on epidemiology and perinatal results for the management of the COVID+ pregnant woman. Objective: To determine the epidemiology and maternal perinatal outcomes of COVID-19 in pregnant women at the Hospital Nacional Docente Madre Niño San Bartolomé, Lima, Peru. Methods: Observational cross-sectional study, from April to July 2020. All the pregnant women who arrived at the obstetric emergency at Hospital San Bartolomé were included, and they underwent an immunochromatography test for IgM / IgG, to determine the seroprevalence of COVID-19. Obstetric and perinatal variables were collected in a data sheet upon admission to the emergency room. Results: Rapid test for SARS-CoV-19 was performed in 345 pregnant women who were hospitalized for delivery care. The average age was 27 years, with 10% adolescents and 16% over 35 years; 60% had 2 to 4 pregnancies, 38% of deliveries were vaginal, 15% of them preterm; 1.2% of the pregnant women were symptomatic and 0.2% were admitted to the intensive care unit. 61% of the newborns weighed between 2 500 and 3 500 g, 53% were male, 94% had an Apgar score greater than 7 at one minute, 3.3% with a positive swab within the first 24 hours. There were 3% fetal deaths. 48% of the pregnant women came from the Northern Cone of the city of Lima. Conclusions: Almost 100% of the pregnant women were asymptomatic and only 0.2% had respiratory complications. The mode of delivery by cesarean section was low in relation to other publications, all had obstetric indication. A small number of neonates had a positive swab. There was a higher incidence of fetal deaths in July 2020. The highest percentage of patients came from the Northern Cone of Lima.
Key words: Pregnancy; Coronavirus infections; SARS-CoV-19. COVID-19; Stillbirth; Lima; Peru
Introduction
In December 2019, cases of unidentified cause pneumonia were reported in Wuhan City, a city of 11 million inhabitants in the People's Republic of China. Subsequent research revealed that they were caused by a new coronavirus, called SARS-CoV-2. The COVID-19 infection spread rapidly to neighboring countries, such as Japan, Thailand, and then the virus traveled with people to different parts of the world. This virus is a family of viruses that cause Middle Eastern Respiratory Syndrome (MERS) and Acute Severe Respiratory Syndrome (SARS) (1.2).
Pneumonia, regardless of the etiological cause, causes morbidity and mortality. It is the most prevalent non-obstetric infection in pregnancy, being considered in some studies as the third leading cause of maternal death in pregnancy. 25% of cases need ventilatory support in intensive care units3-5.
Viral pneumonia has twice as much morbidity as bacterial pneumonia. It is proposed that changes in cell-mediated immunity and those in lung function affect the susceptibility and severity of pneumonia (6.7). The rate of influenza fatality in the 1918-1919 pandemic was 27% 8. During the Asian influenza epidemic in 1957-1958, 10% of all deaths occurred in pregnant women and the fatality rate was double compared to nonpregnant women9. The most common adverse events associated with maternal pneumonia were premature rupture of membranes, preterm birth, intrauterine death, intrauterine growth restriction (IUGR), and neonatal death.
In Peru, the first case of coronavirus was reported on March 6, 2020, and quarantine for the entire population was determined in Peru on the 15th of the same month. Since that day, restrictions on health services, as regards external consultation, have been restricted; only the emergency was in charge of handling the cases. The Hospital San Bartolomé was no stranger to this reality and has had to adapt its facilities to face the challenge of managing the pregnant COVID+. Being a pathology unknown to the world, in the field of obstetrics it is too. It is therefore important to show the experience of San Bartolomé hospital in the management of COVID+ patients. During this period, 1 869 pregnant women have been treated, allowing epidemiological and maternal-neonatal variable data to be used to make better decisions in the management of these patients.
Methods
A cross-sectional observational study was conducted in April to July 2020, which included all pregnant women who arrived at the obstetric emergency of Hospital San Bartolome, who had an immunochromatography test for IgM/IgG, (rapid test) to determine the seroprevalence of SARS-CoV-19. The maternal variables obtained were age, parity, type of delivery and place of origin; and neonatal ones, newborn weight, Apgar, sex, swabbing positivity and fetal death. This data was collected in a data sheet and then processed in the Stata statistical program.
Results
The average age of patients was 27 years, with adolescents being 10% of all COVID+ patients and patients over 35 years of age 16%, representing the extremes of these ages approximately 25%. The youngest patient was 14 years old and the eldest 48 years old. In terms of parity, the group of seconds and four-pregnant women represented 58% of the total, first pregnancy 32% and the multi.pregnancy group (>5 pregnancies) 10%.
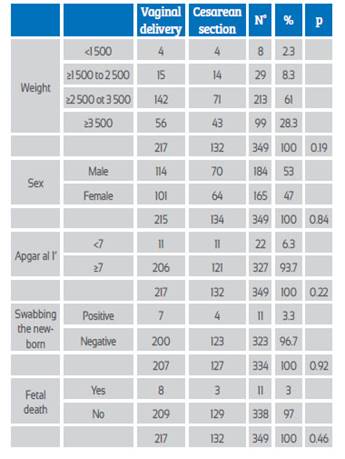
The culmination route of delivery was vaginal in 62% and cesarean section in 38%. In two of the four twin pregnancies, the second baby was born by C-section, so 347 births were considered. 15% of births were preterm, with 11% of them late preterm; 84% were full-term pregnancies. 98.8% of all pregnant women were asymptomatic; only 1.2% presented respiratory symptomatology, with oxygen saturation below 93, and 0.28% needed ventilatory support in the intensive care unit (ICU) (Table 1).
60% of newborns (NB) weighted between 2 500 and 3 500 g, 2.3% less than 1 500 g and 28.3% more than 3 500 g. 53% were male and 47% female. Apgar under 7 per minute accounted for 6% and 94% had Apgar ≥ 7. 3.3% of the 334 swabs made to the NB within the first 24 hours were positive. There were 11 (3%) fetal deaths, zero in May, one in June and 10 in July (Table 2).
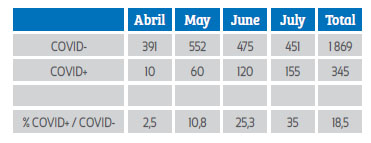
In April there were 10 cases of COVID+ pregnant women, increasing progressively during the months of May to 60 cases, June 120 cases and July 155 cases. The highest percentage of cases was in July, with 35% (Table 3).
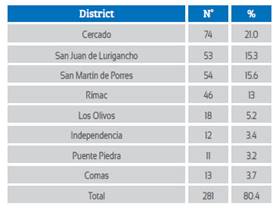
48% of COVID+ women came from the northern cone of Lima, 25% were from Lima Cercado and 19% from Lima East. When analyzing by districts, 21% of the pregnant women corresponded to the Cercado de Lima, secondly, the district of San Martín de Porres with 15.6%, followed by San Juan de Lurigancho with 15.3% and fourthly the Rimac (Table 4).
From April to July there were 11 stillbirths, of which10 arrived as such and one was institutional, representing 3.2% of fetal deaths. These presented during the months of June1 and July10. The stillbirths had less weight relative to living fetuses, this finding being significant. The average weight of COVID+ mother's children was 2 205 g and in the case of COVID-, the average weight was 3 218.
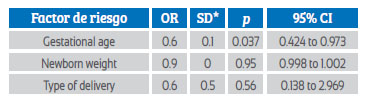
When the logistic regression model is done (Table 5) for the fetal death dependent variable versus the independent variables (gestational age, newborn weight, type of birth), it is noticeable that gestational age influenced the final fetal death event, but not the weight of the baby.
As for the mother's type of delivery and age, it is clear that those who terminated per vagina were younger in relation to those who had cesarean delivery (Table 1).
In relation to the newborn weight and the type of delivery, there was also statistical significance.
Discussion
The total number of participants attended at Hospital San Bartolomé from April to July was 1 869. Initially, the tests were not taken to all patients, being common practice since June, which can be seen in the increase in cases detected from that month. Every patient entering the delivery room was screened with a quick test, which was performed in the obstetric emergency. 346 of the 1 869 patients were diagnosed with COVID+. There was a progressive increase in cases, the highest number in July. The hospital is located in the Cercado de Lima, so it is to be expected that the largest number of patients will come from that area 25% of all patients. However, the Northern Cone was the area from which the patients mostly came (48%), being its districts San Martín de Porres, Los Olivos, Independencia, Puente Piedra and Comas.
As for the age group, the average age was 27 years, unlike studies such as Khan10, Huijun Chen 11 and Dashraath12, who found an average of 30 years, or Schwartz1 and Mullins13 who reported 31 and 32 years, respectively. The population of the present study was younger, even having a 14-year-old pregnant woman and 10% adolescents, somewhat similar to the study of Huertas14, who found an age range of 17 to 41 years.
The C-section rate (38%) is low in relation to other studies showing rates ranging from 84% to 100%, such as Khan's10, Huijun11 and Dashraath12. It should be noted that our study was conducted in a specialized level III hospital in which patients with the history of segmental C-section are given a chance of vaginal delivery. In two cases that were twin pregnancies, C-section had to be performed for the birth of the second baby. The decision to culminate by C-section was eminently obstetric, similar to what Chen et al. proposed15.
Studies mainly in Asia report a preterm birth rate ranging from 20% to 72%. Nationally, the study at the Rebagliati hospital in EsSalud, Huertas y col. 14report an 18% rate of preterm neonates. In our study, the preterm neonates accounted for 15%, a result closer to EsSalud's data. In addition, our work found an association between the pregnancy's delivery route and gestational age.
Regarding maternal complications, there was only one case that was admitted to the maternal ICU. Diagnosis was preeclampsia and COVID+, with oxygen saturation below 93%; childbirth was by C-section. This patient remained in ICU for 70 days, leaving on her own at 90 days postpartum. This single patient accounted for 0.28% of all COVID+ pregnant women, a low rate compared to other publications that find 6% to 34% complications12-15. In the systematic review of more than 2 000 patients, Asma Khalil found that 3.7% of patients were admitted to mechanical ventilation 16.
Regarding fetal death in this study, during July there were 156 births and 10 fetal deaths. Mullins' study13 publishes 32 participants including a single fetal death and one neonatal death. On the other hand, Lehan Lui's study between January and February 2020 does not describe fetal death or neonatal deaths17. It is notorious that in the present study there were more deaths than those found in other countries. It should be considered that there is currently no prenatal control consulting; pregnant women who arrive at the emergency have not had prenatal control in the third trimester. 6% of babies had Apgar under 6 per minute; the highest percentage of newborn babies were born with a good Apgar score, as described in other publications.
When swabbing was performed to neonates during the first 24 hours of life, positivity was found in 11 cases (3%), remaining these babies in the neonatology service in a differentiated environment. Huaping Zhu reports that 6 out of 10 babies who had some symptomatology, none came out positive in the swabbing18.
When performing logistic regression (Table 5) with fetal death as the final event, an OR of 0.6 and p < 0.05 was found for the gestational age variable, which had a protective effect on the final variable or event (death).
As found in this work on the experience in pregnant people at Hospital San Bartolomé, we can conclude that the route of delivery has been very similar to that of patients no COVID. The age group was young relative to other experiences. Most patients were asymptomatic, and there were few participants with respiratory complications. Preterm births predominantly late preterms had a higher percentage compared to the national average. The highest percentage of neonates was negative for the swab test.
REFERENCES
1. Schwartz DA, Graham AL. Potential maternal and infant outcomes from (Wuhan) coronavirus 2019-nCoV infecting pregnant women: lessons from SARS, MERS, and other human coronavirus infections. Viruses. 2020 Feb;2(2):194. doi: 10.3390/v12020194 [ Links ]
2. Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, Tong S. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics. 2020. doi:10.1542/peds.2020-0702 [ Links ]
3. Berkowitz K, LaSala A. Risk factors associated with the increasing prevalence of pneumonia during pregnancy. Am J Obstet Gynecol. 1990;163:981-5. https://doi.org/10.1016/0002-9378(90)91109-P [ Links ]
4. Madinger NE, Greenspoon JS, Eilrodt AG. Pneumonia during pregnancy: Has modern technology improved maternal and fetal outcome? Am J Obstet Gynecol. 1989;161:657-62. https://doi.org/10.1016/0002-9378(89)90373-6 [ Links ]
5. Visscher HC, Visscher RD. Indirect obstetric deaths in the state of Michigan 1960-1968. Am J Obstet Gynecol. 1971;109:1187-96. https://doi.org/10.1016/0002-9378(71)90664-8 [ Links ]
6. Weinberger S, Weiss S, Cohen W, Weiss J, Johnson TS. Pregnancy and the lung. Am Rev Resp Dis. 1980;121:559-81. https://doi.org/10.1164/arrd.1980.121.3.559 [ Links ]
7. Harris JW. Influenza occurring in pregnant women; a statistical study of thirteen hundred and fifty cases. JAMA. 1919;72:978-80. doi:10.1001/jama.1919.02610140008002 [ Links ]
8. Eickhoff TC, Sherman IL, Serfling RE. Observations on excess mortality associated with epidemic influenza. JAMA.1961;176:776-82. doi:10.1001/jama.1961.03040220024005 [ Links ]
9. Instituto de Evaluación de Tecnologías en Salud e Investigación. Transmisión SARS-CoV-2 Madre-Feto: Síntesis Rápida de Evidencia 05-2020. Lima: ESSALUD; 2020. www.essalud. gob.pe/ietsi/pdfs/direcc_invest_salud/RRI_05_2020_V3.pdf [ Links ]
10. Khan S, Peng L, Siddique R, Nabi G, et al. Impact of CO-VID-19 infection on pregnancy outcomes and the risk of maternal-to-neonatal intrapartum transmission of COVID-19 during natural birth. Infection Control & Hospital Epidemiology. 2020;41(6):748-50. https://doi.org/10.1017/ice.2020.84 [ Links ]
11. Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, Liao J. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical record. Lancet. 2020:395(10226):809-15. https://doi.org/10.1016/S0140-6736(20)30360-3 [ Links ]
12. Dashraath P, Wong JLJ, Lim MXK, Lim ML, Li S, Biswas A, Choolani M, Mattar C, Su LL. Coronavirus disease 2019 (COVID-19) pandemic and pregnancy. Am J Obstet Gynecol. 2020 Jun;22(6):521-31. https://doi.org/10.1016/j. ajog.2020.03.021 [ Links ]
13. Mullins E, Evans D, Viner RM, O'Brien P, Morris E. Coronavirus in pregnancy and delivery: rapid review. Ultrasound Obstet Gynecol. 2020;55(5):586-92. https://doi.org/10.1002/uog.22014 [ Links ]
14. Huertas I, Elias J, Campos K, Muñoz R. Maternal and perinatal characteristics of pregnant woman with covid 19 in a national hospital in Lima Perú. Rev Peru Ginecol Obstet. 2020;66(2). DOI: https://doi.org/10.31403/rpgo.v66i2245 [ Links ]
15. Chen D, Yang H, Cao Y, Cheng W, Duan T, Fan C, et al. Expert consensus for managing pregnant women and neonates born to mothers with suspected or confirmed novel coronavirus (COVID-19) infection. Int J Gynecol Obstet. 2020;149(2):130-6. https://doi.org/10.1002/ijgo.13146 [ Links ]
16. Khalil A, Kalafat E, Benlioglu C, O'Brien P, Morris E, Draycott T, von Dadelszen P. SARS-CoV-2 infection in pregnancy: a systematic review and meta-analysis of clinical features and pregnancy outcomes. E Clin Med. 2020;100446. https://doi. org/10.1016/j.eclinm.2020.100446 [ Links ]
17. Liu D, Li L, Wu X, Zheng D, Wang J, Yang L, Zheng C. Pregnancy and perinatal outcomes of women with coronavirus disease (COVID-19) pneumonia: a preliminary analysis. Am J Roentgenol. 2020;1-6. doi.org/10.2214/AJR.20.23072 [ Links ]
18. Zhu H, Wang L, Fang C, Peng S, Zhang L, Chang G, Zhou W. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Translat Pediat. 2020;9(1):51. doi: 10.21037/tp.2020.02.06 [ Links ]
6Cite as: Vera Loyola EM, Montenegro Cruz IM, Cruzate Cabrejos V, Marcelo Pacheco H, Arce Benites M, Pelaez Chomba M. Gestation in times of COVID-19 pandemic. Hospital Nacional Docente Madre Niño San Bartolomé, Lima, Perú. Rev Peru Ginecol Obstet. 2020;66(3). DOI: https://doi.org/10.31403/rpgo.v66i2265
Received: July 23, 2020; Accepted: August 24, 2020











 texto em
texto em