Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.66 no.4 Lima oct-dic 2020
http://dx.doi.org/10.31403/rpgo.v66i2284
Original Articles
Non-puerperal mastitis in a Medellin (Colombia) reference center
1. Mastologist, CES University, MSc Epidemiology and Public Health VIU, IDC Cancer Research Group, Professor UniRemington, Medellín, Colombia
Objective:
To describe the sociodemographic data, clinical manifestations and treatment in patients diagnosed with non-puerperal mastitis.
Methods:
Descriptive, retrospective study of medical records in the institutional database between January 1, 2016 and December 31, 2019. Demographic, clinical and treatment data was collected and analyzed using descriptive statistics.
Results:
The prevalence of non-puerperal mastitis was 3.8%, in mestizo women about 40.4 years-old at time of diagnosis. The most frequent reason for consultation was inflammatory changes in breast in 84.8% (n = 28), and presence of mass in 12.1% (n = 4). There was association with smoking in 33.3% (n = 11). 97% of the patients received initial treatment with antibiotics (n = 32), and ultrasound-guided drainage was performed in 7 cases (21.2%). No case had drainage by mastotomy, and one patient (9%) was treated with quadrantectomy-type resection. Resolution was obtained in 97% of cases (n = 32) in 4.4 months average, and 7 patients (21.2%) had recurrence.
Conclusion:
In this study, non-puerperal mastitis affected women in the fourth decade of life with inflammatory changes and pain. Evolution was chronic with episodes of recurrence. Usually the disorder resolved with antibiotics and some needed ultrasound-guided drainage. Up to one third of cases was associated with smoking.
Key words: Breast; Mastitis; Abscess
Introduction
There are many classifications of mastitis. The best known divides it into infectious (puerperal) and non-infectious (granulomatous mastitis). According to the time of clinical presentation, it is considered acute and chronic1. This article is aimed at mastitis not associated with lactation, a rare disorder, with a prevalence of 1 to 2%2. Lactiferous duct ectasia plays a part in the etiopathogenesis, and is associated with periductal mastitis with dilatation of the lactiferous ducts, occurring in 5 to 9% of non-lactating women3.
Although several cases of non-puerperal mastitis and subareolar abscess were described in the late 1800s, it is Zuska and her colleagues who are credited with knowledge of the disease4. In 1951, they published clinical and pathological findings in five patients with non-puerperal mastitis complicated with abscess and recurrent lactiferous duct fistula. All cases were associated with subareolar mass and pathological telorrhea. The main microscopic findings were acute and chronic inflammation of the lactiferous duct, duct dilation, stasis, and desquamative keratinization of the epithelium in the duct lumen. The authors concluded that the disease was associated with stasis of secretions within the duct, which led to dilation and inflammation or infection, abscess formation and rupture through the skin, creating a fistulous tract.
These abscesses have a chronic course, with recurrent obstruction of the ducts with keratin plugs and a tendency to fistula formation5,6. Abscesses, in general, are central, peri, or subareolar. Risk factors include smoking and diabetes7,8.
The objective of this retrospective study was to review the clinical aspects, diagnosis and treatment of patients with non-puerperal mastitis who attended the mastology consultation at the Profamilia clinic in the city of Medellín. It is the largest series of cases reported in Latin America.
Methods
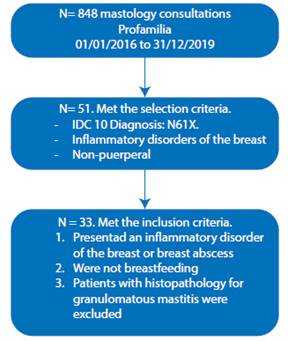
This is a retrospective descriptive study of users treated in the mastology consultation at the Profamilia clinic in the city of Medellín, between January 1, 2016 and December 31, 2019. The clinical records of 848 users treated with the code IDC 10 N61X Inflammatory disorders of the breast were found. 53 records with the diagnosis of non-puerperal mastitis were identified, and an independent database for this cohort of patients was created. 18 cases with diagnosis of granulomatous mastitis were excluded and the subgroup of 33 cases with diagnosis of non-puerperal mastitis and subareolar abscess was analyzed.
The demographic data, clinical and pathological characteristics of the patients were obtained from the clinical history, and data on ethnic origin, age, history of smoking, clinical characteristics as reason for consultation, findings on physical examination, affected side, findings on ultrasound, mammography, types of treatment such as antibiotic therapy or surgery, follow-up and recurrence were included.
The study established three diagnostic criteria necessary for non-puerperal mastitis:
Presenting an inflammatory breast disorder or a breast abscess
No breastfeeding
Patients with histopathology for granulomatous mastitis were excluded.
Descriptive analysis of sociodemographic and clinical variables was performed. Absolute frequencies and percentages, mean and standard deviation were calculated, according to the nature and distribution of the variables. The normal distribution was validated using the Shapiro Wilk test. A bivariate analysis was performed using the chi2 test to establish the association between resolution or recurrence, treatment modalities, and risk factors. For the hypothesis tests, a 95% confidence interval and a 5% significance level were set. Epidat software version 3.1 was used.
The research was submitted to the Profamilia medical ethics committee, a protocol that was authorized by the medical direction. This is considered a risk-free study, in accordance with the classification set forth in Article 11 of Resolution No. 008430 of 1993, issued by the Ministry of Health of Colombia, and is in line with international regulations -Helsinki declaration and ethical guidelines for biomedical research prepared by the Council for International Organizations of Medical Sciences - CIOMS-.
Results
Of the total of 848 patients seen in the period established with diagnosis of inflammatory disorders of the breast, 53 patients with non-puerperal mastitis were identified; 33 patients met the inclusion criteria, with prevalence of 3.8% (Figure 1).
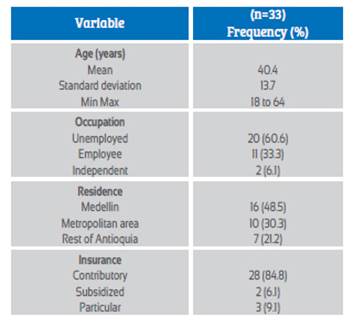
The 33 cases were mestizo women, 48.5% were Medellin residents (n = 16), with mean age 40.4 years (SD 13.7. Range 18 to 64). The sociodemographic characteristics are shown in Table 1.
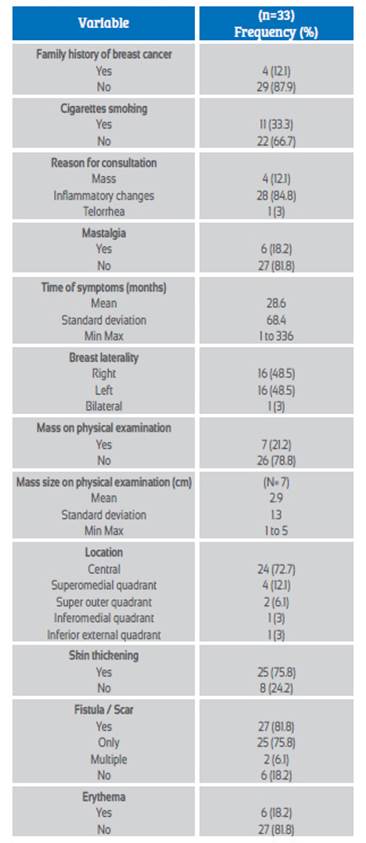
The most common reason for consultation was inflammatory changes, in 84.8% (n = 28), followed by associated mastalgia, in 81.8% (n = 6); the mean time of symptoms was 28.6 months (SD 68.4. Range 1 to 336). Breast involvement did not have a dominant laterality and the most frequent location was central or retroareolar, with 72.7% (n = 24). The most frequent clinical signs were skin thickening with 75.8% (n = 25), fistula / scar with 81.8% (n = 27), mass in 7 cases (21.2%) and erythema in 6 cases (18.2%); there were no cases with lymphadenopathy or fever. 33.3% of the patients used tobacco (n = 11) and 12.1% (n = 4) had a family history of breast cancer. The clinical characteristics are shown in Table 2.
The auxiliary studies included secretion culture in 9 patients (27.3%), positive in 3 patients (15.2%), breast ultrasound in all cases (n = 33) with collection as the most common finding with 54.5% (n = 18), nodule in 18.2% (n = 6) and non-specific benign changes in 18.2% (n = 6); the most frequent BIRADS (Breast Imaging Reporting and Data System) classification was category 2, with 38.4% (n = 13), and a collection with abscess in 54.5% (n = 18). Mammography was performed in 10 cases (30.3%) and 45.5% (n = 15) required a core needle breast biopsy.
The mean follow-up was 3.5 months (SD = 4.7. Range 1 to 18). In 97% of the cases the disease resolved (n = 32) in 4.4 months average (SD = 3.9. Range 1 to 12). There were 7 cases (21.2%) with recurrence, with 2.5 episodes (SD 3.0. Range 1 to 10) average.
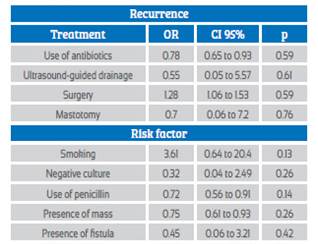
Antibiotic therapy was the treatment most used, in 97% (n = 32), with mean duration of treatment of 9.1 days (SD 2.7. Range 7 to 14). Multiple antibiotics were used in 63.6% (n = 21), and only penicillin in 18.2% (n = 6). Ultrasound-guided drainage was performed in 7 cases (21.2%) and mastotomy in no case. Only in one case (3%) a quadrantectomy was performed, and there was no case of mastectomy. Table 3 shows the bivariate analysis for the association between recurrence of non-puerperal mastitis and the different types of treatment and risk factors.
Discussion
The prevalence of non-puerperal mastitis in the present study was 3.8%, similar to that found by Zuska et al.4 of 2%. Duct ectasia, as part of the etiopathogenesis, is associated with periductal mastitis with dilation of the lactiferous ducts, and occurs in 5% to 9% of non-lactating women3.
The mean age in this series was 40 years, with a range between 18 and 64 years, similar to that found by Rizzo et al.9,10, in women aged 18 to 50 years. Hanavadi, Lannin et al. found the age range from adolescence to 80 years, with a maximum incidence at 40 years11,12. In the present study, one third had history of smoking; Schäfer, Bundred et al.13,14 have described association and cigarette smoking in 90% of women.
The most common clinical presentation in this series was breast changes such as inflammation, thickening of the skin, pain, abscess formation, and fistulas. Dixon2 has described the presentation of fistulas in 30% of the cases that characteristically extend from the abscess cavity or dilated duct towards the nipple or the edge of the areola. They can affect any quadrant, with greater tendency to the subareolar region, similar to that found by Versluijs-Ossewaarde et al.5, where around 90% of the abscesses in periductal mastitis were sub-areolar. The most important differential diagnosis includes locally advanced carcinoma and inflammatory breast carcinoma15. In the present series, 45.5% of patients underwent sharp biopsy without report of malignancy in any case.
Ultrasound was performed in the 33 cases reviewed, and the most common ultrasound findings were heterogeneous collection, areas of echogenicity with cutaneous fistula and thickening of the overlying skin. The BIRADS 2-3 classification was the most frequent, similar to that reported by Lequin, Tan, Fu et al.16-18 that indicate diffuse increased echogenicity of the affected area in the presence of abscesses, hypoechoic collections, internal echoes and ill-defined margins, and heterogeneous hypoechoic masses, in up to 50% of cases.
Treatment is controversial, and includes the use of antibiotics, abscess drainage, and surgery. In general, it is an infectious disease that requires antibiotic therapy. In the present series, antibiotics were used in 97% of the cases, multiple antibiotics in 63.6%. Bharat, Bundred, et al.14,19 have reported higher rates of recurrence and complications associated with mixed flora, anaerobic bacteria and Proteus.
In the present study, 97% of the cases of non-puerperal mastitis resolved completely in an average period of 7 months. A significant percentage of 21.2% presented recurrence, while Scholefield et al.20 found a higher recurrence rate of 50%. Non-surgical management (97%) was preferred in this study, and included antibiotic therapy and ultrasound-guided drainage. Some authors have suggested that conservative management is the most appropriate treatment method11,12.
The limitations of this study include its retrospective nature, and there were no variables such as the use of oral contraceptives.
In conclusion, non-puerperal mastitis is a benign inflammatory disease of the breast, with a well-described, infrequent etiopathogenesis and a wide diagnostic spectrum. It affects women in their fourth decade of life and generally presents with inflammatory changes and breast pain. Ultrasound is useful in determining the characteristics of abscessed masses and collections, being useful for taking the biopsy and percutaneous drainage. The diagnosis is clinical and the microbiological study is useful in determining the bacterial sensitivity. An adequate selection of antibiotic therapy is essential, leaving surgical resection for few cases. Recurrence is high, and long-term follow-up is essential.
REFERENCES
1. Hegg R, Barros A.C.S.D, Pinotti M. Breast Infections. In: Benign Breast Tumors. FIGO. Bonilla-Musoles F (ed). 1994; 211-23. [ Links ]
2. Dixon JM. Periductal mastitis/duct ectasia. World J Surg. 1989; 13:715-720. DOI: 10.1007/BF01658420. [ Links ]
3. AbdelHadi MSA, Bukharie HA. Breast infections in non-lactating women. J Family Community Med. 2005; 12: 133-7. [ Links ]
4. Zuska JJ, Crile G Jr, Ayres WW. Fistulas of lactiferous ducts. Am J Surg. 1951; 81:312-7. DOI: 10.1016/0002-9610(51)90233-4. [ Links ]
5. Versluijs-Ossewaarde FN, Roumen RM, Goris RJ. Subareolar breast abscesses: characteristics and results of surgical treatment. Breast J. 2005;11:179-82. DOI: 10.1111/j.1075-122X.2005.21524.x. [ Links ]
6. Li S, Grant CS, Degnim A, Donohue J. Surgical management of recurrent subareolar breast abscesses: Mayo Clinic experience. Am J Surg. 2006; 192: 528-9. DOI: 10.1016/j.amjsurg.2006.06.010. [ Links ]
7. Rizzo M, Gabram S, Staley C, Peng L, Frisch A, Jurado M, Umpierrez G. Management of breast abscesses in nonlactating women. Am Surg. 2010; 76: 292-5. [ Links ]
8. Marchant DJ. Inflammation of the breast. Obstet Gynecol Clin North Am. 2002; 29: 89-102. DOI: 10.1016/s0889-8545(03)00054-8. [ Links ]
9. Han BK, Choe YH, Park JM, Moon WK, Ko YH, Yang JH, et al. Granulomatous mastitis: mammographic and sonographic appearances. AJR. 1999; 173:317- 20. [ Links ]
10. DeHertogh DA, Rossof AH, Harris AA, Economou SG. Prednisone management of granulomatous mastitis. N Eng J Med. 1980; 308:799-800. [ Links ]
11. Hanavadi S, Pereira G, Mansel RE. How mammillary fistulas should be managed. Breast J. 2005; 11:254-256. DOI: 10.1111/j.1075-122X.2005.21641.x. [ Links ]
12. Lannin DR. Twenty-two year experience with recurring subareolar abscess and lactiferous duct fistula treated by a single breast surgeon. Am J Surg. 2004; 188:407-10. DOI: 10.1016/j.amjsurg.2004.06.036. [ Links ]
13. Schäfer P, Fürrer C, Mermillod B. An association of cigarette smoking with recurrent subareolar breast abscess. Int J Epidemiol. 1988; 17:810-3. DOI: 10.1093/ije/17.4.810. [ Links ]
14. Bundred NJ, Dover MS, Coley S, Morrison JM. Breast abscesses and cigarette smoking. Br J Surg. 1992; 79:58-9. [ Links ]
15. Al-Khaffaf B, Knox F, Bundred NJ. Idiopathic granulomatous masti¬tis: a 25-year experience. J Am Coll Surg. 2008;206:269-73. [ Links ]
16. Lequin MH, van Spengler J, van Pel R, van Eijck C, van Overhagen H. Mammographic and sonographic spectrum of non-puerperal mastitis. Eur J Radiol. 1995; 21:138-42. [ Links ]
17. Tan H, Li R, Peng W, Liu H, Gu Y, Shen X. Radiological and clinical features of adult non-puerperal mastitis. Br J Radiol. 2013 Apr;86(1024):20120657. doi: 10.1259/bjr.20120657. [ Links ]
18. Fu P, Kurihara Y, Kanemaki Y, Okamoto K, Nakajima Y, Fukuda M, Maeda I. High-resolution MRI in detecting subareolar breast abscess. AJR Am J Roentgenol. 2007 Jun;188(6):1568- 72. doi: 10.2214/AJR.06.0099. [ Links ]
19. Bharat A, Gao F, Aft RL, Gillanders WE, Eberlein TJ, Margenthaler JA. Predictors of primary breast abscesses and recurrence. World J Surg. 2009; 33:2582-6. DOI: 10.1007/s00268-009-0170-8. [ Links ]
20. Scholefield JH, Duncan JL, Rogers K. Review of a hospital experience of breast abscesses. Br J Surg. 1987; 74:469-70. DOI: 10.1002/bjs.1800740613. [ Links ]
Received: June 09, 2020; Accepted: August 19, 2020











 texto en
texto en