Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Ginecología y Obstetricia
On-line version ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.66 no.3 Lima Jul-Sep 2020
http://dx.doi.org/10.31403/rpgo.v66i2277
Systematic Review
Pregnant women with coronavirus disease 2019 and intrauterine vertical transmission: a systematic review
1. Faculty of Human Medicine, Universidad Privada Antenor Orrego, Trujillo, Perú
Introduction:
Coronavirus disease 2019, also called COVID-19, is a potentially severe respiratory disease originated by the type 2 coronavirus that causes severe acute respiratory syndrome (SARS-CoV-2). Intrauterine transmission from mother to fetus is a matter of debate.
Objective:
To identify the available evidence of vertical intrauterine transmission in pregnant women with COVID-19.
Methodology:
A systematic review was performed using the terms: "Vertical transmission" AND "COVID-19" OR "SARSCoV-2" NOT "Review *". The databases consulted were MEDLINE/PubMed, Science Direct, Clinical Key, LILACS, SciELO, Google Scholar, medRxiv and SciELO Preprints.
Results:
Thirty primary studies met the selection criteria and included 476 pregnant women. Infection was found in 9 neonates (1.9%) in whom pharyngeal swabs were done within 48 hours of birth. In four of them the presence of the virus was not looked for in other maternal tissues and fluids; in the remaining 5 cases, the virus RNA was identified in the placenta of three of them, in two it was found in the amniotic fluid and in one in vaginal secretion. Studies were very heterogeneous, with great variety of the reported population, the number of samples and time of collection in neonates, the lack of sampling in maternal tissues and fluids.
Conclusions:
Vertical intrauterine transmission of SARS-CoV-2 has not been conclusively demonstrated in pregnant women with COVID-19 as the majority of patients with the disease had newborns with negative molecular test (98,1%). The heterogeneity of the studies does not allow to rule out this possibility either.
Key words: Coronavirus infections; Vertical infectious disease transmission; COVID-19; SARS-CoV-2
Introduction
Coronavirus disease 2019 or COVID-19 is a potentially serious airway disease. This disease is originated by the type 2 coronavirus that causes SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2)1.
COVID-19 was first described in late December 2019 in Wuhan Province in the People's Republic of China. From that moment on, SARS-CoV-2 infection spread rapidly to other countries in Asia, Europe and the Americas, with the first case detected in Peru on March 5, 2020. On March 11, the World Health Organization (WHO) officially declared COVID-19 a pandemic2. As of August 30 this year, more than 200 countries had reported a total of 25 057 670 confirmed cases and about 842 915 deaths; these figures will continue to rise and are updated in real time on the website of the Coronavirus Resource Center of Johns Hopkins University available at: https://coronavirus.jhu.edu/map.html
According to the WHO, this virus is transmitted by direct contact with respiratory droplets expelled by infected people when they cough, speak or exhale. It can also be transmitted by indirect contact when the droplets exhaled by the sick person adhere to different objects and surfaces, which are transmitted when a healthy person touches these surfaces and then touches the mucous membrane of the eyes, nose or mouth2.
The predominant clinical picture is respiratory, which can range from mild compromise in 85% of cases due to involvement of the upper airways (similar to a common cold) to severe and fatal in 5% when it affects the lower airways (complicated pneumonia with acute respiratory distress syndrome -ARDS -and single or multiple organ failure). Other organs or tissues that may also be affected by SARS-CoV-2 include the cardiovascular, neurological, gastrointestinal, and dermatological systems. The lethality can be up to 5% depending on the population group studied. Factors associated with higher lethality include older age, especially from 60 to more years, presence of comorbidities such as high blood pressure, diabetes mellitus, chronic lung disease, obesity, and states of immunosuppression1.
The diagnosis of COVID-19 is confirmed in an asymptomatic or symptomatic person with a positive result on one of the molecular or genomic tests that detect SARS CoV-2, such as the reverse transcription polymerase chain reaction (RT-PCR)3.
To date, there is no specific pharmacological treatment to prevent or cure COVID-19, so management of infected patients is symptomatic or through supportive measures, according to the severity of the disease3.
As the number of infected people increased worldwide, confirmed cases of pregnant women with COVID-19 appeared. Some studies have reported that infected pregnant women do not usually progress to very severe cases. Symptoms are characterized by the presence of fever that is followed by respiratory symptoms such as dry cough, dyspnea, fatigue and / or myalgia and, to a lesser extent, gastrointestinal symptoms such as diarrhea. At present it is not clear whether the lung condition or pattern of pneumonia in infected pregnant women differs from that in the general population4.
It is well documented, and based on evidence, that transmission of SARS-CoV-19 from human to human is through the airway, although the presence of SARS-CoV-2 has also been found in other fluids and secretions such as blood, feces, cerebrospinal fluid, saliva, tears, semen, and conjunctival secretions. This has led some authors to raise the possibility of fecal-oral transmission1,5.
There are some reports of altered perinatal outcomes in pregnant women with COVID-19 depending on the trimester when the infection occurred, including miscarriages and preterm deliveries, but in no case was the transmission of the infection from mother to child demonstrated5.
The vertical intrauterine transmission of COVID-19 remains controversial. Abarzúa6 mentioned that cases of this potential transmission route continue to be reported, such as in China where a newborn born by cesarean section from a mother with confirmed COVID-19 pneumonia tested positive for SARS-CoV-2 in the pharyngeal swab study. Unfortunately, there were no studies in samples of amniotic fluid, cord blood, placenta or breast milk, which could have clarified the hypothesis about the time of transmission, whether it occurred before delivery or postpartum.
To date, doubts remain about the possibility of vertical intrauterine transmission from the mother with COVID-19 to the product of gestation, so it is necessary to review and analyze the information available. Therefore, a systematic review was carried out to determine if there is scientific evidence of vertical intrauterine transmission in the pregnant woman with COVID-19.
Methods
A systematic search of primary studies was done from June 26 to July 30, 2020 using MeSH terms (Medical Subject Headings) in free data-bases and two preprint repositories, the latter in order to decrease selection bias. Case reports, case series, case-control and cohort studies of pregnant women and neonates with diagnosis of COVID-19 confirmed by molecular test were included. The studies were published in English, Spanish, or Portuguese between December 31, 2019 and July 15, 2020. Duplicate primary papers were excluded, selecting the most updated and of the best scientific quality, COVID-19 cases confirmed by non-molecular tests, and cases of non-intrauterine vertical transmission.
To maximize sensitivity, a search strategy was carried out through databases of international publications: MEDLINE/PubMed, Science Direct, Clinical Key, LILACS, SciELO and Google Scholar; and medical preprints repository: medRxiv and SciELO Preprints. The search was carried out on the title and abstract of the selected database with the following MeSH terms: "Vertical transmission" AND "COVID-19" OR "SARS-CoV-2" NOT "Review*" OR "Meta-Analysis". The PRISMA guide was followed and registered in the PROSPERO database (registration code: CRD42020193798).
The articles were identified, screened, reviewed, selected and analyzed by the researchers. In case of any disagreement about any article or content of this, it was decided to accept it by simple majority with the support and guidance from the more experienced researcher. The data collected were: bibliographic source, type of study, pregnant woman’s age, weeks of gestation (trimester of pregnancy), pregnant woman’s symptoms, pharmacological treatment of the pregnant woman, type of delivery, sex of the newborn, age of COVID-19 diagnosis in the newborn, symptoms in the newborn and presence or absence of SARS-Cov-2 in tissues or fluids related to vertical intrauterine transmission (for example, amniotic fluid and/or membrane, umbilical cord and placenta). If the article was a case report, data were extracted on an individual basis. If the article was a case series, case-control or cohort, the mean was calculated for quantitative variables and the proportion of the total for qualitative variables, in addition to ranges according to data availability.
The primary outcome was the presence or absence of neonatal COVID-19 confirmed by molecular method, due to vertical intrauterine transmission of pregnant women with COVID-19 confirmed by molecular method.
Results
A total of 419 studies were identified from 410 (97.9%) peer review medical databases studies and 9 (2.1%) database studies of pre-published studies. Twenty duplicate articles were discard ed during the process, remaining 399 studies for screening. After reading the abstract of the screened articles, 339 studies were excluded, with 60 articles eligible for full-text review. Of these, 30 were excluded for the following reasons: 10 articles were letters to the editor, 8 articles were narrative reviews and 12 articles were systematic reviews. Finally, 30 articles (736) were included in the analysis, synthesis and presentation (Figure 1).
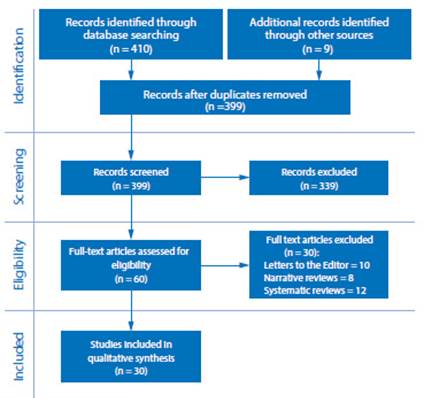
Figure 1 Flow chart oF the selection process oF included studies to evaluate the vertical intrauterine transmissibility in pregnant women with coronavirus 2019 disease according to the prisma guide.
The 30 articles included reported 476 cases of pregnant women with confirmed diagnosis of COVID-19 with their respective neonates (477 due to a twin pregnancy). Thirteen studies were case reports (13 patients), 7 observational studies (190 patients), 7 case series (144 patients), and 3 cohort studies (129 patients), as shown in Table 1.
Table 1 Summary and characteristics of primary studies analyzed to evaluate the intrauterine vertical transmiss ibility of pregnant women with coronavirus 2019 disease.
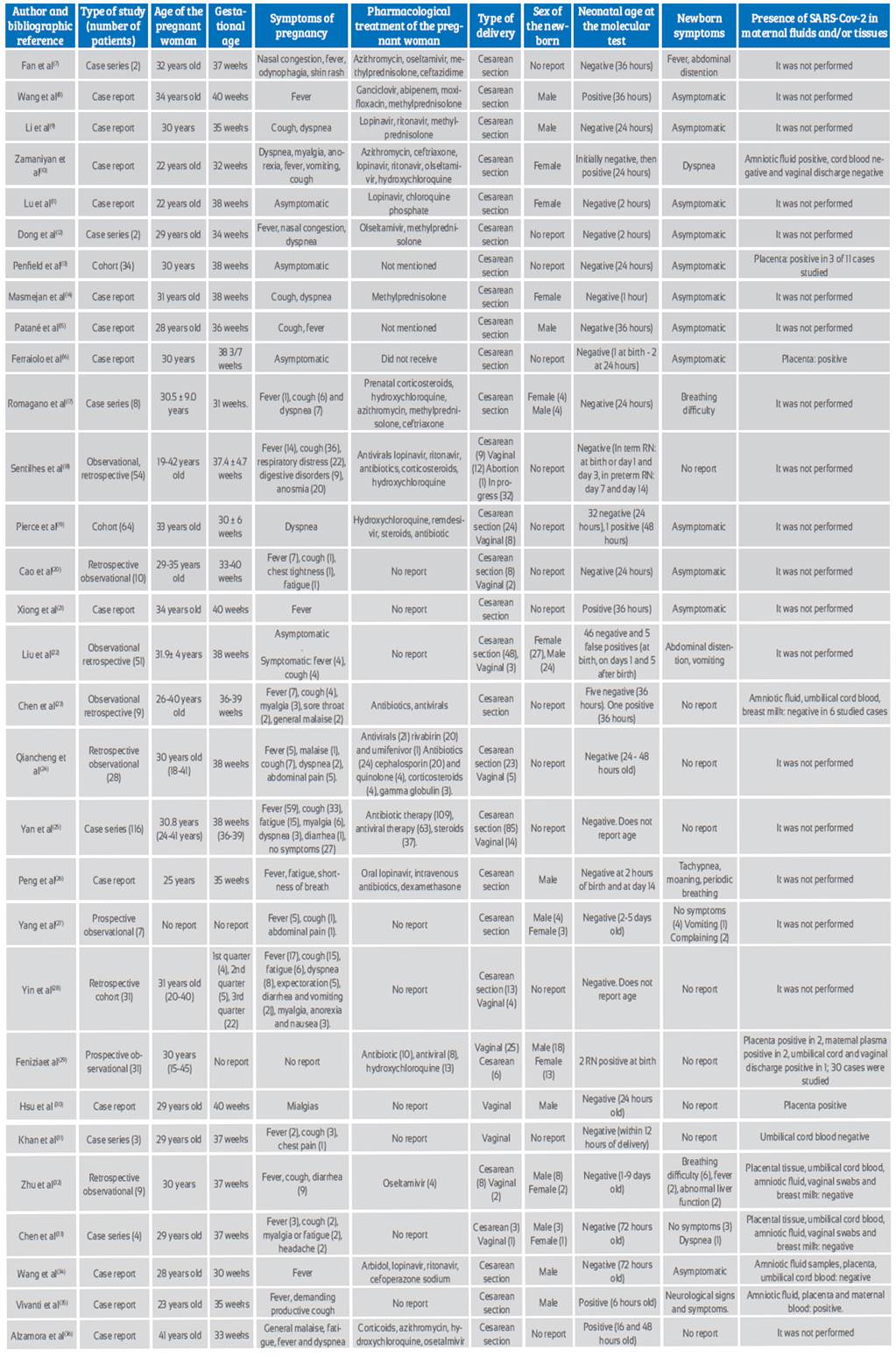
The maternal age range fluctuated between 15 and 45 years. Most cases occurred during the third trimester of pregnancy. The most prevalent maternal symptoms of infection were: fever in 143 cases (30% of cases), cough in 127 cases (26.7%), dyspnea in 29 (6.1%), fatigue in 25 (5.3%), myalgias in 13 (2.7%), and digestive disorders in 11 cases (2.3%), among other symptoms. Asymptomatic pregnant women were 32 (6.7% of cases).
Among the drugs indicated for pregnant women were antivirals, antibiotics, corticosteroids and hydroxychloroquine. The term of pregnancy in most patients was by cesarean section, and only 78 vaginal deliveries (16.4%) were reported.
In 46% of the studies reviewed, the sex of the newborns was not reported, but in the remaining 54%, 68 were males and 53 females. The neonatal age at which the molecular test for the diagnosis of COVID-19 was performed fluctuated between the moment of birth and the 14th day of birth.
In 8 of the 30 included studies(8,10,19,21,23,29,35,36), a total of 9 confirmed positive newborns were reported. In 19 studies of the total, none of the infants showed symptoms of COVID-19 and the remaining 11 studies described various symptoms including tachypnea, fever, vomiting, abdominal distention, liver dysfunction, and neurological symptoms/signs.
In 19 studies, the presence of molecular SARSCoV- 2 in tissues and fluids related to vertical intrauterine transmission was not investigated; in the remaining 11 studies(10,13,16,23,29-35) the virus was found in 7 of 19 placentas studied, and only in 3 of these 7 placentas there was coexistence of neonatal COVID-19. The virus was identified in 2 out of 8 amniotic fluid samples, and in cases of virus-positive placenta it coexisted with neonatal COVID-19. SARS-CoV-2 was identified in 2 out of 9 umbilical cord blood samples and in those cases, there was coexistence with neonatal COVID- 19; vaginal mucosa and maternal blood or plasma were also studied.
Discussion
Despite the time that has elapsed and the increasing number of cases of the disease in pregnant women and the reported cases of probable vertical intrauterine transmission of the disease, this mechanism of transmissibility is still in doubt1-5.
The objective of this study was to determine if there is scientific evidence of vertical intrauterine transmission in the pregnant woman with COVID-19.
Despite the fact that most cases of pregnant women with COVID-19 have completed their gestation with neonates without confirmed COVID-19 (98.1% or 468 of 477 cases), it is important to take into account some aspects that may condition this result.
Molecular test (RT-PCR) confirms the presence of SARS-CoV-2 and therefore COVID-19, even in asymptomatic patients1-4. Unfortunately, its accuracy is not 100%, it has high specificity and moderate sensitivity. Despite this, it is considered the gold standard for the moment37-39. On the other hand, the sensitivity of this test depends on the method and anatomical location for taking the sample as well as the time of evolution of the disease37-39. For example, if the neonatal swab is done too early or late, the sensitivity may be lower than desired. Therefore, in doubt about the exact moment of the hypothetical neonatal intrauterine infection, the best thing would be to take the sample serially.
Our review found that in 16 studies only one swab was taken and it was within 36 hours of birth and in 2 studies at 72 hours; in 10 studies serial swabs were taken and in the remaining 2 the time of swab taking was not specified. Of the 9 neonates found with positive RT-PCR, two were sampled at birth29, one at 6 hours35, one at 16 hours36, one at 24 hours10, three at 36 hours8,21,23, and one at 48 hours19 after birth. These findings would show us how relative it can be to use a single sampling as a diagnostic method to demonstrate or rule out vertical transmission.
Wang S et al8 mention that vertical transmission after primary maternal infection can usually occur during intrauterine life through the transplacental route or during delivery by ingestion or aspiration of cervicovaginal secretions, it is for this last reason that it is decided to terminate the pregnancy by cesarean section, which was evident in most of the articles reviewed except articles18-20,22,24,25,28-31) for ten where delivery was by the vaginal route. Six neonates positive for COVID-19 were delivered by cesarean section8,10,21,23,35,36 and in the remaining three the delivery route was not specified19,29. These results do not allow us to recommend a specific route for the termination of pregnancy to prevent infection in the neonate.
As previously mentioned, the controversial results of the identification of viral RNA in the different maternal tissues and fluids keep the intrauterine transmission mechanism in doubt. To date, reports of SARS-CoV-2 in maternal tissues and fluids have increased. If the virus is found in the placenta, amniotic fluid, or vaginal canal, introduction of this through the neonatal airway would be likely, even if there is no aerosolization. And if we add the duration of fetal exposure to those tissues and fluids, it could be equivalent to exposure to an environmental viral load. The viral RNA was identified in 8 of 14 amniotic fluid samples studied10,23,32-35; the neonate was COVID-19 positive in two cases; it was identified in 7 of 19 placentas13,16,29,30,32-35 of which three were COVID-19 positive neonates. SARS-CoV-2 was found in a sample of maternal blood or plasma29,35 and it was associated with two COVID-19 positive neonates. In the remaining three positive neonates8,19,36, the presence of the virus in other maternal tissues or body fluids was not investigated. In some studies, SARS-CoV-2 was looked for in tissues and/or fluids of mothers with COVID-19, and results were negative, as described by some authors23,31-34.
Despite there being a greater report of probable cases of vertical intrauterine transmission of COVID-19 compared to previous reviews40-47, the presence of several factors in the different studies does not allow for definitive conclusions. Among these factors, we can mention the heterogeneity of the reported population (maternal age, gestational age, treatment for COVID-19 received, way of ending the pregnancy), as well as the number of samples and time of collection in the neonates, the lack of sampling of maternal tissues and fluids in most cases.
Among the limitations of this review, it is considered that no studies in other languages and no manuscripts such as letters to the editor were included, and there was a lack of accessibility to all virtual and written databases available.
Conslussion
Vertical intrauterine transmission of SARS-CoV-2 has not been conclusively demonstrated in the pregnant woman with COVID-19 because most patients with the disease have not had neonates with a positive molecular test (98.3%). However, the heterogeneity of the studies does not allow ruling out this possibility either in cases where maternal and fetal factors converge. Future more complete and homogeneous studies may shed light on our doubts.
REFERENCES
1. Pacheco-Romero J. La incógnita del nuevo coronavirus, la gestante y su niño. Lo que el ginecobstetra está conociendo. Rev Peru Ginecol Obstet. 2020;66(1). Publicación anticipada. doi: 10.31403/rpgo.v66i2247 [ Links ]
2. Noguera M, Santos M, Monsalve N, Avendaño J, Avendaño-Noguera J. COVID-19 por SARS-CoV-2: la nueva emergencia de salud en la embarazada. Lo que los médicos y obstetras necesitan saber. Revista GICOS. 2020-5(e1):83-101. [ Links ]
3. Ortiz EI, Herrera E, De La Torre A. Infección por corona-virus (COVID-19) en el embarazo. Colombia Med (Cali). 2020;51(2):1-7. doi: 10.25100/cm.v51i2.4271 [ Links ]
4. Vigil-De Gracia P, Caballero LC, Ng Chinkee J, Luo C, Sánchez J, Quintero A y col. COVID-19 y embarazo. Revisión y actualización. Rev Peru Ginecol Obstet. 2020;66(2). publicación anticipada. doi: 10.31403/rpgo.v66i2248 [ Links ]
5. Alonso V. Coronavirus: ¿qué hacer en la población gestante? Arch Ginecol Obstet. 2020;58(1):9-17 [ Links ]
6. Arbazúa Camus F. COVID-19 y embarazo. Rev Chil Obstet Ginecol. 2020;85(2):110-4. [ Links ]
7. Fan C, Lei D, Fang C, Li C, Wang M, Liu Y, et al. Perinatal transmission of COVID-19 associated SARS-CoV-2: Should we worry? Clin Infect Dis. 2020 Mar 17:ciaa226. doi: 10.1093/cid/ciaa226 [ Links ]
8. Wang S, Guo L, Chen L, Liu W, Cao Y, Zhang J, Feng L. A case report of neonatal COVID-19 infection in China. Clin Infect Dis. 2020 Mar 12:ciaa225. doi: 10.1093/cid/ciaa225 [ Links ]
9. Li Y, Zhao R, Zheng S, Chen X, Wang J, Sheng X, et al. Lack of vertical transmission of severe acute respiratory syndrome coronavirus 2, China. Emerg Infect Dis. 2020 Jun;26(6):13356. doi: 10.3201/eid2606.200287 [ Links ]
10. Zamaniyan M, Ebadi A, Aghajanpoor S, Rahmani Z, Haghshenas M, Azizi S. Preterm delivery, maternal death, and vertical transmission in a pregnant woman with COVID-19 infection. Prenat Diagn. 2020 Apr 17:10. doi: 10.1002/pd.5713 [ Links ]
11. Lu D, Sang L, Du S, Li T, Chang Y, Yang XA. Asymptomatic COVID-19 infection in late pregnancy indicated no vertical transmission. J Med Virol. 2020 Apr 24. doi: 10.1002/jmv.25927 [ Links ]
12. Dong L, Tian J, He S, Zhu C, Wang J, Liu C, Yang J. Possible vertical transmission of SARS-CoV-2 from an infected mother to her newborn. JAMA. 2020 Mar 26;323(18):1846-8. doi: 10.1001/jama.2020.4621 [ Links ]
13. Penfield CA, Brubaker SG, Limaye MA, Lighter J, Ratner AJ, Thomas KM, Meyer J, Roman AS. Detection of SARS-COV-2 in placental and fetal membrane samples. Am J Obstet Gynecol MFM. 2020 May 8:100133. doi: 10.1016/j.ajogmf.2020.100133 [ Links ]
14. Masmejan S, Pomar L, Favre G, Panchaud A, Giannoni E, Greub G, Baud D. Vertical transmission and materno-fetal outcomes in 13 patients with COVID-19. Clin Microbiol Infect. 2020 Jul 8:S1198 743X(20)30381-5. doi: 10.1016/j.cmi.2020.06.035 [ Links ]
15. Patanè L, Morotti D, Giunta MR, Sigismondi C, Piccoli MG, Frigerio L, et al. Vertical transmission of COVID-19: SARSCoV-2 RNA on the fetal side of the placenta in pregnancies with COVID-19 positive mothers and neonates at birth. Am J Obstet Gynecol MFM. 2020 May 18:100145. doi: 10.1016/j.ajogmf.2020.100145 [ Links ]
16. Ferraiolo A, Barra F, Kratochwila C, Paudice M, Vellone VG, Godano E, et al. report of positive placental swabs for sarscov-2 in an asymptomatic pregnant woman with COVID-19. Medicina (Kaunas). 2020 Jun 22;56(6):E306. doi: 10.3390/medicina56060306 [ Links ]
17. Romagano MP, Guerrero K, Spillane N, Kayaalp E, Smilen SW, et al. Perinatal outcomes in critically ill pregnant women with coronavirus disease 2019. AJOG MFM, 2020, 100151, ISSN 2589-9333. doi: 10.1016/j.ajogmf.2020.100151 [ Links ]
18. Sentilhes L, De Marcillac F, Jouf-frieau C, Kuhn P, Thuet V, Hansmann Y, et al. Coronavirus disease 2019 in pregnancy was associated with maternal morbidity and preterm birth. Am J Obstet Gynecol 2020 Jun 15. doi: 10.1016/j.ajog.2020.06.022 [ Links ]
19. Pierce-Williams RAM, Burd J, Felder L, Khoury R, Bernstein PS, Avila K, et al. Clinical course of severe and critical coronavirus disease 2019 in hospitalized pregnancies: A United States cohort study. Am J Obstet Gynecol MFM. 2020 Aug;2(3):100134. doi: 10.1016/j.ajogmf.2020.100134 [ Links ]
20. Cao D, Yin H, Chen J, Tang F, Peng M, Li R, et al. Clinical analysis of ten pregnant women with COVID-19 in Wuhan, China: A retrospective study. Int J Infect Dis. 2020;95:294300. doi: 10.1016/j.ijid.2020.04.047 [ Links ]
21. Xiong Y, Zhang Q, Zhao L, Shao J, Zhu W. Clinical and imaging features of COVID-19 in a neonate. Chest. 2020;158(1):e5e7. doi: 10.1016/j.chest.2020.03.018 [ Links ]
22. Liu P, Zheng J, Yang P, Wang X, Wei C, Zhang S, et al. The immunologic status of newborns born to SARS-CoV-2-infected mothers in Wuhan, China. J Allergy Clin Immunol. 2020;146(1):101-9. doi: 10.1016/j.jaci.2020.04.038 [ Links ]
23. Chen H, Guo J, Wang C, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020 Feb 12;395(10226):809-15. doi:10.1016/S0140-6736(20)30360-3 [ Links ]
24. Qiancheng X, Jian S, Lingling P, Lei H, Xiaogan J, Weihua L, Gang Y, Shirong L, Zhen W, GuoPing X, Lei Z; sixth batch of Anhui medical team aiding Wuhan for COVID-19. Coronavirus disease 2019 in pregnancy. Int J Infect Dis. 2020;95:376383. doi: 10.1016/j.ijid.2020.04.065 [ Links ]
25. Yan J, Guo J, Fan C, Juan J, Yu X, Li J, et al. Coronavirus disease 2019 in pregnant women: a report based on 116 cases. Am J Obstet Gynecol. 2020;223(1):111.e1-e14. doi: 10.1016/j.ajog.2020.04.014 [ Links ]
26. Peng Z, Wang J, Mo Y, Duan W, Xiang G, Yi M, Bao L, Shi Y. Unlikely SARS-CoV-2 vertical transmission from mother to child: A case report. J Infect Public Health. 2020;13(5):81820. doi: 10.1016/j.jiph.2020.04.004 [ Links ]
27. Yang P, Wang X, Liu P, Wei C, He B, Zheng J, Zhao D. Clinical characteristics and risk assessment of newborns born to mothers with COVID-19. J Clin Virol. 2020;127:104356 doi: 10.1016/j.jcv.2020.104356 [ Links ]
28. Yin M, Zhang L, Deng G, Han C, Shen M, Sun H, et al. Severe acute respiratory syndrome coronavirus 2 (SARSCoV-2) infection during pregnancy in China: A retrospective cohort study [Internet]. Respiratory Med. 2020 abr [cited 12 de julio de 2020]. Doi:10.1101/2020.04.07.20053744 [ Links ]
29. Fenizia C, Biasin M, Cetin I, Vergani P, Mileto D, Spinillo A, et al. In-utero mother-to-child SARS-CoV-2 transmission: viral detection and fetal immune response. Obstet Gynecol. 12 July 2020. DOI: 10.21203/rs.3.rs-45729/v1 [ Links ]
30. Hsu AL, Guan M, Johannesen E, Stephens AJ, Khaleel N, et al. Placental SARS-CoV-2 in a patient with mild COVID-19 disease [Internet]. medRxiv. Cited 17 July 2020]. doi: 10.1101/2020.07.11.20149344 [ Links ]
31. Khan S, Peng L, Siddique R, Nabi G, Nawsherwan, Xue M, Liu J, Han G. Impact of COVID-19 infection on pregnancy outcomes and the risk of maternal-to-neonatal intrapartum transmission of COVID-19 during natural birth. Infection Control & Hospital Epidemiology, 2020;41:748-50. doi: 10.1017/ice.2020.84 [ Links ]
32. Zhu H, Wang L, Fang C, Peng S, Zhang L, Chang G, Xia S, Zhou W. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl Pediatr. 2020;9(1):51-60. doi: 10.21037/tp.2020.02.06 [ Links ]
33. Chen Y, Peng H, Wang L, Zhao Y, Zeng L, Gao H, Liu Y. Infants born to mothers with a new coronavirus (COVID-19). Front Pediatr. 2020;8:104. doi: 10.3389/fped.2020.00104 [ Links ]
34. Wang X, Zhou Z, Zhang J, Zhu F, Tang Y, Shen X, et al. A case of 2019 novel coronavirus in a pregnant woman with preterm delivery. Clin Infect Dis. 2020;71(15):844-6. doi: 10.1093/cid/ciaa200 [ Links ]
35. Vivanti AJ, Vauloup-Fellous C, Prevot S, Zupan V, Suffee C, Cao JD et al. Transplacental transmission of SARS-CoV-2 infection. Nat Commun. 2020;11(1):3572. doi: 10.1038/s41467-020-17436-6 [ Links ]
36. Alzamora MC, Paredes T, Caceres D, Webb CM, Valdez LM, La Rosa M. Severe COVID-19 during pregnancy and possible vertical transmission. Am J Perinatol. 2020;37(8):861-5. doi: 10.1055/s-0040-1710050 [ Links ]
37. Watson J, Penny F, Brush JE. Interpreting a covid-19 test result. BMJ. 2020;369:m1808. doi: 10.1136/bmj.m1808 [ Links ]
38. La Marca A, Capuzzo M, Paglia T, Roli L, Trenti T, Nelson SM. Testing for SARS-CoV-2 (COVID-19): a systematic review and clinical guide to molecular and serological in-vitro diagnostic assays. Reprod Biomed Online. 2020. doi: 10.1016/j.rbmo.2020.06.001 [ Links ]
39. Tahamtana A, Ardebilib A. Real-time RT-PCR in COVID-19 detection: issues affecting the results. Expert Review Molecular Diagnostics. 2020. Doi:10.1080/14737159.2020.1757437 [ Links ]
40. Zimmermann P, Curtis N. COVID-19 in children, pregnancy and neonates: A review of epidemiologic and clinical features. Pediatr Infect Dis J. 2020;39(6):469-77. doi: 10.1097/INF.0000000000002700 [ Links ]
41. Instituto de Evaluación de Tecnologías en Salud e Investigación. Transmisión SARS-CoV-2 madre-feto: síntesis rápida de evidencia. Marzo-2020. Lima: ESSALUD; 2020. http://www.essalud.gob.pe/ietsi/pdfs/direcc_invest_salud/RRI_05_2020_ V3.pdf [ Links ]
42. Karimi-Zarchi M, Neamatzadeh H, Dastgheib SA, Abbasi H, Mirjalili SR, Behforouz A, et al. Vertical transmission of coronavirus disease 19 (COVID-19) from infected pregnant mothers to neonates: A review. Fetal Ped Pathol. 2020;39(3):246-50. doi: 10.1080/15513815.2020.1747120 [ Links ]
43. Caparrós-González RA. Consecuencias maternas y neonatales de la infección por coronavirus COVID-19 durante el embarazo: una scoping review. Rev Esp Salud Pública. 2020;94:e1-9. https://medes.com/publication/151452 [ Links ]
44. Fornari F. Vertical transmission of Covid-19. A systematic review. J Pediatr Perinatol Child Health. 2020;4(2):7-13. doi: 10.26502/jppch.7405034 [ Links ]
45. Muhidin S, Behboodi Moghadam Z, Vizheh M. Analysis of maternal coronavirus infections and neonates born to mothers with 2019-nCoV; a systematic review. Arch Academic Emerg Med. 2020 Apr 14;8(1):e49. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7211430/pdf/aaem-8-e49.pdf [ Links ]
46. De Rose DU, Piersigilli F, Ronchetti MP, Santisi A, Bersani I, Dotta A, et al. Novel coronavirus disease (COVID-19) in newborns and infants: what we know so far. Italian J Ped. 2020;46:56. doi: 10.1186/s13052-020-0820-x [ Links ]
47. Duran P, Berman S, Niermeyer S, Jaenisch T, Forster T, Gomez R, et al. COVID-19 and newborn health: systematic review. Rev Panam Salud Publica. 2020;44:e54. doi: 10.26633/RPSP.2020.54 [ Links ]
Received: August 30, 2020; Accepted: September 11, 2020











 text in
text in 



