Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.67 no.1 Lima ene./mar 2021
http://dx.doi.org/10.31403/rpgo.v67i2303
Special Articles
Vaginohysteroscopy, diagnosis and treatment of endometrial pathologies in office
1Staff Physician INMATER, fertility clinic
2Staff Physician Instituto Peruano de Medicina y Cirugía Fetal
3Staff Physician Clínica San Felipe
4Staff Physician Clínica Detecta
5Staff Physician Clínica San Judas Tadeo
In recent years there have been important technological advances, many applied to the medical field, allowing the evolution of numerous procedures. An example is hysteroscopy, where the miniaturization of its instruments and the improvement in the resolution of the images have allowed its evolution from an exclusive procedure in the operating room to use in the office. Vaginohysteroscopy allows the diagnosis of most endometrial pathologies without anesthesia, speculum, clamping or dilation of the cervix. It presents a series of advantages such as good tolerance by the patient, lower costs, less waiting time to resolve the pathologies and shorter work rest, making this procedure the standard for the diagnosis and treatment of endometrial and endocervical pathologies.
Key words: Hysteroscopy; infertility; vaginohysteroscopy; office hysteroscopy
Introduction
Hysteroscopy is a procedure that takes advantage of the endocervical canal as a natural access route to the endometrial cavity, a unique advantage for direct visualization in the diagnosis of uterine pathology and the opportunity to obtain biopsies. Without hysteroscopy, up to 58% of endometrial polyps, 50% of hyperplasia cases, 30% of focal lesions, and 11% of cancers could be missed1 when blind methods are used. such as uterine curettage or manual vacuum aspiration (MVA). In addition, hysteroscopy allows treatment to be carried out under direct vision, reducing the risk of partial or inadequate resolution of these pathologies (Figure 1).

Figure 1 (A) Shows the sequence of images of the same patient with an endometrial polyp, (b) its partial extraction after manual vacuum aspiration, and (c) vision of the cavity after hysteroscopic polypectomy with blunt tip scissors.
From 1869, when Pantaleoni reported the first successful hysteroscopy 2, to the present day, great technological advances have allowed hysteroscopy to go from being a rare procedure, due to its considerable technical challenges, to being one of the most widely used ambulatory gynecological procedures in the world3. These factors include the emergence of more efficient light sources, digital and optical endoscopic video cameras with more advanced lens systems, which have meant better image quality. In addition, thinner optics have appeared, up to 2 mm in diameter (Figure 2), with a system of lenses or optical fibers, the basis for the miniaturization of hysteroscopes and easier and painless access to the uterine cavity.

Figure 2 (A) overview of (1) 2 mm, (2) 2,9 mm and (3) y 4 mm optics. (b) close-up of optics in figure a. (image courtesy dr. marcelo velit).
Hysteroscopy has thus gone from being a procedure that was performed exclusively in the operating room with anesthesia and cervical dilation, to one that can be performed in the office, without anesthesia or sedation and, in the case of vaginohysteroscopy, without a speculum, clamping or dilation of the cervix, eliminating the discomfort caused by manipulation of the vagina and uterine cervix. These advantages have led vaginohysteroscopy to be suggested as the standard technique for ambulatory hysteroscopy4.
Hysteroscopy, depending on the site where it is performed and the type of anesthesia used, can be classified into those that are performed in the operating room and those that are performed in the office. In the first, mono or bipolar resectoscopes of 18.5, 22 and 26 Fr are used, which, due to their diameter, require the dilation of the cervical canal and, therefore, the use of anesthesia or sedation of the patient. Until the appearance of Hamou's diagnostic set, in the 1980s, hysteroscopy in the operating room was the most used modality. The current trend is to use operating room hysteroscopy mainly in challenging cases, such as endometrial ablation, fibroids larger than 1.5 cm, wide-based septa and large polyps, tending to pass the rest of the procedures to the office5.
Among the hysteroscopies performed in the office or officinal hysteroscopies, we can find three types: diagnostic, classic or conventional and vaginohysteroscopy. They all have common points that are performed in the office and that instruments with a diameter equal to or less than 5 mm are used. Among its peculiarities, diagnostic hysteroscopy allows direct visualization of the uterine cavity and identify its pathologies, for which a diagnostic sleeve with a single channel is used for the exclusive use of the optics. Classic or conventional hysteroscopy and vaginohysteroscopy differ only in the way they access the cervix. In the first, a speculum and clamping of the cervix are used to visualize and enter the external cervical os. This technique is less and less used, and even some literature considers it as obsolete6.
Over time, conventional hysteroscopy evolved to vaginohysteroscopy, in which the principle “don't touch” proposed by Bettocchi and Selvaggi in 19977 is applied. For this, the hysteroscope is placed directly into the vaginal introitus, introducing the medium of distention that allows the separation of the vaginal walls and the entry of the operative sleeve through the external cervical os and cervical canal. It eliminates the pain that occurs when placing the speculum and manipulating the cervix8, making the method better tolerated by patients.
Conventional hysteroscopy and vaginohysteroscopy employ shirts that are both diagnostic and operative. They provide the advantages of diagnostic hysteroscopy in a single time, allowing the procedure to be performed in the office without anesthesia, sedation, dilation or clamping of the cervix. It also provides the strengths of operating room hysteroscopy by allowing biopsies and treatment of endocavitary pathologies, such as submucosal myomas, endometrial polyps, release of uterine synechiae, resection of thin base septa, removal of intrauterine device, taking of targeted biopsies of endometrial thickening, lesions suggestive of cancer and endocervical pathologies.
Advantages of vaginohisteroscopy
Vaginohysteroscopy does not have a statistically significant difference compared to intraoperative hysteroscopy in terms of efficacy, sensitivity, and specificity in the detection of intrauterine lesions9. It omits the risks of anesthesia, reduces recovery times, provides greater convenience and profitability for patients, and reduces work permits8,9. This has led to the current trend towards performing most hysteroscopic procedures in the office.
Vaginohysteroscopy and ultrasound
Ultrasound is very effective in evaluating intramural and extramural uterine disease, such as type III-VII fibroids and ovarian pathologies. It also has good sensitivity and specificity in the diagnosis of endometrial pathologies and, if supplemented with saline infusion, the sensitivity and specificity increase from 89% and 56% to 91.8% and 60%, respectively. Despite these results, vaginohysteroscopy remains the gold standard with sensitivity and specificity of 97.3% and 92%, respectively10. It allows the identification of endometrial pathologies such as sub-mucosal fibromas and small polyps located in the isthmic and cornual cervix11, as well as the uterine synechiae that are difficult to identify by ultrasound. Its higher sensitivity and specificity differentiate it from the rest of the less invasive indirect imaging methods, such as transvaginal ultrasound, hysterosalpingography (HSG) and hysterosonography. Vaginohysteroscopy allows direct vision and resolution or taking targeted biopsies of pathologies12.
Vaginohysteroscopy in gynecology
The utility of vaginohysteroscopy in the gynecological area is evident in the study and treatment of bleeding in menopausal patients, dysfunctional bleeding, confirmation of ultrasound images that suggest endocavitary pathology such as fibroids, polyps, endometrial thickening and other, with the possibility of correction of these in up to 70% of cases in a single procedure, "see and treat principle" 13 (Figure 3). Based on this, the United Kingdom’s National Institute of Health and Clinical Excellence, NICE, has promoted a radical paradigm shift in the diagnosis of abnormal genital bleeding (HMB), reflected in its NG88 guideline 14 published in late 2018. Indicate vaginohysteroscopy in women with HMB if their history suggests submucosal fibroids, polyps or endometrial pathology, displacing ultrasound as a first-line procedure in the diagnosis of these pathologies. This change is based on the fact that vaginohysteroscopy provides more precise diagnoses and treatments, making it a more profitable tool for health policy. Another utility is the extraction of intrauterine devices whose threads are not evident through the external cervical os. This significantly reduces the risk of uterine perforation or rotation of the same by blind maneuvers.
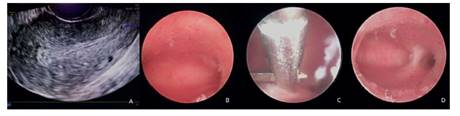
Figure 3 longitudinal section of the uterus. (a) at the fundus of the endometrial cavity, there is a slight increase in echogenicity. (b) a vaginohysteroscopy is performed, showing uterine synechia in the left horn. (c) excision of the same with blunt tip scissors. (d) the normal endometrial cavity can be seen after treatment
Vaginohysteroscopy in infertulity
The uterus plays a fundamental role in human reproduction. Pathologies such as polyps, endometritis, intrauterine synechiae, isthmocele, leiomyoma, Müllerian anomalies, among others, can compromise implantation and placentation, producing a negative impact on fertility. These pathologies can be found among 40-50% of infertile women and constitute 6-11% of the causes of infertility15. Hence the importance of ensuring a suitable uterine cavity to achieve a healthy child at home. As a valuable tool, hysteroscopy has been gaining importance over the years, which is expressed in the phrase of Dr. Linda Bradley “the hysteroscope should be considered the stethoscope for the uterus”16).
At present, the role of hysteroscopy in the treatment of endometrial pathologies is not in dispute, regarding its usefulness in improving reproductive results in relation to ultrasound or saline infusion ultrasound. Despite the number of publications confirming its importance, there are two recent trials, inSIGHT17 and TROPHY18, that have not shown benefit with the use of hysteroscopy. However, these studies had several limitations that may affect their generalizability. The fact is that robust and high-quality randomized clinical trials are needed before hysteroscopy can be considered a first-line procedure in all infertile women19. However, we cannot ignore the advantages of examining most endometrial cavity under direct vision and the possibility of taking biopsies or solving most endometrial pathologies in the same surgical act, factors that speed up time and reduce costs in the processes of fertility.
Hysteroscopy in obstetrics
Hysteroscopy also has its place in obstetrics. Hysteroembryoscopy is performed in pregnant women with embryos without cardiac activity, allowing to obtain selective samples of embryonic tissue under direct vision, reducing the risk of contamination by maternal cells20. A more precise view of the external morphology of the embryo is obtained and diagnoses of morphological alterations can be made or diagnostic suspicions confirmed (Figure 4), which are extremely difficult due to do when tissue is destroyed by manual vacuum aspiration or uterine curettage.
Instrumental
For the performance of vaginohysteroscopy there are different operative shirts and reusable surgical instruments. It can be carried out with rigid or flexible instruments, the rigid ones being used more frequently because they provide better images, lower percentage of failed procedures, faster examination time, cheaper acquisition, longer duration and less need for maintenance4,21.
Regarding the rigid operative shirts, the best known is the Bettocchi hysteroscope, an ovalshaped diagnostic-operative shirt, which allows better adaptation to the anatomy of the cervix. There is a 4 mm model and a 5 mm larger diameter model, which use 2 mm and 2.9 mm diameter optics, respectively. Among the new models are Bettocchi Integrated Office Hysteroscope System (B.I.O.H.S.) which has a diameter greater than 4 mm and 2.0 mm optics; it allows the handling and control of the inlet and outlet of liquids with one hand and all the connections are located at the lower end of the handle, to simplify handling22; the field hysteroscope has a sliding mechanism that allows a 2.9 mm first line to be inserted for a better approach to the cervical tract and the uterine cavity, without discomfort for the patient; in the same act, it can slid over the surgical sleeve, changing to a larger diameter and moving from a diagnostic hysteroscopy to an operative one8; each of these operative shirts (Figure 5) has two channels, one for the optics and the other for introducing the reusable 5 Fr surgical instruments, such as the fine tip scissors, blunt tip grasper, biopsy forceps, mono or bipolar electrodes and even diode laser fibers. The small diameter of all these surgical shirts allows the evaluation and treatment of patients who have not started their sexarche - that is, vaginoscopy and extraction of foreign bodies in girls -, and patients with vaginal stenosis due to oncological pathology.
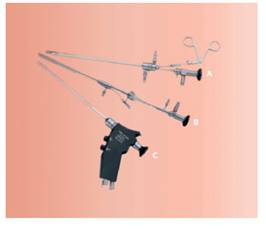
Figure 5 different types of operative sleeves are shown. in descending order (a) bettocchi hysteroscope, (b) field trophyscope, and (c) bettocchi integrated office hysteroscope system (image modified from karl storz hysteroscope catalog diagnostic and surgical procedures for ambulatory hysteroscopy).
The evolution of hysteroscopy is in full swing, with the appearance of new and smaller instruments. Recently, 15 and 16 Fr diameter resectoscopes and morcellators have appeared and even manual morcellators of 5 Fr which can be inserted through the operative channel of the Bettocchi set. These new instruments promise to continue strengthening the current trend of moving the study and treatment of endometrial pathologies to an office environment without anesthesia or sedation.
Means of distension
As the endometrial cavity is a virtual concavity, it requires a means of distension that allows the separation of the uterine walls for its hysteroscopic evaluation. These media can be gaseous, such as carbon dioxide (CO2), electrolyte-free solutions, such as glycine, sorbitol and mannitol, or electrolyte solutions, such as sodium chloride. The choice of the means of distension will depend on the type of energy used. Thus, when using monopolar energy, one of the electrolyte-free solutions is used; if mechanical, bipolar or laser energy is applied, electrolytic solutions are used22, noting that the latter have proven to be the most comfortable and safest means of distension23 by reducing the risk of hyponatremia and vasovagal episodes12 and allow a greater differential between the volume of distention medium entering and leaving the endometrial cavity; this can reach 2 500 mL in patients under 50 years of age without other pathologies8, resulting into longer operative time and resolution capacity.
Factors committing the success of vaginohysteroscopy
Although officinal hysteroscopy is a relatively simple procedure and very well tolerated by patients, between 5 and 15% may present pain of moderate to strong intensity, and around 5% will present a failed access to the uterine cavity, being the main causes cervical stenosis or pain (6). This can lead to the fact that, despite its great advantages, there is a group of patients and gynecologists who are not convinced by vaginohysteroscopy in an outpatient setting.
To try to identify this group of patients who have a higher risk of pain and failed hysteroscopies, it is very important to make an adequate selection and identify risk factors, such as cervical stenosis, menopause, poor visualization of the cervix, absence of vaginal delivery, as well as reinforcing the elements that serve as pain protectors, such as the experience of the operator, surgical time and the diameter and type of equipment used 24. Another important element is to reduce the anxiety of the patient with an adequate explanation of the method before its performance, about the procedure, its advantages, disadvantages, scope and limitations. Based on complete information, you can make a conscious decision whether to have vaginohysteroscopy without or with anesthesia, along with a pleasant environment and constant communication of the hysteroscopist and the patient during the procedure6. These are factors that can contribute to the success of the procedure.
Vaginohisteroscopy in times of covid 19
This year 2020, due to the situation caused by COVID-19, there have been important changes in medical practice. Although information on this virus is still under study, there is evidence of possible viral shedding during minimally invasive gynecological procedures, due to the presence of the virus in the blood, feces and aerosolization of the virus, especially when using smoke generating devices12 and in procedures that require intubation that generate aerosol (AGP). One of the advantages of vaginohysteroscopy is that it is not aerosol-generating and that it allows the option of using mechanical energy, such as scissors and graspers, so the risk of transmission is theoretically low or negligible. These characteristics make vaginohysteroscopy an excellent alternative for the treatment of most endometrial pathologies in this era of COVID-19.
A few months ago the consensus statement of the Global Congress of Hysteroscopy25 was published, in which related recommendations are offered, such as performing adequate triage of the patient, considering requesting the preoperative COVID-19 test -in our case, it is requested per protocol to all patients the days before the procedure in the office-, limit hysteroscopic procedures to those patients in whom their delay could lead to adverse clinical results, minimize the number of people participating in the procedure, favor the use of instruments that do not produce surgical smoke -such as scissors, forceps and tissue recovery systems, as well as the respective decontamination measures after each procedureand the use of appropriate personal protective equipment.
Conclusions
There is no doubt that vaginohysteroscopy is the gold standard for the assessment and treatment of endometrial and endocervical pathologies, allowing the inspection and endoscopic treatment of the uterine cavity and cervical canal in the office using optical and surgical instruments less than or equal to 5 mm in diameter. The small diameter of the instruments makes it a very well tolerated procedure by most patients.
The fact of doing this procedure in the office reduces the time of resolution of the pathologies, since it allows in a single act to see and treat most of the endometrial pathologies, with practically immediate recovery that shortens the periods of rest for the patients; likewise, by avoiding anesthesia and the operating room there is a considerable reduction in costs, making it more accessible to the general population.
As vaginohysteroscopy is a diagnostic and surgical procedure in which the patient will be awake, it is important to take into consideration the theoretical and practical domain of the technique by the hysteroscopist, a pleasant environment that has the conditions and the necessary instruments for its performance and the proper selection of the patient. For this, the antecedents that facilitate or not the entrance to the uterine cavity, the pain threshold and the willingness of the patient to collaborate during the procedure must be assessed. It is essential that the patient has clear information about what vaginohysteroscopy is, what she may feel while it is being performed, its advantages, disadvantages, scope, limitations and risks, all of which will help her to collaborate consciously during the performance of this in office technique.
REFERENCES
1. Filiz T, Doger E, Corakçi A, Ozeren S, Caliskan E. The efficacy, cost and patient satisfaction of classic versus office hysteroscopy in cases with suspected intrauterine space occupying lesions with 3-dimension ultrasound and abnormal uterine bleeding. J Turk Ger Gynecol Assoc. 2009 Dec 1;10(4):189-93. PMID: 24591870. [ Links ]
2. Instituto Mexicano del Seguro Social. Recomendaciones en histeroscopia. 2011. http://www.cenetec.salud.gob.mx/descargas/gpc/CatalogoMaestro/585_GPC_/585GER.pdf [ Links ]
3. Amer-Cuenca JJ, Marín-Buck A, Vitale SG, La Rosa VL, Caruso S, Cianci A, et al. Non-pharmacological pain control in outpatient hysteroscopies. Minim Invasive Ther Allied Technol. 2020 Feb;29(1):10-19. doi: 10.1080/13645706.2019.1576054 [ Links ]
4. Royal College of Obstetricians and Gynaecologists. Best practice in outpatient hysteroscopy. RCOG Green-top Guideline No. 59 March 2011. [ Links ]
5. Di Spiezio Sardo A, Calagna G, Di Carlo C. Tips and tricks in office hysteroscopy, Gynecology and Minimally Invasive Therapy. 2015;4(1):3-7. ISSN 2213-3070. https://doi.org/10.1016/j.gmit.2014.12.004 [ Links ]
6. Alonso L. The endocervical canal strategies for an easy access to the uterine cavity. Hysteroscopy Newsletter. 2019;5(4). [ Links ]
7. Bettocchi S, Selvaggi L. A vaginoscopic approach to reduce the pain of office hysteroscopy. J Am Assoc Gynecol Laparosc. 1997 Feb;4(2):255-8. doi: 10.1016/s1074-3804(97)80019-9 [ Links ]
8. ACOG Technology Assessment No. 13: Hysteroscopy. Obstet Gynecol. 2018 May;131(5):e151-e156. doi: 10.1097/AOG.0000000000002634 [ Links ]
9. Bennett A, Lepage C, Thavorn K, Fergusson D, Murnaghan O, Coyle D, et al. Effectiveness of outpatient versus operating room hysteroscopy for the diagnosis and treatment of uterine conditions: A systematic review and meta-analysis. J Obstet Gynaecol Can. 2019 Jul;41(7):930-41. doi: 10.1016/j.jogc.2018.10.002 [ Links ]
10. Parry JP, Isaacson KB. Hysteroscopy and why macroscopic uterine factors matter for fertility. Fertil Steril. 2019 Aug;112(2):203-10. doi: 10.1016/j.fertnstert.2019.06.031 [ Links ]
11. Yang JH, Chen MJ, Yang PK. Factors increasing the detection rate of intrauterine lesions on hysteroscopy in infertile women with sonographically normal uterine cavities. J Formos Med Assoc. 2019 Jan;118(1 Pt 3):488-93. doi: 10.1016/j.jfma.2018.08.017 [ Links ]
12. Yen CF, Chou HH, Wu HM, Lee CL, Chang TC. Effectiveness and appropriateness in the application of office hysteroscopy. J Formos Med Assoc. 2019 Nov;118(11):1480-7. doi: 10.1016/j.jfma.2018.12.012 [ Links ]
13. Bristish Society of Gynaecological Endoscopy (BSGE) Newsletter of the British Society for Gynaecological Endoscopy. The Scope Internet vol. 20 (2018). https://28x8koygrj92snigkorkjod2-wpengine.netdna-ssl.com/wcontent/uploads/2019/02/The-Scope-Issue 11_web.pdf [ Links ]
14. National Collaborating Centre for Women's and Children's Health (UK). Heavy Menstrual Bleeding. London: RCOG Press; 2007 Jan. PMID: 21938862. [ Links ]
15. Jain S, Inamdar DB. Manual of Fertility Enhancing Hysteroscopy. Library of Congress Control Number: 2018937589. Singapore: Springer Nature Singapore Pte Ltd. 2018. [ Links ]
16. Remohí Giménez J, Bellver Pradas J, Ferrando Serrano M, Requena Miranda A, Pellicer Martínez A. Manual Práctico de Esterilidad y Reproducción Humana. Aspectos Clínicos. 5ª Edición. Madrid: Editorial Médica Panamericana. 2018. [ Links ]
17. Smit JG, Kasius JC, Eijkemans MJC, Koks CAM, van Golde R, Nap AW, et al. Hysteroscopy before in-vitro fertilisation (inSIGHT): a multicentre, randomised controlled trial. Lancet. 2016 Jun 25;387(10038):2622-9. doi: 10.1016/S0140-6736(16)00231-2. Erratum in: Lancet. 2019 Jun 15;393(10189):2394. PMID: 27132052. [ Links ]
18. El-Toukhy T, Campo R, Khalaf Y, Tabanelli C, Gianaroli L, Gordts SS, et al. Hysteroscopy in recurrent in-vitro fertilisation failure (TROPHY): a multicentre, randomised controlled trial. Lancet. 2016 Jun 25;387(10038):2614-2621. doi: 10.1016/S0140-6736(16)00258-0 [ Links ]
19. Di Spiezio Sardo A, Di Carlo C, Minozzi S, Spinelli M, Pistotti V, Alviggi C, et al. Efficacy of hysteroscopy in improving reproductive outcomes of infertile couples: a systematic review and meta-analysis. Hum Reprod Update. 2016 Jun;22(4):479-96. doi: 10.1093/humupd/dmw008 [ Links ]
20. Campos-Galindo I, García-Herrero S, Martínez-Conejero JA, Ferro J, Simón C, Rubio C. Molecular analysis of products of conception obtained by hysteroembryoscopy from infertile couples. J Assist Reprod Genet. 2015 May;32(5):839-48. doi: 10.1007/s10815-015-0460-z [ Links ]
21. Unfried G, Wieser F, Albrecht A, Kaider A, Nagele F. Flexible versus rigid endoscopes for outpatient hysteroscopy: a prospective randomized clinical trial. Hum Reprod. 2001 Jan;16(1):168-171. doi: 10.1093/humrep/16.1.168 [ Links ]
22. Federación Latinoamericana de Obstetricia y Ginecología - FLASOG. Cirugía Mínimamente Invasiva en Ginecología, Altavoz Editores, noviembre 2017. [ Links ]
23. del Valle C, Solano JA, Rodríguez A, Alonso M. Pain management in outpatient hysteroscopy. Gynecology and Minimally Invasive Therapy. 2016;5(4):141-7. ISSN 2213-3070. [ Links ]
24. Díaz-Yamal IJ, Uscátegui-Diago AM, Castañeda-Castañeda J, Fandiño-Rodríguez CA, Villamil-Pérez JE, Gómez-Corredor F, et al. Seguridad de la histeroscopia oficinal en una unidad de fertilidad. Bogotá, Colombia, 2011-2016. Cohorte retrospectiva. Rev Colomb Obstet Ginecol. [Internet]. 2017;68(3):186-92. http://dx.doi.org/10.18597/rcog.776 [ Links ]
25. Carugno J, Di Spiezio Sardo A, Alonso L, Haimovich S, Campo R, De Angelis C, et al. COVID-19 Pandemic. Impact on hysteroscopic procedures: a consensus statement from the Global Congress of Hysteroscopy Scientific Committee. J Minim Invasive Gynecol. 2020 Jul-Aug;27(5):988-92. doi: 10.1016/j.jmig.2020.04.023 [ Links ]
Cite as:Goncalves Rodríguez JL,Escudero Velando LE, Velit Suarez M, Ascenzo Battistini M, Bonomini Catanzaro C, Bozzo Pancorvo R, Coronel Bravo H. Vagino hysteroscopy, diagnosis and treatment of endometrial pathologies in office. Rev Peru Ginecol Obstet. 2021;67(1). DOI: https://doi.org/10.31403/rpgo.v67i2303
Received: July 27, 2020; Accepted: November 20, 2020











 texto en
texto en