Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.66 no.4 Lima oct-dic 2020
http://dx.doi.org/10.31403/rpgo.v66i2282
Original Articles
Uterocervical angle or cervical length for prediction of impending preterm delivery in symptomatic patients
1. Doctor of Medical Sciences, Specialist in Gynecology and Obstetrics, Associate Physician, Gynecology and Obstetrics Service, Hospital Central "Dr. Urquinaona, Maracaibo, Venezuela
2. Doctor in Clinical Medicine, Professor at the Faculty of Medicine of the University of Zulia, Maracaibo, Venezuela
3. Doctor in Medical Sciences, Professor at the Faculty of Medicine of the University of Zulia, Maracaibo, Venezuela
4. Doctor in Medical Sciences, Specialist in Gynecology and Obstetrics. Associate Physician Gynecology and Obstetrics Service Central Hospital "Dr. Urquinaona, Maracaibo, Venezuela
5. Specialist Physician in Gynecology and Obstetrics, Associate Physician Gynecology and Obstetrics Service Hospital Central "Dr. Urquinaona, Maracaibo, Venezuela
6. Doctor in Medical Sciences, Specialist in Gynecology and Obstetrics, Professor at the Faculty of Medicine of the University of Zulia, Maracaibo, Venezuela
Objective:
To compare the uterocervical angle with the cervical length in the prediction of impending preterm delivery in symptomatic patients.
Design:
Case-control study. Institution: Central Hospital "Dr. Urquinaona", Maracaibo, Venezuela. Participants: Patients with preterm delivery within 7 days (group A) and pregnant women with preterm delivery beyond 7 days (group B).
Methods:
At the time of diagnosis, the patients were evaluated using transvaginal ultrasound and were followed until delivery. Main outcome measures: General characteristics, uterocervical angle, cervical length, impending preterm delivery, and prognostic efficacy.
Results:
326 patients were included, 75 women presented impending preterm delivery (group A) and 251 patients were considered as controls (group B). The patients in group A had significantly higher values of the uterocervical angle and lower cervical length compared to the patients in group B (p <0.0001). The uterocervical angle showed an area under the curve of 0.864, while the value of the area under the curve of cervical length was 0.985. The difference in the discrimination ability between the areas under the curve of each test was significant (p <0.0001).
Conclusion:
The uterocervical angle is not greater than the cervical length in predicting impending preterm delivery in symptomatic patients.
Key words: Uterocervical angle; Cervical length; Preterm delivery; Prediction
Introduction
Preterm delivery (PD) occurs in 10% to 12% of pregnancies and is associated with high rates of perinatal morbidity and mortality1. Its frequency has changed little in recent decades, due to the lack of effective methods to detect patients at risk and of adequate tools to reduce it.
Screening for pregnancies at risk for PD remains difficult, as most current strategies lack optimal precision. Transvaginal ultrasound is the standard for the evaluation of cervical length (CL) and the prediction of PD, since it is highly reproducible and is not affected by maternal obesity, cervical position, and fetal shading2. However, its sensitivity is relatively low (60%)3. Other predictors have not shown superior benefits4. Likewise, with the exception of a history of PD, all associated clinical risk factors (such as obesity) also have limited predictive capacity5.
Cervical tissue, made up of collagen fibers, has the function of maintaining pregnancy until reaching term and subsequently undergoing modifications to allow delivery6. Structural force on cervix is mediated by pressure from surrounding pelvic organs and the weight of the pregnant uterus. The combination of pressure, tension of the uterine wall, and individual anatomy produces cervical remodeling during pregnancy7. Orientation variations and asymmetry of the cervical canal - uterus result in alteration of the forces on the lower segment and the internal cervical os, beginning cervical dilation8.
The uterocervical angle (UCA), measured between the cervix and the lower uterine segment, has been proposed as an additional screening tool for PD9. An acute UCA reinforces the closure of the endocervical canal, while a more obtuse angle may facilitate opening of the cervix. Several studies have analyzed the predictive power of this measurement9-14. However, most of the studies have been retrospective and none have compared this marker with CL in the prediction of impeding delivery in patients with threatened PD.
The objective of the research was to compare the uterocervical angle with the cervical length in the prediction of imminent preterm delivery in symptomatic patients.
Methods
This was a prospective study conducted at the Hospital Central "Dr. Urquinaona", Maracaibo, Venezuela, from June 2014 to May 2020. Women with single pregnancies between 24 and 35 weeks, determined by ultrasound in the first trimester, with a clinical diagnosis of threatened PD (up to 3 uterine contractions in 30 minutes, cervical dilation less than 3 centimeters, effacement less than 80% and integral membranes) were consecutively selected. The study was approved by the Ethics Committee of the hospital. Written informed consent was obtained at the time of the selection of each participant.
Exclusion criteria were: multiple pregnancies, history of progesterone or any other tocolytic use in current pregnancy, known cervical insufficiency or history of cerclage, premature rupture of membranes, uterine abnormalities, abnormal placentation, maternal cardiac abnormalities, active inflammatory or infectious disease, hypertension and pre-gestational or gestational diabetes, fetal intrauterine growth restriction, congenital fetal abnormalities, changes in the volume of amniotic fluid, acute chorioamnionitis, and unknown gestational age. Patients who refused to participate or whose data were in-complete were also excluded from the study.
Within one hour of hospital admission, and before the start of any treatment, participants underwent a cervical examination with sterile speculum, performing fern and nitrazine paper tests to rule out membranes rupture. Immediately afterwards, the digital examination was carried out by the on-call personnel and confirmed by one of three investigators. Dilation, maturation, consistency and position of the cervix were evaluated, as well as fetal engagement to calculate Bishop’s score. They were then subjected to transabdominal fetal ultrasound evaluation to determine fetal presentation, placental insertion, fetal head and abdominal circumference measurement, femur length, and amniotic fluid index. Subsequently, the monitoring of the fetal heart rate and the evaluation of the characteristics of uterine contractions by tocodynamometry began.
Image acquisition was performed with the Voluson® V730 Expert ultrasound equipment (GE Healthcare, USA) and a volumetric and multi-frequency vaginal transducer (2 to 10 MHz). Pregnant women were placed in dorsal lithotomy position with an empty bladder. UCA measurements were performed using the previously described method9. The UCA is the triangular segment measured between the lower uterine segment and the cervical canal, which produces a measurable angle. This angle is created by the intersection of a first straight and unbroken line connecting the internal cervical os with the external cervical os. The internal os was identified as the point at the end of the endocervical mucosa, while the external os was identified as the most external point where the anterior and posterior lips of the cervix meet. The second line was drawn from the inferior aspect of the anterior uterine wall, passing through the end of the first line in internal cervical os (including the isthmus) and to the point of the internal inferior uterine segment, at an ideal distance of 3 centimeters (Figure 1). The final value was established by the average of three measurements.
The evaluation of CL by transvaginal ultrasound was done immediately after the determination of the UCA. This was performed by placing the 7.5 MHz transvaginal transducer in the anterior vaginal fornix, slowly withdrawing it to obtain a sagittal view of the cervix. In the absence of uterine contractions, all measurements were made by orienting the transducer to view the internal and external cervical os in the same plane. The image was magnified to 75% of screen and the length was measured as a straight line between two electronic markers with the furthest points and identified by sonolucence of the cervical canal. Three images were obtained and the one showing the shortest length was used.
All ultrasound measurements were performed by a single specialist in maternal-fetal medicine belonging to the research and who did not participate in the clinical care of the participants. The duration of the evaluation was less than 10 minutes and the members of the hospital team who performed the care were unaware of the results. Therefore, ultrasound measurements did not influence the management of the participants.
Initially, all selected pregnant women were admitted to be treated with bed rest in the left lateral decubitus position and hydrated with 500 mL of lactated Ringer's solution. If progressive cervical changes were documented or contractions persisted for at least 2 hours after treatment, they were hospitalized and tocolytic treatment was started, with calcium channel blockers as first-line therapy. During hospitalization, two 12 mg doses of intramuscular betamethasone were administered 24 hours apart to induce fetal lung maturation. Tocolytics were discontinued 48 hours after the first steroid dose.
A form was prepared that included the following data: identification number, maternal age, gestational age at the time of examination, parity, presence of bleeding, history of PD, digital cervical examination with determination of dilation and effacement, station and consistency and cervical position and UCA and CL values. The main study variable was frequency of imminent delivery (in the 7 days following the evaluation). Data were also included on the weight of the newborns at birth and the time interval between assessment and delivery. All data was recorded and stored for later analysis.
The data distribution was evaluated with the Shapiro-Wilk normality test. Categorical variables were analyzed using chi-square tests or Mann-Whitney U test. Continuous variables with normal distribution were compared with Student's t test. Those variables with a distribution other than the normal one were compared with the Wilcoxon rank sum test. Operator-receptor curves (ROC) were used to determine the best cut-off point and evaluate the diagnostic accuracy of UCA and CL in predicting impending PD. The Hanley McNei test was used to compare the differences in ROC areas of both tests. The sensitivity, specificity, negative predictive value, positive predictive value, and positive and negative likelihood ratios with their 95% confidence intervals (CI) in predicting impending PD were calculated for the optimal cutoff based on COR. The alpha level of statistical significance was p <0.05. All analyzes were performed with the SPSS® version 22.0 statistical package (SPSS Inc., USA).
Results
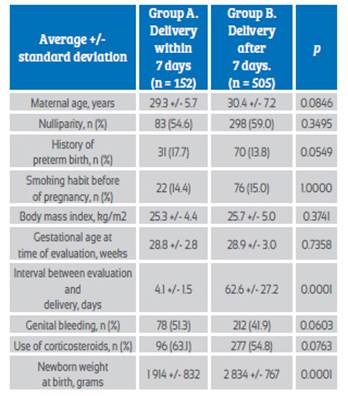
For the final analysis of the research, 326 patients were included, of which 152 women (31.7%) presented PD in the following 7 days of the evaluation (group A) and 251 patients (68.3%) had delivery afterwards of the 7 days (group B). Table 1 shows the general characteristics of the patients in each of the groups. No differences were found in relation to maternal age, nulliparity, history of PD, history of smoking before pregnancy and value of body mass index (p = ns). Gestational age at the time of evaluation for group A was 29.4 +/- 2.7 weeks and for group B, 29.9 +/- 2.9 weeks (p = ns). The interval between evaluation and delivery was 4.0 +/- 1.6 days for group A patients and 66.2 +/- 25.4 days for group B patients (p <0.0001). The weight of the newborns in group A was significantly lower than that of the patients in group B (p <0.0001).
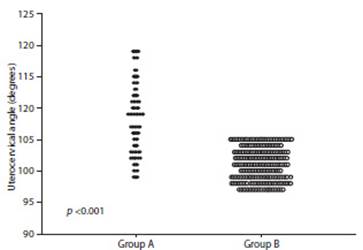
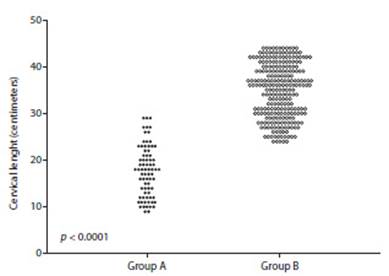
Regarding the ultrasound variables, the patients in group A presented significantly higher UCA values (108.1 +/- 5.7º) compared to the patients in group B (100.9 +/- 2.6º, p <0,0001; Figure 2). However, patients in group A (17.7 +/- 5.4 millimeters) showed significantly lower CL values compared to patients in group B (34.9 +/- 5.7 millimeters, p <0,0001; Figure 3).
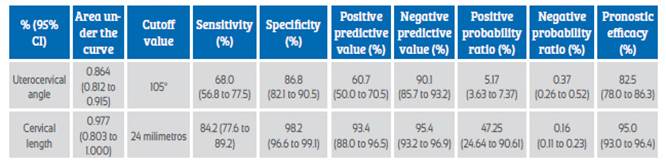
Figure 4 shows the ROC of the variables for predicting impeding PD. The UCA showed an area under the curve value of 0.864 (95% CI; 0.800 to 0.952) while the value of the area under the CL curve was 0.985 (95% CI; 0.733 to 1.000). The didifference in the discrimination capacity between the areas under the curve of each test was significant (p <0.0001). The combination of both elements improves the ability to predict the UCA (p = 0.0906), but it is lower than the CL (p <0.0001). The cutoff values, sensitivity, specificity, predictive values, probability ratios and prognostic efficacy for each of the tests are shown in Table 2.
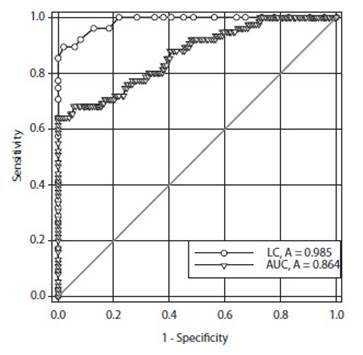
Figure 4 Operator-receptor curve of the prognostic capacity of the uterocervical angle and cervical length in the prediction of imminent preterm delivery in symptomatic patients.
Discussion
There is evidence that UCA is an ultrasound marker for the prediction of successful induction of labor15. Although in a limited way, it has also been shown to be useful in identifying pregnant women at risk of PD, as it may reflect cervical competence16. Results of this study show that patients with impeding preterm delivery had a significant increase in UCA compared to patients who delivered beyond 7 days. However, CL is more useful in predicting impending PD compa-red to UCA, confirming that CL is a more adequate predictor of impending PD.
In normal pregnancy, physiological loads of pregnancy produce compression and tension on the structures of the cervix, while the anatomical variants generate specific patterns of pressure on the internal os. Weight distribution can put pressure on the internal os, which can directly affect cervical direction17. These changes can also affect flexibility9. However, an indirect comparison of the orientation and dispersion of collagen fibers in the cervix of pregnant and non-pregnant women suggested that dispersion -direction of collagen may influence cervical remodeling18.
The clinical application of ultrasound screening and / or surveillance to establish cervical conditions in prediction of PD is limited by the lack of effective preventive interventions. The use of CL as a tool to estimate risk has been widely studied. Different guidelines recommend that patients with a history of PD be screened for CL in the second trimester19. Previous studies that used it as a screening tool in low-risk women during second trimester showed that CL equal to or less than 25 millimeters had a sensitivity of 37% for PD20, while the evaluation in high-risk pregnant women had sensitivity of only 19%21.
The positive predictive value of CL ranges from 18% for low-risk groups to 75% for high-risk groups20,21.
During labor, the Bishop score assesses cervical position to determine the likelihood of successful induction of labor. The posterior uterine angle is used to predict the success of vaginal delivery15. The UCA, formed by the angle between the endocervical canal and the anterior uterine wall, has been proposed by several studies as a predictor of PD9,10,13,21. Depending on the angle of inclination, the cervical canal can be considered "closed" in cases of acute UCA or "open" in cases of obtuse angle. Until recently, the UCA had only been used to evaluate small cohorts of patients with single pregnancies treated with a cervical pessary8,17,22.
There is conflicting evidence regarding the clinical use of the UCA with its predictive ability of PD. A first study retrospectively evaluated UCA in first and second trimesters and found significant differences between the group that presented PD compared to controls, both in the first and second trimesters10. Another retrospective cohort investigation found that women with pregnancies of 16-23 weeks and UCA equal to or greater than 105º had a greater chance of delivery before 34 weeks, with a sensitivity of 81% and a negative predictive value of 99%9. Another case-control study showed that a broader UCA (105º) during second trimester was related to PD14. Finally, a systematic review of the available evidence concluded that UCA measurements during the second trimester may be a useful method to determine the risk of PD23. On the other hand, in women with single pregnancies, there is evidence that a change in angle is associated with risk of cerclage failure11.
However, other studies have shown contrary results. A retrospective investigation found that a value greater than or equal to 105º between 19 and 24 weeks of gestation was related to a lower incidence of PD before 34 weeks. However, authors included pregnant women with short CL12. Another investigation found that the ROC value was 0.704 and the optimal cut-off value was 110º, with a sensitivity of 83% and a positive predictive value of 16%. The authors concluded that measurement during the second trimester was not a good predictor of PD24.
This is the first study to directly compare the prognostic ability of UCA and CL in the prediction of symptomatic PD patients. The results of this study showed that UCA has a lower sensitivity (68.0%) than CL (89.3%) in predicting impending PD. The positive predictive value of UCA was 60.7% compared to 83.1% of CL. Although the positive predictive value depends on the prevalence of disease, in this research these factors, as there are no differences between the groups, seem to have no effect on the values. Differences with previous studies may be due to the retrospective design of these investigations, small sample values, and differences in the selection criteria. Furthermore, most of the previously cited studies selected pregnant women with gestational ages between 16 and 24 weeks, while in this study pregnant women between 24 and 35 weeks were selected.
The present study has several strengths. It is a prospective study, for which pregnant women with a definitive outcome (impeding PD) were selected, with relatively homogeneous groups in their general characteristics. Ultrasound measurements were performed by a limited group of specialists following established protocols.
Among the limitations, the technique of precise identification of the ultrasound plane can be difficult, since, in cases of adherence, abnormal cervical position can distort the measurement. This can be avoided by following standard methodology. Furthermore, the present study was conducted in a single center and may be subject to participant selection bias. Given that both measurements were only performed on admission, it is unknown whether the serial evaluation of the parameters would modify the prediction value of impending PD.
In conclusion, although the UCA is significantly higher in patients with imminent preterm delivery, it is not higher than the CL in symptomatic patients.
REFERENCES
1. Lamont RF. Spontaneous preterm labour that leads to preterm birth: An update and personal reflection. Placenta. 2019;79:21-9. doi: 10.1016/j.placenta.2019.03.010 [ Links ]
2. Thain S, Yeo GSH, Kwek K, Chern B, Tan KH. Spontaneous preterm birth and cervical length in a pregnant Asian population. PLoS One. 2020;15(4):e0230125. doi: 10.1371/journal.pone.0230125 [ Links ]
3. Son M, Miller ES. Predicting preterm birth: Cervical length and fetal fibronectin. Semin Perinatol. 2017;41(8):445-51. doi: 10.1053/j.semperi.2017.08.002 [ Links ]
4. Berghella V, Saccone G. Fetal fibronectin testing for reducing the risk of preterm birth. Cochrane Database Syst Rev. 2019;7(7):CD006843. doi: 10.1002/14651858.CD006843.pub3 [ Links ]
5. Damaso EL, Rolnik DL, Cavalli RC, Quintana SM, Duarte G, da Silva Costa F, et al. Prediction of preterm birth by maternal characteristics and medical history in the Brazilian population. J Pregnancy. 2019;2019:4395217. doi: 10.1155/2019/4395217 [ Links ]
6. Myers KM, Feltovich H, Mazza E, Vink J, Bajka M, Wapner RJ, et al. The mechanical role of the cervix in pregnancy. J Biomech. 2015;48(9):1511-23. doi: 10.1016/j.jbiomech.2015.02.065 [ Links ]
7. Yellon SM. Contributions to the dynamics of cervix remodeling prior to term and preterm birth. Biol Reprod. 2017;96(1):13-23. doi: 10.1095/biolreprod.116.142844 [ Links ]
8. Jayyosi C, Lee N, Willcockson A, Nallasamy S, Mahendroo M, Myers K. The mechanical response of the mouse cervix to tensile cyclic loading in term and preterm pregnancy. Acta Biomater. 2018;78:308-19. doi: 10.1016/j.actbio.2018.07.017 [ Links ]
9. Dziadosz M, Bennett TA, Dolin C, West Honart A, Pham A, Lee SS, et al. Uterocervical angle: a novel ultrasound screening tool to predict spontaneous preterm birth. Am J Obstet Gynecol. 2016;215(3):376.e1-7. doi: 10.1016/j.ajog.2016.03.033 [ Links ]
10. Sochacki-Wójcicka N, Wojcicki J, Bomba-Opon D, Wielgos M. Anterior cervical angle as a new biophysical ultrasound marker for prediction of spontaneous preterm birth. Ultrasound Obstet Gynecol. 2015;46(3):377-8. doi: 10.1002/uog.14801 [ Links ]
11. Knight JC, Tenbrink E, Sheng J, Patil AS. Anterior uterocervical angle measurement improves prediction of cerclage failure. J Perinatol. 2017;37(4):375-9. doi: 10.1038/jp.2016.241 [ Links ]
12. Lynch TA, Szlachetka K, Seligman NS. Ultrasonographic change in uterocervical angle is not a risk factor for preterm birth in women with a short cervix. Am J Perinatol. 2017;34(11):1058-64. doi: 10.1055/s-0037-1603653 [ Links ]
13. Sepúlveda-Martínez A, Díaz F, Muñoz H, Valdés E, Parra- Cordero M. Second-trimester anterior cervical angle in a low-risk population as a marker for spontaneous preterm delivery. Fetal Diagn Ther. 2017;41(3):220-5. doi: 10.1159/000447588 [ Links ]
14. Farràs Llobet A, Regincós Martí L, Higueras T, Calero Fernández IZ, Gascón Portalés A, Goya Canino MM, et al. The uterocervical angle and its relationship with preterm birth. Matern Fetal Neonatal Med. 2018;31(14):1881-4. doi: 10.1080/14767058.2017.1331427 [ Links ]
15. Rane SM, Guirgis RR, Higgins B, Nicolaides KH. The value of ultrasound in the prediction of successful induction of labor. Ultrasound Obstet Gynecol. 2004;24(5):538-49. doi: 10.1002/uog.1100 [ Links ]
16. Corrêa TD, Amorim EG, Tomazelli JAG, Corrêa MD Júnior. Use of the pessary in the prevention of preterm delivery. Rev Bras Ginecol Obstet. 2019;41(1):53-8. doi: 10.1055/s-0038-1676511 [ Links ]
17. Vink J, Mourad M. The pathophysiology of human premature cervical remodeling resulting in spontaneous preterm birth: Where are we now? Semin Perinatol. 2017;41(7):427-37. doi: 10.1053/j.semperi.2017.07.014 [ Links ]
18. Yao W, Gan Y, Myers KM, Vink JY, Wapner RJ, Hendon CP. Collagen fiber orientation and dispersion in the upper cervix of non-pregnant and pregnant women. PLoS One. 2016;11(11):e0166709. doi: 10.1371/journal.pone.0166709 [ Links ]
19. Jacobsson B, Saltvedt S, Wikström AK, Morken NH, Leijonhufvud Å, Hagberg H. Preterm delivery: an overview on prediction, prevention and treatment. Lakartidningen. 2019;116:FSST. [ Links ]
20. Esplin MS, Elovitz MA, Iams JD, Parker CB, Wapner RJ, Grobman WA, et al. Predictive accuracy of serial transvaginal cervical lengths and quantitative vaginal fetal fibronectin levels for spontaneous preterm birth among nulliparous women. JAMA. 2017;317(10):1047-56. doi: 10.1001/jama.2017.1373 [ Links ]
21. Chen L, He J, Yue Q, Zhu C, Shen W, Yao M, et al. Association between mid-trimester cervical length and risk of spontaneous preterm birth is modified by a prior cervical excisional procedure. Int J Clin Exp Pathol. 2019;12(6):2249-56. eCollection 2019. [ Links ]
22. Kyvernitakis I, Maul H, Bahlmann F. Controversies about the secondary prevention of spontaneous preterm birth. Geburtshilfe Frauenheilkd. 2018;78(6):585-95. doi: 10.1055/a-0611-5337 [ Links ]
23. Daskalakis G, Theodora M, Antsaklis P, Sindos M, Grigoriadis T, Antsaklis A, et al. Assessment of uterocervical angle width as a predictive factor of preterm birth: a systematic review of the literature. Biomed Res Int. 2018;2018:1837478. doi: 10.1155/2018/1837478 [ Links ]
24. Sawaddisan R, Kor-Anantakul O, Pruksanusak N, Geater A. Uterocervical angle measurement for preterm birth prediction in singleton pregnant women with no history of preterm birth and normal cervical length: A prospective cohort study. Eur J Obstet Gynecol Reprod Biol. 2020;252:30-5. doi: 10.1016/j.ejogrb.2020.06.020 [ Links ]
Received: August 27, 2020; Accepted: September 24, 2020











 texto en
texto en