Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.66 no.3 Lima jul-sep 2020
http://dx.doi.org/10.31403/rpgo.v66i2280
Case Report
Tubal ectopic pregnancy six years after supracervical hysterectomy. A case report
31. Hospital Nacional Guillermo Almenara Irigoyen, EsSalud, Lima, Perú
2. Clínica de Prevención Larco, EsSalud, Lima, Perú
Ectopic pregnancy in hysterectomized patients is an uncommon event and it is rarely considered in the differential diagnosis. We present the case of a 30-year-old patient with hysterectomy performed 6 years before who presented to the emergency service with a 3-day evolution of lower abdominal pain. Ultrasonography showed a gestational sac with embryo and the presence of free fluid in the Douglas sac. Histological examination of the surgical piece revealed chorionic villi and an embryo within the uterine tube.
Key words: Ectopic pregnancy; post hysterectomy; Tubal pregnancy
Introduction
An ectopic pregnancy happens in 1 to 2% of pregnancies1 and is one of the main differential diagnoses in women of fertile age with abdominal pain2. This diagnosis is usually not considered when the patient has a history of hysterectomy, which postpones treatment, resulting in complications that put the patient's life at risk. Although it is a rare event, there are approximately 74 reported cases in hysterectomized patients3,4 until now, and half of them has happened years after the hysterectomy, as did the case we will describe.
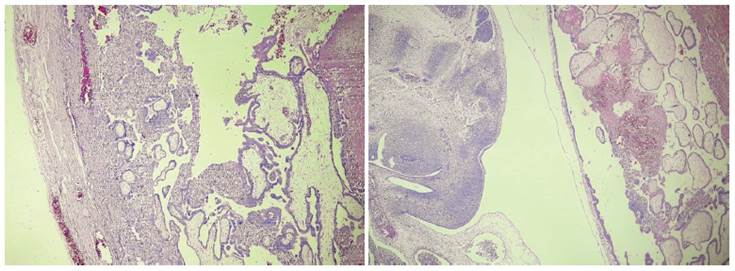
A 30-year old woman positive to the human immunodeficiency virus had been on antiretroviral therapy for the past 5 years. She had a history of conventional subtotal hysterectomy performed 6 years before due to uterine atony. She was admitted to the hospital with a 3-day hypogastric abdominal pain which caused nausea and vomiting. On physical examination there was pain on palpation of the hypogastrium and mobilization of the cervix. Speculoscopy showed no tumors or vaginal bleeding. In transvaginal ultrasonography, abundant free fluid was evidenced in the Douglas sac and a left 35 x 18 mm para-ovarian mass containing a gestational sac with a 9.5 mm embryo with cardiac activity was seen (Figure 1). It was considered a complicated ectopic pregnancy.In the intraoperative period, a hemoperitoneum of approximately 300 mL was found; the left uterine tube was ruptured, the left ovary was attached to the posterior wall and there were adhesions to the pelvic wall. Left salpingo-oophorectomy was performed with adhesions release and hemostasis control. In the histological study, chorionic villi infiltrating the muscular wall of the uterine tube was found as well as an embryo in the tubal lumen (Figure 2).
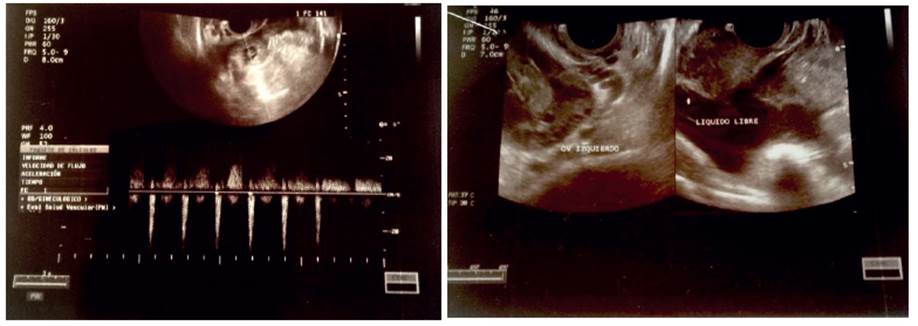
Figure 1 Transvaginal ultrasound. A) Left para-ovarian tumor containing a gestational sac and an embryo. B) Free fluid at the bottom of Douglas’ sac.
Discussion
The ectopic pregnancy in hysterectomized patients was made known for the first time in 18955. Since that first publication, 75 cases have been reported, including the present one. Most of them were in the uterine tube, although there are reports in other locations, such as the abdomen6 and the cervical stump7,8. These cases have presented early, usually between the first 2 to 3 months following the hysterectomy9, as well as belatedly, up to 12 years after10.
In cases presenting early, it is postulated that the pregnancy occurred prior to the surgery. Therefore, the surgical intervention was carried out in the periovulatory phase, when the sperm was in the tube, or the fertilized egg was heading for the uterine cavity3. When the uterus was removed, the development of gestation was confined within the uterine tube. When these cases become clinically apparent, they are often confused with post-surgical complications6, such as hematomas and/or pelvic abscesses.
Ectopic pregnancies that manifest themselves late have been reported in variable periods, from months to years after hysterectomy, as in the present case, which occurred six years later.
Some researchers have linked it to the type of hysterectomy, suggesting that it occurs mostly in the vaginal type, because of the type of surgical closure performed or because the adnexa are approximated or even incorporated into the vaginal stump during peritoneal closure for suspension of the vaginal vault. Another important factor associated with the development of ectopic pregnancy corresponds to the formation of a vaginal fistula as a result of vaginal infections, hematomas at the surgical site, or defects in the healing process of the vaginal stump. Although 50% of the cases occur in patients with a history of vaginal hysterectomy, reports show they can occur after any type of hysterectomy, including the abdominal6,11, in which the surgical closure leaves the adnexa distant from the vaginal stump.
To date, 15 cases prior to the present one has occurred following a supracervical hysterectomy3,7 (Figure 3), which is mainly performed in situations where blood loss is severe or there is an anatomical distortion that limits the extent of dissection12. It is believed that the formation of an ectopic pregnancy in these cases is due to the recanalization of the endocervical canal that was occluded during surgery, thus allowing the passage of sperm into the peritoneal cavity.
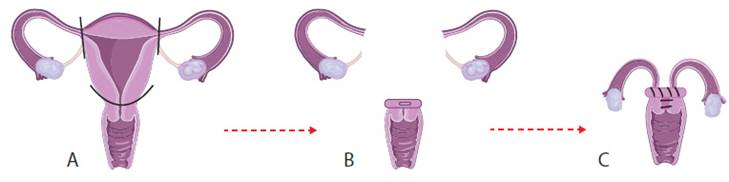
Figure 3 Supracervical hysterectomy. A) Uterus is removed. B) The cervix and adnexa are left. C) The tubo-ovarian pedicle is brought close to the cervical stump for the pelvic floor proper suspension, and the endocervical canal is closed.
It is interesting to make an association between the occurrence of these cases and the theoretical postulates that sperm capacitation occurs in the female genital tract. This capacitation has been proposed as a process of structural changes that sperm suffer since they are deposited in the vagina and then transported through the endocervical canal, uterus and fallopian tube to their encounter with the egg13. In the cases of ectopic pregnancies in patients with a history of total hysterectomy, this sperm capacitation would be diminished at two levels: cervix and uterine body. This fact suggests a more transcendent role for the fallopian tube in the process of sperm capacitation and invites research in this regard.
We present this case in order to make it known that, although early cases are treated diligently assuming them as post-surgical complications, those that happen late can lead to diagnosis delay, constituting an error with possible harmful consequences for the patient. In this sense, we suggest that ectopic pregnancy be considered within the differential diagnoses in patients of fertile age with abdominal pain, despite the history of hysterectomy.
On the other hand, as far as the surgical act is concerned, it would be advisable to avoid bringing the uterine tubes close to the vaginal or cer vical stump during peritoneal closure, as well as performing hysterectomies during the periovulatory phase, and to advise the patient not to have sexual relations or use barrier methods in the days prior to the surgery.
REFERENCES
1. ACOG Practice Bulletin no. 94: Medical management of ectopic pregnancy. Obstet Gynecol. 2008;111(6):1479-85. [ Links ]
2. Body S, Phillips C. Gynaecological causes of abdominal pain. Surgery. 2018;36(5):252-6. doi: 10.1016/j. mpsur.2018.03.009 [ Links ]
3. Fylstra D. Ectopic pregnancy after hysterectomy may not be so uncommon: A case report and review of the literature. Case Rep Women's Health. 2015;7:8-11. Doi: 10.1016/j.crwh.2015.04.001 [ Links ]
4. Ilea C, Stoian I, Carauleanu D, Socolov D. A case of ectopic tubal pregnancy eight years after a hysterectomy presenting as a diagnostic challenge. Am J Case Reports. 2019;20:1596600. DOI: 10.12659/AJCR.918894 [ Links ]
5. Wendler P. Ein fall con tubenschwangershaft nach extirpation uteri vaginalis. Monatsschr Geburtshilfe Gynakol. 1985(Suppl.):210. [ Links ]
6. Fader AN, Mansuria S, Guido RS, Wiesenfeld HC. A 14-week abdominal pregnancy after total abdominal hysterectomy. Obstet Gynecol. 2007 Feb 1;109(2 Part 2 Suppl):519-21. DOI: 10.1097/01.AOG.0000243774.14606.64 [ Links ]
7. Ahmed D, Fetene A, Asres E, Mekonnen A, Mamuye H. Cervical stump pregnancy 6 years after subtotal hysterectomy: a case report. J Med Case Reports. 2019;13(1):135. DOI: 10.1186/s13256-019-2077-9 [ Links ]
8. McDaniel JB, Jr, Gullo TV. Pregnancies after hysterectomies: a case report and review. J Natl Med Assoc. 1968;60:366-72. [ Links ]
9. Maheux AF, Kind S. Tubal ectopic pregnancy 12 weeks after laparascopic supracervical hysterectomy and tubal ligation. J Emerg Med Case Rep. 2018;9:8-9. DOI: 10.5152/jemcr.2018.1986 [ Links ]
10. Brown WD, Burrows L, Todd CS. Ectopic pregnancy after cesarean hysterectomy. Obstet Gynecol. 2002;99:933-4. [ Links ]
11. Cook S, Davies N. Ectopic pregnancy after total abdominal hysterectomy. J Obstet Gynaecol. 2014;34:90. doi: 10.3109/01443615.2013.830598 [ Links ]
12. Rock JA, Jones HW. Te Linde Ginecología Quirúrgica. Vol 1. 10a ed. Filadelfia: Panamericana. 2017;733-9. [ Links ]
13. De Jonge C. Biological basis for human capacitation-revisited. Hum Reprod Update. 2017;23:289-99. doi: 10.1093/humupd/dmw048 [ Links ]
11Right to privacy and informed consent: Information on the clinical history and histology examination were obtained from the surgical piece; therefore, no consent was needed from the patient
14Original contribution and importance: The importance of making this case public is based on the fact that the diagnosis of ectopic pregnancy is usually not considered when the patient has a history of hysterectomy, which postpones treatment, resulting in complications that put the patient's life at risk
Received: April 26, 2020; Accepted: June 15, 2020











 texto en
texto en