Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.67 no.1 Lima ene./mar 2021
http://dx.doi.org/10.31403/rpgo.v67i2307
Case Report
Giant uterine arteriovenous malformation. A case report
1. Hospital Nacional Daniel Alcides Carrión, Callao, Peru
2. Fetal Medicine Center: CENMEF, Grupo de Medicina Materno Fetal: Fetalis
The case of a patient who presented with abnormal uterine hemorrhage due to an acquired arteriovenous malformation diagnosed with Doppler ultrasound and magnetic resonance is presented. This pathology is becoming more and more frequent and with serious consequences, if proper and timely management is not given.
Key words: Uterus; Vascular malformations; Congenital anomalies; Uterine hemorrhage
Introduction
Uterine arteriovenous malformation (UAVM), previously called arteriovenous fistula or cirsoid aneurysm, was first reported by Dubreuil and Loubat in 19261. It has an unknown incidence, but it is more frequent than estimated. There are few documented cases and series in the literature.
UAVM can be classified as congenital or acquired, the most common being acquired UAVM. Congenital UAVM develops due to failure in the embryological differentiation of primitive vascular structures, resulting in the creation of abnormal vascular connections that tend to extend beyond the margins of the uterus into the pelvis2. Acquired UAVM has an unclear origin, but is related to episodes of endometrial trauma with the presence of trophoblastic tissue (uterine curettage, uterine surgeries such as cesarean section, placenta accreta, gestational trophoblastic disease or vaginal delivery). It appears as multiple vascular connections of variable size between arteries and veins, which are usually focused on the area in relation to the triggering factor3-5.
We present the unusual case of an acquired UAVM which involved the entire myometrium of the uterine corpus and presented with severe uterine bleeding.
Case report
40-year-old patient with obstetric history of first vaginal delivery 20 years ago, without complications. Cesarean section 16 years ago due to eclampsia and 6 years since an incomplete abortion complicated with severe anemia, which required transfusion of 2 globular packets prior to endometrial manual vacuum aspiration (MVA). Five years ago, there was a new incomplete abortion treated with MVA, without complications. In both cases, the anatomopathological study corresponded to placental and decidual remains.
The patient visited an outpatient clinic 8 months ago due to abnormal uterine bleeding (AUB) of two months of evolution. Initial ultrasound studies (at another medical institution) considered the diagnoses of uterine leiomyomata, adenomyosis and endometrial thickening. She underwent hysteroscopy 6 months ago, without finding major alterations in the cavity. The abnormal uterine bleeding persisted in the patient, and a new ultrasound revealed thickened and heterogeneous myometrium and thin endometrium of difficult delimitation (Figure 1A). There were hypoechoic myometrial areas that showed global increase in vascularity on Doppler study (Figures 1B and 2); these vessels showed a peak systolic velocity PSV) of 47.33 cm/sec (Figure 2B). Uterine sarcoma or giant uterine arteriovenous malformation was proposed as a diagnosis.
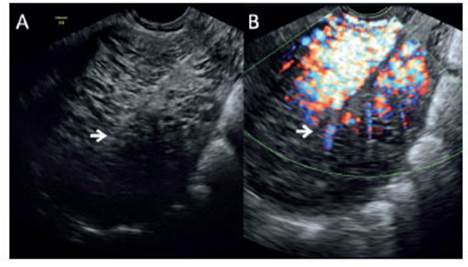
Figure 1 A. Ultrasonography of the uterus in sagittal section, showing thickened and heterogeneous myometrium. The arrow points to the endometrium, which is difficult to differentiate. B. Ultrasonography with HD power Doppler, showing considerable increase in vascular flow throughout the endometrial thickness.
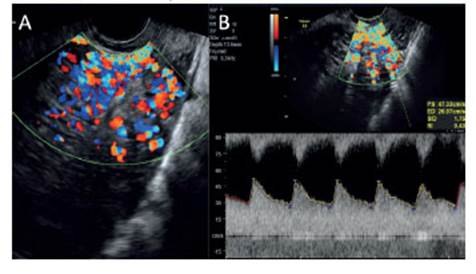
Figure 2 A. Pulsed Doppler ultrasound shows abundant multidirectional vascularity throughout the endometrial thickness. B. Spectral wave of abnormal myometrial vessels, with systolic peak at 47.33 cm/s, low resistance index at 0.43.
Magnetic resonance imaging revealed thickening of the myometrium, with marked increase in contrast uptake throughout the uterine muscle and the uterine vessels of the broad ligament, with no evidence of endometrial tumors or pathology (Figure 3). A few days later, she presented an episode of massive uterine bleeding with severe symptomatic anemia that required a transfusion of 2 globular blood packets. Once stabilized and due to the severity of the condition, the patient was scheduled for an emergency abdominal hysterectomy. During the surgical act, a uterus of approximately 15 cm was found, dilated and tortuous uterine vessels of the broad ligament, intraoperative bleeding of 2 800 mL, for which she received multiple blood products.
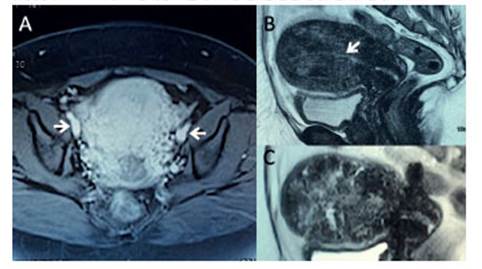
Figure 3 A. Magnetic resonance with contrast in the axial section; there is evidence of dilated broad ligament vessels and enlarged uterine arteries (white arrow). B and C. Sagittal resonance section shows globally thickened myometrium, heterogenous with hypointense areas and lineal endometrial cavity.
The postoperative period was uneventful. The pathological anatomy of the surgical specimen referred to acquired arteriovenous malformation. Macroscopically, the thickened myometrium was observed, with vessels of diverse caliber, with the exception of the cervix and isthmus (Figure 4A). Microscopy showed multiple myometrial vessels of variable morphology, different caliber, and walls of irregular thickness (Figure 4B)
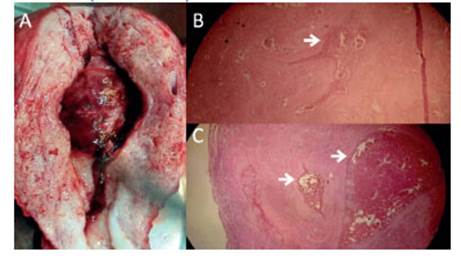
Figure 4 A. Anatomical pa rt of the uterus, thickened myometrium with increased vascularity (reddish coloration), whitish cervix without alterations, uterine cavity occupied by tissue with a hematic appearance. Figures B and C. Histological sections of the myometrium show vessels with variable morphology and caliber, with walls of irregular thickness surrounded by fibrosis (white arrows).
Discussion
Arteriovenous malformation is a shunt formed by abnormal communication between branches of the uterine artery and the myometrial venous plexuses1,2. Mulliken and Glowacki consider UAVM as tortuous vascular canals of different sizes and shapes, covered by a continuous endothelium and surrounded by an abnormal complement of mural cells. Müngen considers that, in acquired cases, variable vascularity and increased fibrosis are associated with myometrial retention of conceptional remains (trophoblast)2,6,7.
The suspicion of UAVM is established by abnormal uterine bleeding that, on transvaginal ultrasound, shows an area of heterogeneity in the uterine muscle, such as irregular anechoic spaces of different sizes, usually grouped and close to the endometrium7-9. When using Doppler, be it color or power, a ball with multidirectional flow is evidenced that corresponds to the anechoic areas mentioned above (Figures 1B and 2A). The high velocity in these abnormal vessels generates a vascular mosaic image typical of arteriovenous shunts in 95% of cases. There are high peaks in systolic velocity with a low index of resistance and pulsatility, a characteristic finding of this condition10 (Figures 1 and 2).
Kamaya classifies the vascularization of the uterus with UAVM studied with Doppler in: a) type 0: remains of the conception retained without vascularization; b) type 1: uterine content with minimal vascularity; c) type 2: moderate vascularization; and, d) type 3 extensive vascularity11,12. Van den Bosch uses the term "enhanced myometrial vascularity" to Doppler examination when it comes to retention of conception remains. It seems reasonable to use it as an integral term for the description of UAVM, as the ultrasound image is similar, regardless of the associated pathology2,8,11,13.
Although these patients usually remain asymptomatic, it is common for them to present uterine bleeding that is generally painless and unspecific. It should be suspected when, before an invasive procedure (uterine curettage, endometrial biopsy) the bleeding is profuse without a clear explanation. For this reason, its search is essential when ultrasound studies in patients with bleeding and a close history of pregnancy or abortion, before submitting them to procedures6,7,13.
Arteriography is considered the gold standard for definitive diagnosis. However, various studies have shown that transvaginal ultrasound and Doppler study are simple, reproducible and cost-effective diagnosis modalities10,14,15. Tomography and resonance can in selected cases provide differential diagnoses and the extent of pelvic vascularity; they may be recommended, but they are not always necessary.
Broadly speaking, the management of asymptomatic patients is medical (control, gesta-gens, methylergonovine, combined contraceptives). Patients with recurrent episodes will have surgical indication (hysterectomy, laparoscopic hypogastric artery ligation or hysteroscopy), especially those with massive refractory bleeding, as was the case presented. Selective distal embolization of the uterine arteries is currently recommended in patients who wish to preserve fertility, with a success rate greater than 93%16.
One way to choose management is based on the vascular behavior of the UAVM. If the VPS values are below 40 cm/sec, the course is considered less risky. The signs and symptoms are generally subject to periodic monitoring2,13,15,17. If the patients present SPV between 40 and 60 cm/sec, they can have medical management, as long as they remain asymptomatic. However, if the velocities are greater than 60 or 70 cm/sec, they are candidates for treatment with uterine artery embolization or surgical treatment2,7,9. What was abnormal in the case presented was the heavy vaginal bleeding with low SPV; perhaps the general extension of the lesion could explain this behavior.
Capmas reports the only published case of an extensive UAVM that covered the entire myometrium, showing areas of hypervascularity, turbulent flow, and high systolic velocity. After failure of conservative management, they opted for hysterectomy18. The present case shows similarity in the vascular compromise of the entire myometrium, with similar Doppler flow images and clinical course.
Although UAVM is a rare, the potential complications of not being diagnosed require a search in cases of AUB, always before surgical procedures related to recent abortions.
REFERENCES
1. Fleming H, Ostör AG, Pickel H, Fortune DW. Arteriovenous malformations of the uterus. Obstet Gynecol. 1989;73:209. PMID: 2643064 [ Links ]
2. Timor-Tritsch IE, Haynes MC, Monteagudo A, Khatib N, Kovács S. Ultrasound diagnosis and management of acquired uterine enhanced myometrial vascularity/arteriovenous malformations. Am J Obstet Gynecol. 2016;214(6):731. e1-731.e10. DOI:10.1016/j.ajog.2015.12.024 [ Links ]
3. Ghai S, Rajan DK, Asch MR, Muradali D, Simons ME, TerBrugge KG. Efficacy of embolization in traumatic uterine vascular malformations. J Vasc Interv Radiol. 2003;14(11):1401-8. DOI: 10.1097/01.rvi.0000096761.74047.7d [ Links ]
4. Peitsidis P, Manolakos E, Tsekoura V, Kreienberg R, Schwentner L. Uterine arteriovenous malformations induced after diagnostic curettage: a systematic review. Arch Gynecol Obstet. 2011;284(5):1137-51. DOI: 10.1007/s00404-011-2067-7 [ Links ]
5. Grivell RM, Reid KM, Mellor A. Uterine arteriovenous malformations: a review of the current literature. Obstet Gynecol Surv. 2005;60:761-7. DOI: 10.1016/j.gyobfe.2011.08.013 [ Links ]
6. Nasu K, Fujisawa K, Yoshimatsu J, Miyakawa I. Uterine arteriovenous malformation: ultrasonographic, magnetic resonance and radiological findings. Gynecol Obstet Invest. 2002;53(3):191-4. DOI: 10.1159/000058373 [ Links ]
7. Huang MW, Muradali D, Thurston WA, Burns PN, Wilson SR. Uterine arteriovenous malformations: gray-scale and Doppler US features with MR imaging correlation. Radiology. 1998;206(1):115-23. DOI:10.1148/radiology.206.1.9423660 [ Links ]
8. Flynn MK, Levine D. Non-invasive diagnosis and management of a uterine arteriovenous malformation. Obstet Gynecol. 1996;88:650. doi: 10.1016/0029-7844(96)00122-6 [ Links ]
9. Rosa C, De Aguiar F, Japur A, Reis F, Poli O, Nogueira A. Conservative management of large uterine arteriovenous malformation: case report. Fertil Steril. 2008;90:2406-7. DOI: 10.1016/j.fertnstert.2008.01.097 [ Links ]
10. Szpera-Gozdziewicz A, Gruca-Stryjak K, Breborowicz GH, Ropacka-Lesiak M. Acquired uterine arteriovenous malformation - a diagnostic dilemma. Ginekol Pol. 2018;89(4):227- 8. doi:10.5603/GP.a2018.0039 [ Links ]
11. Zhu YP, Sun ZJ, Lang JH, Pan J. Clinical characteristic and management of acquired uterine arteriovenous malformation. Chin Med J (Engl). 2018;131(20):2489-91. DOI:10.4103/0366-6999.243570 [ Links ]
12. Kamaya A, Petrovitch I, Chen B, Frederick CE, Jeffrey RB. Retained products of conception: spectrum of color Doppler findings. J Ultrasound Med 2009;28:1031-41. DOI: 10.7863/jum.2009.28.8.1031 [ Links ]
13. Timmerman D, Van den Bosch T, Peeraer K, Debrouwere E, Van Schoubroeck D, Stockx L, et al. Vascular malformations in the uterus: ultrasonographic diagnosis and conservative management. Eur J Obstet Gynecol Reprod Biol. 2000;92(1):171-8. doi:10.1016/s0301-2115(00)00443-7 [ Links ]
14. Polat P, Suma S, Kantarcy M, Alper F, Levent A. Color Doppler US in the evaluation of uterine vascular abnormalities. Radiographics 2002;22:47-53. doi:10.1148/radiographics.22.1.g02ja0947 [ Links ]
15. Lacunza RO. Uterine arteriovenous malformation as a non-frequent cause of abnormal uterine hemorrhage. Case report. Rev Peru Ginecol Obstet. 2013;59:203-6. [ Links ]
16. Grivell RM, Reid KM, Mellor A. Uterine arteriovenous malformations: a review of the current literature. Obstet Gynecol Surv 2005;60: 761-7. DOI: 10.1016/j.gyobfe.2011.08.013 [ Links ]
17. Syla B, Fetiu S, Tafarshiku S. Transabdominal two-and-three-dimensional color Doppler imaging of a uterine arteriovenous malformation. Ultrasound Obstet Gynecol. 2011;37:376-8. DOI: 10.1002/uog.8918 [ Links ]
18. Capmas P, Levaillant JM, Teig B, Fernandez H. Uterine arteriovenous malformation involving the whole myometrium. Ultrasound Obstet Gynecol. 2013;41(6):715-7. doi:10.1002/uog.12432 [ Links ]
Received: July 08, 2020; Accepted: November 09, 2020











 texto en
texto en 



