Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.67 no.1 Lima ene./mar 2021
http://dx.doi.org/10.31403/rpgo.v67i2312
Case Report
Non-puerperal uterine inversion: first case reported in Peru
1. Maternal and Child Department, Hospital III Suarez, Angamos, EsSalud, Lima, Peru
Non-puerperal uterine inversion is very rare. A case associated with leiomyomatosis is reported. The case of a 45-year-old multiparous woman with severe vaginal bleeding, pelvic pain and vaginal foreign body sensation is presented. Uterine leiomyoma in abortive phase was diagnosed. She was scheduled for myomectomy with probable abdominal hysterectomy and complete uterine inversion was found. This report is an anecdotal case of non-puerperal uterine inversion, whose surgical treatment was successful.
Key words: Uterine inversion; Uterine hemorrhage; Leiomyomatosis; Uterine myomectomy
Introduction
Non-puerperal uterine inversion is a rare event in daily gynecological practice. Many specialists do not witness this entity in their medical working life. Uterine inversion1 is defined as the exit of the endometrial aspect of the uterus through the vagina. It is classified as partial or complete, according to its magnitude, and as acute or chronic according to the time in which it manifests itself. It occurs more frequently after an obstetric episode, with an incidence of 1 in 3 500 vaginal deliveries 2. The manifestation outside pregnancy is extremely rare, so much so that there is no reliable estimate of its incidence in the medical literature, and reports in Peru are neither described nor available2,3. The pre-operative diagnosis is not usually easy, the most common cause being a submucosal myoma. However, other causes can be malignant uterine tumors or idiopathic presentations4. In most cases management is surgical and consists of vaginal or abdominal hysterectomy. We describe a case of non-puerperal uterine inversion concomitant with a submucosal uterine leiomyoma, whose surgical treatment was successful.
Case report
She was a 42-year-old female patient from Lima, Peru, a housewife, with no significant personal or family history. Her gynecological-obstetric history was menarche at 12 years of age, menstruation every 28 to 30 days, multiparous (4 vaginal deliveries), not a contraceptive method user, with negative cervical cytology. The current disease started 10 months prior to her care, with episodes of hypermenorrhea associated with dysmenorrhea. Outpatient transvaginal ultrasound showed intramural leiomyoma 5 cm in diameter at fundal level. She was prescribed oral contraceptives, analgesics and expectant management.
The patient presented multiple admissions to the emergency service for the same symptomatology, so it was decided to prepare her for surgery, which was deferred for COVID emergency health reasons (March 2020). In July 2020, she went to the emergency department for severe pelvic pain, heavy vaginal bleeding, dysuria and foreign body sensation in the vagina. On evaluation she presented normal nutritional status and severe pallor was evident. On gynecological examination, the uterus was palpated, measuring approximately 15 cm, and a fleshy mass of 10 cm in diameter was observed protruding through the external genitalia, with apparent presence of cervical pedicle. She was hospitalized for study and treatment. During her hospitalization she presented with decreased vaginal bleeding, severe anemia (hemoglobin 4.5 g/dL) and urinary sepsis, being transferred to the intensive care unit for management with broad-spectrum antibiotic therapy, vasopressors and blood transfusion.
She presented favorable evolution and was scheduled for surgical treatment for probable abortive leiomyoma. Among the imaging tests requested, vaginal ultrasound and pelvic tomography showed the aforementioned mass, but were unsatisfactory for a definitive diagnosis.
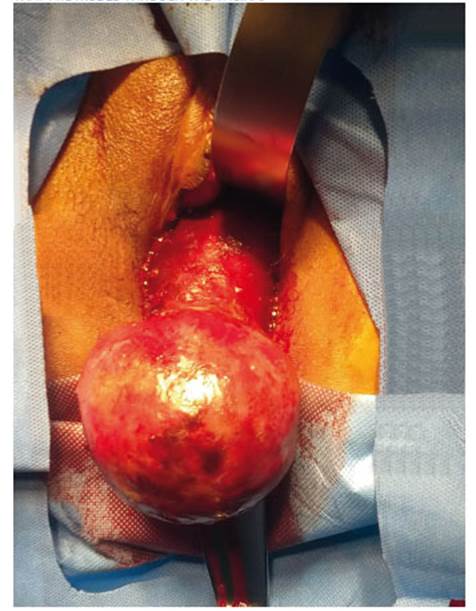
In the operating room, a bimanual examination was performed under anesthesia, showing a fleshy mass with a sessile base, 10 cm in diameter, with superficial bleeding, which protruded through the external genitalia and continued with endometrial-like tissue; neither the endocervical canal nor a pedicle was evident (Figure 1). Given the high suspicion of a fundal submucous leiomyoma associated with uterine inversion, it was decided to schedule the patient for vaginal leiomyomectomy plus exploratory laparotomy, due to the difficulty in returning the uterus to its anatomical position.
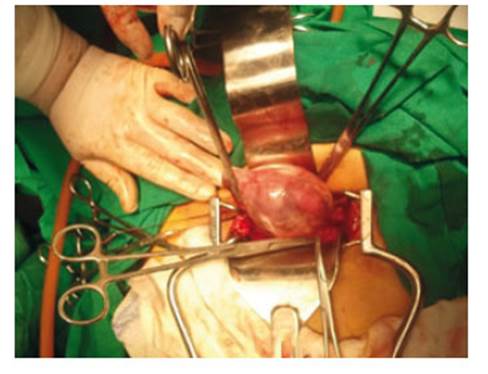
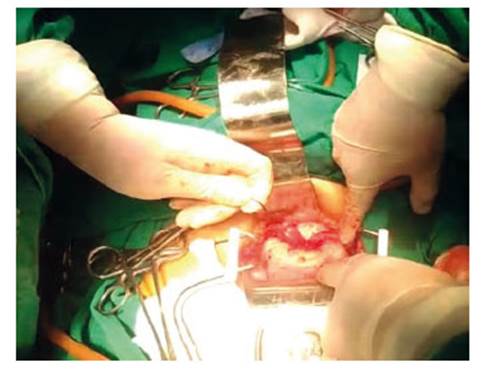
During the abdominal approach, the absence of uterus in the abdominal cavity and a defect in the pelvic excavation (pericervical ring of 3 cm in diameter) through which the uterus, round ligaments and tubes were introduced were confirmed (Figure 2). An attempt was made to reposition the uterus to its anatomical position by alternating traction of the round ligaments (Huntington procedure), with the aid of vaginal compression, without favorable results. Finally, an incision was made in the posterior fundus of the vaginal sac to section the constriction ring, applying vaginal compression. This allowed the uterus to return to its anatomical position, showing signs of tissue hypoxia (Figure 3). Subsequently, total hysterectomy with preservation of the adnexa was performed according to the usual technique. The pathological anatomy of the surgical specimen was reported as a 10 cm sessile submucosal leiomyoma, fundic location, with necrotic-hemorrhagic changes secondary to vascular injury. The patient evolved favorably and was discharged 2 days after surgery.
Disscussion
Non-puerperal uterine inversion is an infrequent episode, so much so that its incidence has not been estimated1. A report of 150 cases between 1887 and 2006 was published in 20072. In a more recent systematic review, conducted in 2018, case reports between 1940 and 2017 were analyzed, where a total of 170 cases reported worldwide were found3. There was no case reported in Peru; most were from Asia and Europe, being the average age 46 years, the most frequent cause leiomyomatosis (57.2%), followed by sarcoma (13.5%) and idiopathic causes (9.9%); they had very similar characteristics to the clinical case presented.
The pathophysiology of non-puerperal uterine inversion is not clear. Some authors4,5 describe the thinning of the uterine walls, due to the intrauterine tumor that exerts persistent and chronic traction towards the cervix, causing its dilatation after some time. Added to this, are the uterine contractions that attempt to expel the tumor, as well as increased abdominal pressure due to exertion or overweight. multiparity and advanced age6,7.
The clinical presentation is variable, most women present irregular vaginal bleeding, pelvic discomfort and a sensation of lump or pressure at the vaginal level. Also, severe dysmenorrhea, menorrhagia and dyspareunia. Hypovolemic shock8 has been reported in a case of acute uterine inversion due to uterine leiomyomatosis; also, acute urinary retention requiring catheterization9,10. The stages of uterine inversion11 are: a) Stage I, the uterine inversion is intrauterine (incomplete) and the uterine fundus remains inside the cavity; b) Stage II, complete inversion involves the uterine fundus, which protrudes through the cervix; c) Stage III, complete inversion, with protrusion of the uterine fundus through the vulva; and d) Stage IV, total inversion, where the vagina is also involved. The present clinical case was a complete uterine inversion.
For the diagnosis 2 key points are considered: 1) the body and uterine fundus cannot be palpated by combined vaginal examination; 2) the cervical os is not visualized1; it is complemented with ultrasound studies, computed axial tomography or magnetic resonance imaging13,14. The latter are recommended because they have a higher degree of diagnostic certainty, since they allow detection of a U-shaped uterine cavity, an inverted and thinner uterine fundus in the sagittal section, and an image of "bull's eyes" in the axial section, as signs indicative signs of uterine inversion. In our case, the first two studies were not satisfactory, and there was no possibility of using magnetic resonance imaging. However, in emergency cases the diagnosis is usually clinical.
Regarding the treatment of non-puerperal uterine inversion, most published cases consider definitive treatment by hysterectomy3,12,15, in 86.8% of the cases, with uterine reposition being possible in a few cases, which is usually effective only in acute inversions.
In chronic cases, the surgical approach can be through the abdominal or vaginal route, with techniques described in the literature15 (abdominal: Huntington and Haultain; vaginal: Kustner and Spinelli). Each case must be individualized, since most of them are secondary to uterine tumor, usually of considerable size, which makes vaginal access difficult. Vaginal hysterectomy can be difficult due to anatomical distortion, even for expert surgeons.
REFERENCES
1. Herath R, Patabendige M, Rashid M, Wijesinghe P. Nonpuerperal uterine inversion: What the gynaecologists need to know? Review article. Gynecol Obstet Invest. 2018;83:428-36. doi:10.1159/000488089 [ Links ]
2. Gomez-Lobo V, Burch W. Nonpuerperal uterine inversion associated with an immature teratoma of the uterus in an adolescent. Obstet Gynecol. 2008;112(3):708-9 doi: 10.1097/AOG.0b013e3181864cc3. [ Links ]
3. Rosa Silva B, de Oliveira Meller F, Uggioni ML, Grande AJ, Chiaramonte Silva N, Colonetti T, Rebello JR, da Rosa MI. Non-puerperal uterine inversion: a systematic review. Gynecol Obstet Invest. 2018;83:428-36. doi: 10.1159/000488089 [ Links ]
4. De Vries M, Perquin D. Non-puerperal uterine inversion due to submucous myoma in a young woman: a case report. J Med Case Rep. 2010;24(4):21. doi: 10.1186/1752-1947-4-21 [ Links ]
5. Takano K, Ichikawa Y, Tsunoda H, Nishida M. Uterine inversion caused by uterine sarcoma: a case report. Jpn J Clin Onc. 2001;3:39-42. doi: 10.1093/jjco/hye002 [ Links ]
6. Rathod S, Samal SK, Pallavee P, Ghose S. Non puerperal uterine inversion in a young female- a case report. J Clin Diagn Res. 2014; 8(9):OD01-OD02. doi: 10.7860/jcdr/2014/8961.4826 [ Links ]
7. Birge, O Tekin, B Merdin, A. Chronic total uterine inversion in a young adult patient. Am J Case Rep. 2015;16:756-9. doi: 10.12659/AJCR.894264 [ Links ]
8. Song YJ, Yang J, Yun HS, Lee SK, Kim HG, Lee DH, Choi OH, Na YJ. Non-puerperal uterine inversion presented with hypovolemic shock. J Menopausal Med. 2016; 22(3):184-7. doi: 10.6118/jmm.2016.22.3.184 [ Links ]
9. Chen Y, Chen CH, Cheng W, Huang Ch, Chang Ch, Lee Ch, Hsieh Ch. Submucous myoma induces uterine inversion. Taiwan J Obstet Gynecol. 2006;45:159-61. doi: 10.1016/S1028-4559(09)60216-3 [ Links ]
10. Ashraf-Ganjooie Y. Nonpuerperal uterine inversion: a case report. Int J Rep Obster Gynecol. 2017;4(4):1223-6. doi: 10.18203/2320-1770.ijrcog20150464 [ Links ]
11. Saxena R, Shah T, Thirumalappa S. Technique of abdominal hysterectomy for non-puerperal uterine inversion. BMJ Case Rep. 2011. doi: 10.1136/bcr.01.2011.3729 [ Links ]
12. Auber M, Darwish B, Lefebure A, Ness J, Roman H. Management of nonpuerperal uterine inver- sion using a combined laparoscopic and vaginal approach. Am J Obstet Gynecol. 2011;204:e7-e9. doi: 10.1016/j.ajog.2011.01.024 [ Links ]
13. Moulding F, Hawnaur JM. MRI of non-puerperal uterine inversion due to endometrial carcinoma. Clin Radiol. 2004;59:534-7. doi: 10.1016/j.crad.2003.11.007 [ Links ]
14. Lewin JF, Byyon PJ. MR imaging of uterine inversion. J Compt Assist Tomgr. 1989;13:357-9. doi: 10.1097/00004728-198903000-00038 [ Links ]
15. Lascarides E, Cohen M. Surgical management of non-puerperal inversion of the uterus. Obstet Gynecol. 1968; 32:376-81. PMID: 5754584. [ Links ]
Received: September 21, 2020; Accepted: November 14, 2020











 texto en
texto en