Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Ginecología y Obstetricia
On-line version ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.66 no.3 Lima Jul-Sep 2020
http://dx.doi.org/10.31403/rpgo.v66i2273
Original Articles
Sars-CoV-2 in the second half of pregnancy: Maternal and perinatal outcomes
1Clínica San Gabriel, Lima, Perú
2Instituto Nacional de Salud del Niño - Breña, Lima, Perú
3 Departament of Gynecology and Obstetrics, Hospital Nacional Edgardo Rebagliati Martins, EsSalud, Lima, Perú
Introduction: The COVID-19 pandemic is a global health and social emergency. Knowledge is still limited about its effect on pregnant women. Objective: To describe maternal-perinatal outcomes of COVID-19 according to severity classification in women hospitalized in the second half of pregnancy. Methods: Retrospective, descriptive, observational study from March to July 2020 at Edgardo Rebagliati Martins National Hospital. All hospitalized pregnant women with RT-PCR and/ or rapid positive test for SARS-CoV-2 were included. Pregnancies less than 20 weeks and epidemiological discharges were excluded. Maternal characteristics at admission and maternal-perinatal outcomes were grouped according to the clinical classification of the disease. The qualitative variables are presented in counts and percentages; and quantitative ones, in medians and ranges. Results: 247 pregnant women were studied. Most of them were in the third trimester (76%). The most frequent presentation of the disease was asymptomatic (83%), and cases of severe pneumonia were few (3.2%). The cesarean section rate was high (60%), although vaginal deliveries doubled over time (0-24 a 44%). Severe cases had a higher rate of cesarean section (100%) and iatrogenic preterm delivery (75%). No maternal deaths were reported. There were 9 stillbirths and 5 positive neonates for SARS-CoV-2, both among asymptomatic and mild patients. 9 stillbirths and 5 positive neonates for SARS-CoV-2, both among asymptomatic and mild cases. Conclusions: The possibility of cesarean section and iatrogenic preterm delivery is greater in severe cases. The vaginal delivery rate increased in recent months. No perinatal complications related to COVID-19 were identified.
Key words: Coronavirus infections; COVID-19; SARS-CoV-2; Pregnancy; Pregnancy complications; infectious; Pregnancy outcome; Perinatal death; Lima; Peru
Introduction
The World Health Organization (WHO) reported the novel coronavirus SARS-CoV-2 for the first time on December 31, 2019, in Wuhan, China. In a few weeks, the virus has spread throughout China, and in less than a month, it had affected several countries. Later on, this disease has been named COVID-19, and its rapid expansion has covered all continents, being declared a pandemic on March 11, 20201.
In Peru, its rapid advance has resulted in a health and social emergency, leading to institutional changes in the care of COVID-19 patients, including pregnant women.
In a previous publication, it has been reported that universal screening with serological tests identified most of the cases in asymptomatic patients (68.3%), and among those who presented symptoms, cough (84.6%) and fever (76.9%) were the most frequent. Furthermore, the cesarean section rate was high (76.5%)2.
This study describes the maternal and perinatal outcomes according to the clinical classification of COVID-19, from March to July in the Hospital Nacional Edgardo Rebagliati Martins, Lima, Peru.
Methods
This is a descriptive, observational, retrospective study that included pregnant women attended from March to July 2020 at the HNERM. The inclusion criteria were: 1) Pregnant women who required hospital admission; 2) Diagnosis of SARS-CoV-2 infection confirmed by RT-PCR and/or rapid serological test according to guidelines of the Ministry of Health (MINSA)3). The exclusion criteria were: 1) Pregnancies less than 20 weeks; 2) Patients with epidemiological discharge according to MINSA resolution4.
The maternal clinical and laboratory characteristics are described upon admission due to emergency, as well as the maternal and perinatal results. The pregnant women, in turn, were grouped according to the clinical classification of the disease based on the resolution of the MINSA5.
During the study period, the rapid serological test SARS-CoV-2 Detection Kit (Zhejiang Orient Gene BioTech) was used first, with sensitivity 43.8% and specificity 98.9%.6) Later, the StandardTM Q COVID-19 IgM/IgG Combo Test (SD Biosensor) was available with a sensitivity of 88.5% and specificity 98.8%.7
The information was entered into an electronic filling form, and the data obtained were processed in the SPSS version 23 program. The values of the qualitative variables are presented using counts and percentages, whereas those of the quantitative variables, in medians and ranges.
Results
247 pregnant women with SARS-CoV-2 infection were analyzed and hospitalized for obstetric causes and/or pneumonia. Asymptomatic cases corresponded to 83.0% and mild cases to 10.5% of the population studied. Only 3.2% of the cases had severe COVID-19 pneumonia.
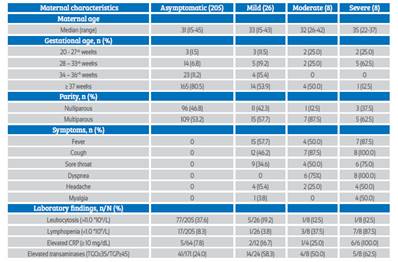
Of the asymptomatic patients, 80.5% were hospitalized with a full-term pregnancy. 75% of severe cases occurred in the third trimester, and 87.5% of these were premature. The most common symptoms were fever in 81.3% and cough in 84.4%. The most common laboratory findings in moderate and severe cases were elevated CRP, lymphopenia, and increased transaminases by 70%, 62.5%, and 56.3%, respectively.
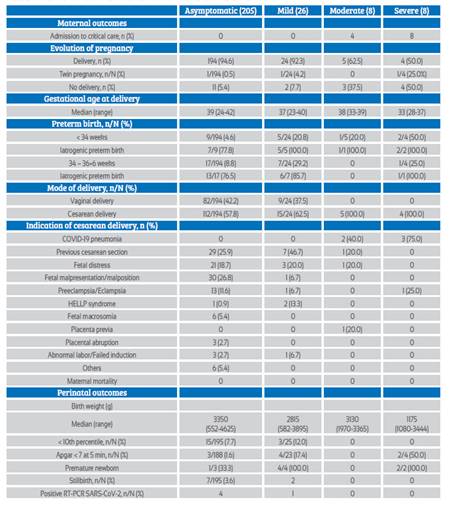
It was observed that 4.8% required admission to critical care in all severe cases, although in moderate ones, half remained in the obstetric service. No maternal deaths were reported.
Of the 227 patients, three delivered twins: one from the asymptomatic group, one from the mild symptomatic group, and one from a patient with severe pneumonia. Conversely, 19 were discharged pregnant, and one remained hospitalized until the end of the study. No patient with moderate or severe clinical presentation had vaginal delivery. The preterm birth rate was 18.5% and, within these, the medically indicated preterm birth rate was 83.3%, being 100% for moderate and severe cases.
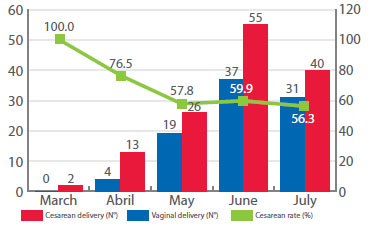
The overall cesarean section rate was 59.9%. A variation in time was observed: in March and April, there was a high rate (100%-76.5%) of cesarean sections, and from May it decreased significantly, reaching 56.3% in the month of July.
Median birth weight was 1 175 g in the offspring of patients classified as severe. In the asymptomatic group, 7.7% had infants weighting less than the 10th percentile, with 12% of the mild symptomatic group. There were 5 cases of perinatal transmission of SARS-CoV-2 confirmed by nasopharyngeal swab, as well as 9 cases of stillbirth, 8 of which occurred in the last two months of study.
Discussion
The form of presentation of the disease was mostly asymptomatic or mild in 231 cases, coinciding with what was described in the general population and pregnant women8-10. In a systematic review, Capobianco G. et al. described that the mean age of pregnant women was 30.2 years11, similar to that of the women in the present study.
Most of the admitted patients were in the third trimester of pregnancy, corresponding mainly to asymptomatic/mild cases. Crovetto et al. found in 874 women that hospital admission was significantly more prevalent in the last trimester12. Khalil et al. also describe in a systematic review, which included 2 567 pregnant women, that 75% were in the third trimester13.
In the present study, the parameters most frequently associated with moderate/severe cases were lymphopenia and elevated CRP. This coincides with what Pereira A. et al. correlated with severe pneumonia14.
The overall rate of cesarean sections was higher than that reported in a systematic review by Khalil et al., where it was 48.3%13). However, the HNERM is a referral center; most of its pregnant women have obstetric risk factors. It should be noted the decrease in the rate of cesarean sections as of May, with the consequent increase in vaginal deliveries.
Most of the patients admitted to a critical care unit were far from term, and severe cases were associated with high rates of cesarean section and iatrogenic preterm delivery. Only one patient in the severe group underwent surgery for preeclampsia with severe features, and in the immediate puerperium, she developed symptoms of COVID-19 pneumonia. In their cohort study, Martínez-Perez and Vouga found that iatrogenic preterm birth was indicated in all patients with severe COVID-1915. In a systematic review, Pettirosso found that the preterm birth rate ranged from 10% to 100%16).
The maternal death rate was zero, coinciding with the low or null mortality described in other studies17,18. In systematic reviews, it has been observed that maternal mortality occurred mainly in women with previous comorbidities13,19. These variables were not included in the present study.
Knowledge about the possible risk of vertical transmission is very limited. In order to demonstrate this, samples of placenta, amniotic fluid, cord blood and neonate should be collected immediately after delivery20. These requirements were not met in any of the neonates confirmed with SARS-CoV-2 infection, all being diagnosed with a swab taken in the first 24 hours of life. In addition, it is presumed that this occurs in patients with high viremia and severe clinical pictures, such as the case reported in France21.
The stillbirth rate increased in the last 2 months. Khalil et al. describe an increase in the incidence of stillbirths during the pandemic22. These changes could be due to the measures adopted by the pandemic, such as the restriction of care only to emergencies, and not being able to perform prenatal control or ultrasounds, to which is added the fear of patients to go to a health facility due to the risk of acquiring the infection.
In conclusion, the clinical and laboratory characteristics of the women seen during the COVID-19 pandemic were similar to those of non-pregnant women. There is a greater possibility of iatrogenic cesarean section and premature delivery in women who develop a severe infection. Due to institutional measures, the vaginal delivery rate doubled compared to baseline. Perinatal complications, death rate, and infected neonates do not seem to be directly related to COVID-19 during pregnancy. The limitations of the study lie in its retrospective nature, the underreporting, the diagnostic method that went from being combined to being almost exclusive to the rapid serological test, and the uniformity of the time of the neonatal RT-PCR sample collection.
REFERENCES
1. World Health Organization. Timeline of WHO's response to COVID-19. Last updated 30 July 2020. https://www.who.int/news-room/detail/29-06-2020-covidtimeline [ Links ]
2. Huerta Sáenz IH, Elías Estrada JC, Campos Del Castillo K, Muñoz Taya R, Coronado JC. Características materno perinatales de gestantes COVID-19 en un hospital nacional de Lima, Perú. Rev Peru Ginecol Obstet. 2020;66(2):1-6. DOI: https://doi.org/10.31403/rpgo.v66i2245 [ Links ]
3. Ministerio de Salud. Alerta epidemiológica N°15 Código: AE-015-2020. "Alerta Epidemiológica ante la transmisión de COVID-19 en el Perú", 13 de marzo del 2020. https://cdn. www.gob.pe/uploads/document/file/582356/AE015.pdf [ Links ]
4. Ministerio de Salud. R. M. N° 448-2020-MINSA. "Lineamientos para la Vigilancia, Prevención y Control de la salud de los trabajadores con riesgo de exposición a COVID-19", 30 de junio del 2020. https://cdn.www.gob.pe/uploads/document/ file/903763/RM_448-2020-MINSA.pdf [ Links ]
5. Ministerio de Salud. R. M. N° 139-2020-MINSA. "Documento técnico: Prevención y atención de personas afectadas por COVID-19 en el Perú", 29 de marzo del 2020. https://cdn.www.gob.pe/uploads/document/file/574295/resolucion-ministerial-139-2020-MINSA.PDF [ Links ]
6. Paiva KJ, Grisson RD, Chan PA, Lonks JR, King E, Huard RC, et al. Validation and performance comparison of three SARS-CoV-2 antibody assays [published online ahead of print, 2020 Jul 25]. J Med Virol. 2020;10.1002/jmv.26341. doi:10.1002/jmv.26341 [ Links ]
7. Vidal-Anzardo M, Solis G, Solari L, Minaya G, Ayala-Quintanilla B, Astete-Cornejo J, Luque-Aguilar A, Jorge A, Rojas N, Cardenas F, Soto A. Evaluación en condiciones de campo de una prueba rápida para detección de anticuerpos IgM e IgG contra SARS-CoV-2. Rev Peru Med Exp Salud Publica. 2020;37(2). doi: 10.17843/rpmesp.2020.372.5534 [ Links ]
8. Guan WJ, Ni ZY, Hu Y, Liang W-h, Ou C-q, He J-x, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708-20. doi:10.1056/NEJMoa2002032 [ Links ]
9. Sutton D, Fuchs K, D'Alton M, Goffman D. Universal screening for SARS-CoV-2 in women admitted for delivery. N Engl J Med. 2020;382(22):2163-4. doi:10.1056/NEJMc2009316 [ Links ]
10. Khalil A, Hill R, Ladhani S, Pattisson K, O'Brien P. Severe acute respiratory syndrome coronavirus 2 in pregnancy: symptomatic pregnant women are only the tip of the iceberg. Am J Obstet Gynecol. 2020;223(2):296-7. doi:10.1016/j.ajog.2020.05.005 [ Links ]
11. Capobianco G, Saderi L, Aliberti S, Mondoni M, Piana A, Dessole F, et al. COVID-19 in pregnant women: A systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2020;S0301-2115(20)30446-2. doi:10.1016/j.ejogrb.2020.07.006 [ Links ]
12. Crovetto F, Crispi F, Llurba E, Figueras F, Gómez-Roig MD, Gratacós E. Seroprevalence and presentation of SARS-CoV-2 in pregnancy. Lancet. 2020 Aug 6. doi: 10.1016/S0140-6736(20)31714-1 [ Links ]
13. Khalil A, Kalafat E, Benlioglu C, O'Brien P, Morris E, et al. SARS-CoV-2 infection in pregnancy: A systematic review and meta-analysis of clinical features and pregnancy outcomes. EClinicalMedicine. 2020 Jul 3: 100446.doi: 10.1016/j.eclinm.2020.100446 [ Links ]
14. Pereira A, Cruz-Melguizo S, Adrien M, Fuentes L, Marin E, Perez-Medina T. Clinical course of coronavirus disease-2019 in pregnancy. Acta Obstet Gynecol Scand. 2020;99(7):83947. doi:10.1111/aogs.13921 [ Links ]
15. Martínez-Perez O, Vouga M, Cruz Melguizo M, Acebal LF,m Panchaud A, Muñoz-Chápuli M, Baud D. Association between mode of delivery among pregnant women with COVID-19 and maternal and neonatal outcomes in Spain. JAMA. 2020 Jun 8;e2010125. doi: 10.1001/jama.2020.10125 [ Links ]
16. Pettirosso E, Giles M, Cole S, Rees M. COVID-19 and pregnancy: A review of clinical characteristics, obstetric outcomes and vertical transmission [published online ahead of print, 2020 Aug 10]. Aust N Z J Obstet Gynaecol. 2020;10.1111/ajo.13204. doi:10.1111/ajo.13204 [ Links ]
17. Yan J, Guo J, Fan C, Juan J, Yu X, Li J, et al. Coronavirus disease 2019 in pregnant women: a report based on 116 cases. Am J Obstet Gynecol. 2020;223(1):111.e1-111.e14. doi:10.1016/j.ajog.2020.04.014 [ Links ]
18. Turan O, Hakim A, Dashraath P, Jeslyn WJL, Wright A, Abdul Kadir R. Clinical characteristics, prognostic factors, and maternal and neonatal outcomes of SARS-CoV-2 infection among hospitalized pregnant women: a systematic review. Int J Gynecol Obstet. 2020 Jul 24. doi:10.1002/ijgo.13329 [ Links ]
19. Hessami K, Homayoon N, Hashemi A, Vafaei H, Kasraeian M, Asadi N. COVID-19 and maternal, fetal and neonatal mortality: a systematic review [published online ahead of print, 2020 Aug 16]. J Matern Fetal Neonatal Med. 2020;1-6. doi:10.1080/14767058.2020.1806817 [ Links ]
20. Wang C, Zhou YH, Yang HX, Poon LC. Intrauterine vertical transmission of SARS-CoV-2: what we know so far. Ultrasound Obstet Gynecol. 2020;55(6):724-5. doi:10.1002/uog.22045 [ Links ]
21. Vivanti AJ, Vauloup-Fellous C, Prevot S, Zupan V, Suffee C, Do Cao J, et al. Transplacental transmission of SARS-CoV-2 infection. Nat Commun. 2020;11(1):3572. Published 2020 Jul 14. doi:10.1038/s41467-020-17436-6 [ Links ]
22. Khalil A, Von Dadelszen P, Draycott T, Ugwumadu A, O'Brien P, Magee L. Change in the Incidence of stillbirth and preterm delivery during the COVID-19 pandemic. JAMA. 2020 Jul 10. doi:10.1001/jama.2020.12746 [ Links ]
5The content of this article is original and has not been sent to another biomedical journal. The present study has been approved by the Institute of Health Technology Assessment and Research (IETSI) and had the authorization of the Department of Obstetrics and Gynecology.
Received: August 18, 2020; Accepted: September 16, 2020











 text in
text in