Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Ginecología y Obstetricia
On-line version ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.67 no.1 Lima Jan-Mar 2021
http://dx.doi.org/10.31403/rpgo.v67i2306
Case Report
Abdominal ectopic pregnancy: Report of two cases
1 Gynecologist and Obstetrician, Hospital Nacional Edgardo Rebagliati Martins, EsSalud, Lima, Peru
We present two cases of abdominal ectopic pregnancy of 16 and 26 weeks, evaluated with ultrasound and magnetic resonance imaging. Both cases presented an acute surgical abdomen, the case with the oldest gestational age showed hemodynamic decompensation due to hemoperitoneum secondary to placental abruption. The clinical presentation led to resolution by laparotomy and extraction of the fetus and placental tissue, ending in hysterectomy due to trophoblastic involvement of the uterine surface and adjacent organs in the first case. The 26-week-neonate died after 4 months due to late sepsis. Clinical suspicion for amenorrhea and severe abdominal pain are important criteria, and imaging studies, especially ultrasound, are the main diagnostic tools.
Key words: Abdominal pregnancy
Introduction
Abdominal pregnancy is defined as an ectopic embryonic implantation that occurs in the peritoneal cavity. It is a rare condition, with an estimated incidence of 1/10,000 births and in 1.4% of ectopic pregnancies(1). Most ectopic pregnancies are a result of reimplantation of a tubal abortion (secondary), and the most frequent site of implantation is para-adnexal1. There are various, nonspecific symptoms associated with this pathology which are dependent on the location and gestational age of the fetus. These range from asymptomatic cases that progress to or beyond the second trimester, to those with nonspecific symptoms and abdominal pain that could result in hypovolemic shock due to the rupture of abnormally implanted placental vessels2,3,4.
Ultrasound is the gold standard for diagnosis of ectopic pregnancy with a specificity and sensitivity previously described as 94% and 87% respectively2. The abdominal-pelvic nuclear magnetic resonance imaging (MRI) may help guide the involvement of adjacent organs.
Management depends on maternal symptoms and fetal status. In many cases, emergency laparotomy is the chosen technique, as the patient may present acute, severe intra-abdominal haemorrhage due to placental separation of the implantation bed. Due to the extreme risk of complications and associated maternal mortality of up to 5 per 1000 cases4, some experts recommend surgical intervention as soon as the diagnosis has been made5. Cases of conservative management are usually isolated6 and fetal mortality can reach more than 50%. Abdominal pregnancy has also been associated with congenital malformations in about 20% of neonates7.
This study presents two complicated cases of abdominal pregnancy at 16 and 26 weeks in a social healthcare hospital of Peru, and we performed a literature review regarding the approach and treatment of this entity.
Case reports
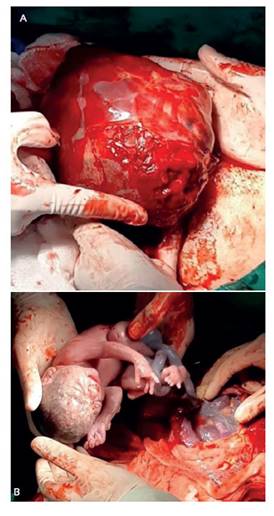
Case 1 involved a 35-year-old patient (gravida 2, para 1) referred at 16 weeks, with severe abdominal pain without genital bleeding. A transvaginal and abdominal ultrasound was performed, detecting a 13 × 7 cm myomatous uterus, empty uterine cavity and fetal bone structures without cardiac activity adjacent to the uterus. The magnetic resonance imaging is shown in Figure 1 An exploratory laparotomy was performed, which found a heterogeneous mass protected by omentum adjacent to the right uterine lateral wall. Subsequently, the chorioamniotic membranes was released and a stillbirth of 120 gr was removed. The placenta was separated from the omentum and the intestinal serosa, finding choriodecidual fragments firmly attached to the adnexa and uterus, so a total hysterectomy was performed. The post-surgical progression was favourable and the patient was discharged on the seventh day.
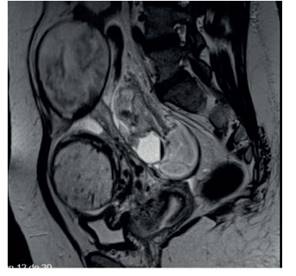
Figure 1 Case 1: pelvic mr: image compatible with abdominal extrauterine pregnancy with invasion of the placenta to the pelvic surface.
Case 2. involved a 37-year-old patient, (gravida 6, para 2) referred at 24 weeks to our hospital with painful abdominal syndrome due to cholecystitis. The general surgery service planned an expectant management. The symptoms persisted, and during the evolution the patient presented a decrease in hematocrit and severe anemia (hemoglobin: 6.9 g). An obstetric ultrasound was performed by our service which showed a 26-week-old active fetus located on the right flank, with a posterior placenta without myometrial lining, and an unoccupied 13 cm uterus associated with free fluid in the peritoneal cavity (Figure 2). Magnetic resonance imaging findings are shown in Figure 3. Hemoglobin was optimized, fetal lung maturation with corticosteroids and fetal neuroprotection with magnesium sulphate were indicated. An exploratory laparotomy was performed which found two litres of hemoperitoneum and a live female fetus of 710 gr, Apgar score 61 and 75, wrapped by the chorionic membranes of approximately 18 cm in diameter. The placenta was posterior and lying on the broad ligament, which presented a 6 cm rupture on the high posterior side, with active bleeding from the uterine nutrient vessel, without involvement of the abdominal organs (Figure 4); it was removed en bloc. The surgical service referred the patient back for cholecystectomy on the sixth postoperative day, due to persistent abdominal pain. The progression was favourable, and she was discharged on the sixth day following the cholecystectomy. The neonate exhibited necrotising enterocolitis with bronchopulmonary dysplasia. Furthermore, a persistent ductus arteriosus, intraventricular haemorrhage and retinopathy due to extreme prematurity, caused the newborn’s death at 4 months 4 days from late sepsis.

Figure 2 Case 2: a: fetus and placenta without surrounding myometrium and hemoperitoneum. b: fetus and empty uterus in sagittal view
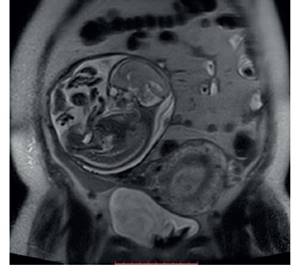
Figure 3 Case 2: Mri t2, maternal coronal plane: chorioamniotic sac in extrauterine position with normal fetal content. empty uterus.
Discussion
We highlight two cases of abdominal ectopic pregnancy, the first with an early second trimester fetal death and the second showing a 26-week live fetus, both with similarity with respect to clinical pictures, imaging findings and approach. Following Studdiford’s criteria established in 1946, both were secondary abdominal pregnancies because of tubal involvement and placental uterus fistula. Amenorrhea and abdominal-pelvic pain were the main maternal symptoms in both cases. The second case was confused with biliary pathology, which was the reason for referral to our institution. Ultrasonography is generally used for diagnosis and guiding signs included an empty uterus, a poor placental definition and an unusual fetal attitude. It was also essential to determine the absence of myometrial tissue between the pregnancy and the bladder and adjacent organs, which serves to differentiate advanced abdominal pregnancies from intrauterine ones8.
MRI is useful in these cases to assess the extent of placental involvement to adjacent organs9. Advanced abdominal pregnancies are defined as those that exceed 20 weeks of gestation and their main management dilemma is in relation to placental management once the fetus has been removed. Nunyalulendho reported 163 cases from 1946 to 2008, with a preoperative diagnosis of less than 50%7). Masukume included 38 cases of advanced abdominal pregnancies with live fetuses in the period between 2008 to 201310 and Minakshi Rohilla reviewed cases from 2013 to 2018, reporting 26 cases of advanced abdominal pregnancies with better preoperative diagnostic rates (56%)11). Term cases have been described as incidental intraoperative findings, even in our setting12.
There is no standardised protocol for the management of this pathology. These are usually interrupted at the time of diagnosis because of the high risk of maternal complications, although expectant behaviour has been considered in asymptomatic cases, hoping for viability13. The maximum gestational age for these cases, according to reports, is from 32 to 34 weeks (consensus is not to exceed the gestational age limit at which fetal viability is reached), when an exploratory laparotomy is scheduled considering catheterisation of pelvic vessels to control intraoperative hemorrhage. The most frequent maternal complications after surgery include hemorrhage and infection with a maternal mortality rate of 12% in these cases7. Regarding the management of placental tissue, its complete excision is easier the smaller the pregnancy. Even laparoscopic treatment could be considered in these cases and the association with uterine vessel embolization has also been described14.
In the first case presented, the placental involvement included intestinal loops and the uterine wall, leading to a hysterectomy. In the second case, the implantation in the peritoneum allowed en bloc evacuation which involved the right tube, conserving the uterus. In cases where complete placental extraction is not possible, conservative management is an option which involves leaving the placenta in situ and it is recommended to double check for the possibility of maternal complications such as abscesses, late bleeding and obstruction of hollow viscera as a result of secondary inflammatory and necrotic phenomena15.
The use of methotrexate for the post-operative management of placental reduction is discussed and experts recommend placental extraction, which is possible in 55%-75% of cases11. Escobar 16 reports 74 cases of advanced abdominal pregnancy including 25 cases with expectant management (median latency of 6.1 weeks) with neonatal survival rates of 56%; the placenta could be removed in 58% of cases and maternal mortality due to hemorrhage was of 4%.
In conclusion, abdominal ectopic pregnancy is a rare condition with high maternal-fetal mortality rate and has led to marked variability concerning therapeutic approach. Ultrasonography and MRI support is useful for diagnosis and planning of the appropriate surgical approach. The most frequent form of presentation is the acute abdomen secondary to hemoperitoneum, which can turn the condition into a gynecological emergency that demands a hospital resources with high resolution capacity for its successful management.
REFERENCES
1. Okafor I, Ude AC, Aderibigbe ASO, Amu OC, Udeh PE, Obianyo NEN, Ani COC. Abdominal pregnancy a case report. J West Afr Coll Surg. 2011;1:121-30. PMID: 25452947 [ Links ]
2. Audifred JR, Herrera A, Gonzalez MG. Embarazo ectópico intraligamentario. Ginecol Obstet Mex. 2013;81:211-4. [ Links ]
3. Sunday-Adeoye I, Twomey D, Egwuatu EV. A 30-year review of advanced abdominal pregnancy at the Mater Misericordiae Hospital, Afikpo, southeastern Nigeria (19762006). Arch Gynecol Obstet. 2011;283:19-24. doi 10.1007/s00404-009-1260-44 [ Links ]
4. Roberts RV, Dickinson JE, Leung Y. Advanced abdominal pregnancy: still an occurrence in modern medicine. Aust N Z J Obstet Gynaecol. 2005; 45: 518-521. doi 10.1111/j.1479-828X.2005.00489.x [ Links ]
5. Naim NM, Ahmad S, Siraj HH, Ng P, Mahdy ZA. Advanced abdominal pregnancy resulting from late uterine rupture. Obstet Gynecol. 2008;111(2 Pt 2):502-4. doi 10.1097/01.AOG.0000279451.51446.c1 [ Links ]
6. Díaz M. Embarazo abdominal a término: reporte de un caso. Rev Colomb Obstet Ginecol. 2002;53(1):93-5. doi https://doi.org/10.18597/rcog.656 [ Links ]
7. Nunyalulendho DN, Einterz EM. Advanced abdominal pregnancy: case report and review of 163 cases reported since 1946. Rural Remote Health. 2008;8:1087. PMID: 19053177 [ Links ]
8. Onan MA, Turp AB. Primary omental pregnancy: case report. Hum Reprod. 2005;20:807-9. doi 10.1093/humrep/deh683 [ Links ]
9. Yoshigi J, Yashiro N, Kinoshito T. Diagnosis of ectopic pregnancy with MRI: efficacy of T2-weighted imaging. Magn Reson Med Sci. 2006;5:25-32. doi 10.2463/mrms.5.25 [ Links ]
10. Masukume G. Live births resulting from advanced abdominal extrauterine pregnancy, a review of cases reported from 2008 to 2013. WebmedCentral Obstet Gynaecol. 2014;5(1):WMC004510. doi 10.9754/journal.wmc.2014.004510 [ Links ]
11. Minakshi R, Bharti J, Vanita J. Advanced abdominal pregnancy: a search for consensus. Review of literature along with a case report. Arch Gynecol Obstet. 2018;298(1):1-8. doi 10.1007/s00404-018-4743-3 [ Links ]
12. Gamboa J, Ayala F, Oros V. Presentación de un caso de embarazo ectópico abdominal a término con evolución favorable madre-niño. Rev Peru Matern Perinat. 2012;1(1):62-5. [ Links ]
13. Mpogoro F, Gumodoka B. Managing a live advanced abdominal twin pregnancy. Ann Med Health Sci Res. 2013;3:113-5. doi 10.4103/2141-9248.109472 [ Links ]
14. Oneko O, Petru E. Management of the placenta in advanced abdominal pregnancies at an East african tertiary referral center. J Womens Health. (Larchmt). 2010;19(7):1369-75. doi 10.1089/jwh.2009.1704 [ Links ]
15. Cetinkaya MB, Kokcu A. Follow up of the regression of the placenta left in situ in an advanced abdominal pregnancy using the Cavalieri method. J Obstet Gynaecol Res. 2005;31:22-6. doi 10.1111/j.1447-0756.2005.00236.x [ Links ]
16. Escobar, Caicedo-Herrera. Embarazo ectópico abdominal avanzado: reporte de dos casos y revisión de la literatura. Rev Colomb Obstet Ginecol. 2017;68(1):71-82. doi 10.18597/rcog.2983- [ Links ]
Received: October 19, 2020; Accepted: December 20, 2020











 text in
text in