Introducción
The consequences of COVID-19 infection in the world, as of August 25, 2020, is around 832 000 deaths among 23 million cases, with 103 deaths per million inhabitants and a fatality of 3.8%. Perú has a mortality of 826 deaths per million inhabitants, corresponding to a fatality of 4.8%, the highest in America at the moment1.
Global maternal mortality expressed as the world maternal death ratio in 2017 was 211/100 000 live births, the main causes being hemorrhage in 27%, preeclampsia in 14%, sepsis 11%, abortion 8%, embolism 3%, other direct causes 10% e indirect 28%2.
The majority of pregnant women with COVID-19 are asymptomatic, in 87.9%3. As for pregnant women who have symptoms, 86% have mild disease, 9.3% severe and 4.7% critical4.
The most severe complications from COVID-19 occur mostly in the third trimester of pregnancy, 4.2% suffer of pneumonia5. Obstetric complications are present in 45% (95% CI: 24.0% to 6.0%) of cases6.
With respect to women of the same age, pregnant women with COVID-19 are more likely to enter intensive care (OR=5.4 (95% CI 95%: 2,89 to 10.08) and to need mechanical ventilation, OR=4,0 (95% CI: 1.75 to 9.14)7. In addition, it is known that the greater the number of comorbidities, the greater the risk of death8. In a study in Brazil, it was found that 55% of pregnant women deaths from COVID-19 had comorbidities, 80% of deaths occurred during the puerperium, in 10% associated with preeclampsia9. In another report, 7 maternal deaths from COVID-19 also had fetal death in 42.9% of cases10. Other comorbidities found in maternal deaths are diabetes, obesity, asthma, advanced maternal age, hypothyroidism11. One death during pregnancy due to coagulopathy and basilar artery thrombosis has been described in the United Kingdom12.
The objective of this communication is to present three cases of maternal death with SARSCoV-2 IgG / IgM (+), of the 36 occurred in Peru, treated at the Cajamarca Regional Teaching Hospital. They had severe preeclampsia and complications such as eclampsia and HELLP syndrome, with ischemic stroke, acute kidney injury, and hemorrhagic cerebrovascular disease. In addition, all had stillbirth.
Presentation of cases
Case 1: Ischemic stroke, eclampsia
A 32-year-old woman, 10-day puerperal with a 35-week stillbirth, and presenting high blood pressure and seizures, arrived from a distant health center in coma, with sepsis and pneumonia to COVID-19, As a background, she was G2 P0301 (one twin pregnancy) and had a positive contact with COVID-19 in her previous hospitalization 10 days before. She presented seizures, coma and left hemiplegia. The diagnosis was puerperal for 10 days, COVID-19 pneumonia, sepsis, right cerebral infarction, severe preeclampsia, eclampsia. The neurological diagnosis was score 20 according to the stroke score of the US Health Centers (NIH Stroke Scale- NIHSS).
The results of the laboratory tests were: reactive C protein: 96 mg/dL, complement 3: 289 mg/dL, complement 4: 90 mg/dL, sedimentation rate: 50 mm/h, SARS-CoV-2: IgG/IgM (+).
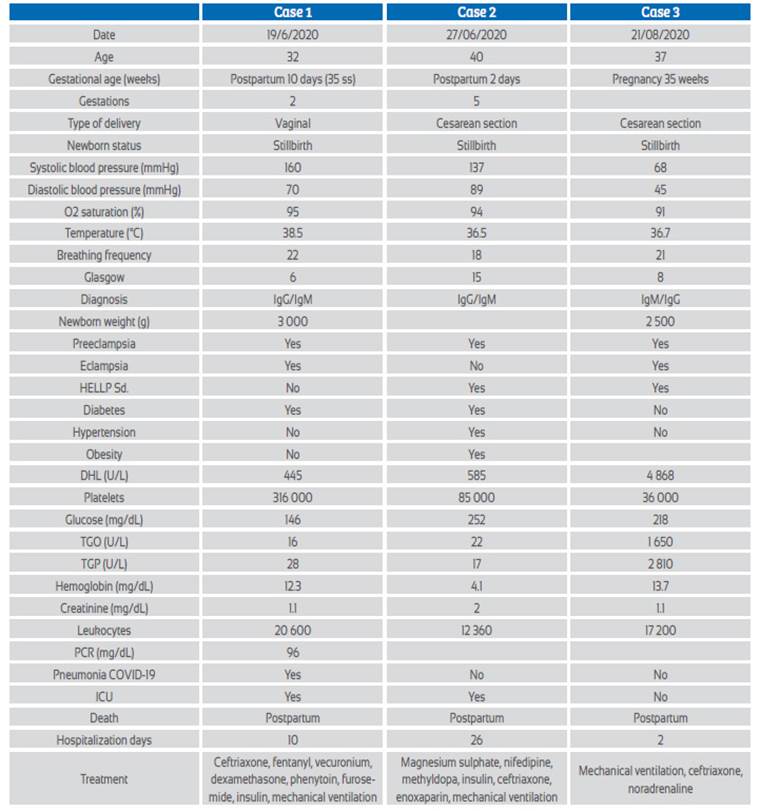
Brain multislice spiral tomography (MST) with coronal and sagittal reconstructions (Figure 1) showed extensive right cerebral infarction (in the middle cerebral artery (MCA) and the anterior cerebral artery (ACA) territory, with a large mass effect, conditioning deviation of the midline by 14 mm to the left and partial collapse of the supratentorial ventricles. Increase density of the MCA was evidenced, probably related to thrombus (Alberta Stroke Program Early CT Score (ASPECTS):0). Chest MST with coronal and sagittal reconstructions showed typical signs of Covid-19 ("ground glass", vascular thickening, cobblestone pattern, parenchymal bands and bilateral consolidations predominantly left). CORADS: 513.
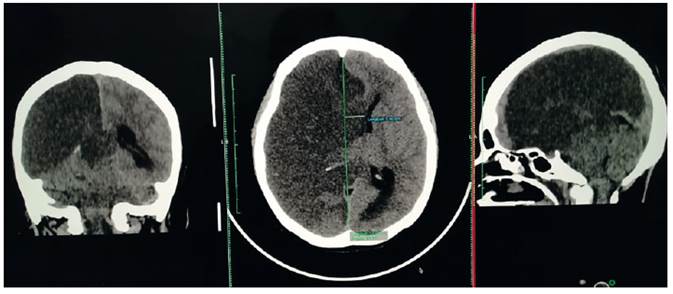
Figure 1 Case 1. Brain tomography without contrast (with coronal and sagittal reconstruction): extensive rigth cerebral infarction (in the territory of the middle cerebral artery (MCA) and anterior cerebral artery (ACA)), with a large mass effect, conditioning a deviation of the midline by 14 mm to the left and partial collapse of the supratentorial ventricles. Increased MCA density is evidenced, probably related to thrombus (Alberta Stroke Program Early CT Score (ASPECTS ):0).
Treatment (see Table) included mechanical ventilation. During evolution, she presented seizures, auricular flutter, septic shock, kidney injury and died.
Case 2: Comorbidities, hellp syndrome, acute kidney injury
The case was a 40-year-old woman two days after a cesarean section in another hospital for severe preeclampsia, stillbirth and COVID-19, with a history of diabetes, obesity, high blood pressure, and HELLP syndrome, G5P3021. She complained of abdominal pain.
The diagnosis was two days post cesarean section, severe preeclampsia, HELLP syndrome, obesity, diabetes, IgG/IgM (+) to SARS-CoV-2.
Laboratory tests were reported as: hemoglobin 4.9 mg/dL, platelets 77 000, glucose 400 mg/dL, creatinine 2.1 mg/dL, LDH 456 U/L, TGP 15 U/L, TGO 30 U/L. Ultrasound showed free fluid in the abdominal cavity.
Treatment included mechanical ventilation (Table 1).
In the evolution, a 4 liters hemoperitoneum was found with no apparent cause. She underwent laparotomy and exploration of the liver and spleen, but the bleeding source was not found.
She was poly-transfused, had mechanical ventilation. She improved in ICU but decompensated later and developed acute kidney injury, anasarca, and pulmonary edema.
Case 3: Eclampsia, Cardiorespiratory arrest, hemorrhagic cerebrovascular disease, hellp syndrome
A 37-year-old female patient was admitted without prenatal control, with history of severe headache, abdominal pain, loss of consciousness and seizures. The 35-week pregnant woman was diagnosed of stillbirth, severe preeclampsia, HELLP syndrome, eclampsia, cerebrovascular disease (possible stroke with NIHSS 33), IgG/IgM positive to SARS-CoV-2.
Laboratory tests were: white blood count 17 200, hemoglobin 13.7 mg/dL, glucose 218 mg/dL, creatinine 1.1 mg/dL, LDH 4 704 U/L, TGO 302 U/L, total bilirubin 4.3 mg/dL (Table 1). Ultrasound showed fetal death.
Treatment consisted in cesarean section, mechanical ventilation (Table 1)
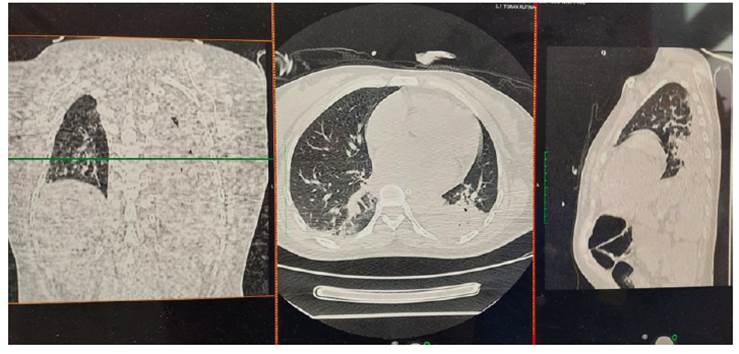
Figure 2 Case 1. Non-contrast chest tomography (with coronal and sagittal reconstruction) shows typical signs of Covid-19 - ‘ground glass’, vascular thickening, cobblestone pattern, parenchymal bands and bilateral consolidations, predominantly left. CO-RADS: 513.
During evolution she presented cardiorespiratory arrest in the emergency room, from which she recovered. She underwent a cesarean section without anesthesia, no hemoperitoneum was found. It was not possible to perform a tomography or to admit her to the intensive care unit. She died one day after cesarean section.
Discussion
Among the 36 maternal deaths in Peru due to COVID-19, we present three maternal deaths that occurred in Cajamarca, all with IgG/IgM (+) to SARS-CoV-2 and severe preeclampsia, two with eclampsia and two with HELLP syndrome. The first maternal death presented ischemic stroke (cerebral infarction). The second died of diabetes, kidney injury and pulmonary edema. The third, with eclampsia, HELLP syndrome and possible stroke. All three had a stillbirth of around 35 weeks.
One publication on maternal death in Brazil states that 10% of them were associated with preeclampsia9, which differs from our findings, where all three had severe preeclampsia with 4 Rev Peru Ginecol Obstet. 2020;66(3) eclampsia and/or HELLP syndrome. There are publications that seek criteria to differentiate the findings or HELLP syndrome and complications typical of COVID-19 with similar manifestations14.
In a systematic review of COVID-19 and pregnancy, stillbirth figures are around 45%10. We found death in the third trimester (35 weeks) in all three cases (100%).
In all three cases we have found diabetes associated morbidities in two cases, obesity in one patient, cesarean section in two, age over 35 years in two, and two women presented complications in the puerperium. These data are similar to those of a publication that shows that the more the comorbidities, the greater the risk of death11.
Neurological symptoms due to COVID-19 range from anosmia to ischemic stroke or intracerebral hemorrhage. It is reported that due to hypercoagulability up to 5.7% of patients have cerebrovascular accident and 2.8% ischemic stroke15. Of hospitalized patients with COVID-19 and neurological compromise, 77% have an ischemic component. Because the complication occurs in the great vessels, 84.2% improve with Solumbra technique mechanical thrombectomy, obtaining substantial improvement in permeabilization, with score TICI> 2B/3 (16) . In our cases, coagulopathy with ischemic stroke was found in the territory of the right anterior and middle cerebral arteries in 33.3% of cases, associated with eclampsia and pneumonia due to COVID-19 (CORADS-5). In these cases, teamwork with neurology, neurosurgery, cardiology and radiology specialists is necessary, as well as the use of NIHSS clinical and ASPECT carotid arteries Doppler, cardiac Doppler radiological scales, and adequate thrombolysis, measurable with mTICI (modified treatment in cerebral infarction score), and early decompressive craniotomy.
The limitation of this communication is the small number of cases, in a context where the ICU and patient flow charts were not yet fully implemented.
In conclusion, there is still a lack of experience in the management of pregnant women in this pandemic. We consider that, first of all, pregnant women should be considered vulnerable and continue to control them without limitations.
Second, the possibility that preeclampsia be considered a comorbidity associated with mortality from COVID-19. Third, stillbirth may be common and should be considered and prevented. Fourth, severe preeclampsia in the presence of symptomatic COVID-19 has high mortality, due to the severity of both. Fifth, brain tomography is essential in early diagnosis and would help to quickly initiate the management of postpartum women with ischemic or hemorrhagic brain involvement.