Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Ginecología y Obstetricia
On-line version ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.67 no.2 Lima Apr./Jun. 2021
http://dx.doi.org/10.31403/rpgo.v67i2313
Special article
Implementation of a mixed model of inperson and virtual prenatal care during the COVID-19 pandemic at the National Maternal Perinatal Institute in Lima- Peru
1. Instituto Nacional Materno Perinatal, Lima, Perú
2. Universidad Nacional Mayor de San Marcos, Lima, Perú
3. Universidad Peruana Cayetano Heredia, Lima-Perú
The coronavirus 19 (COVID-19) pandemic and the measures implemented for its control meant the interruption of prenatal care, with potential risk to maternal and fetal health. However, conventional in-person prenatal care would imply exposure and risk of infection in patients and health care providers. The Instituto Nacional Materno Perinatal (INMP) has incorporated teleconsultation as part of a new model of mixed prenatal care, which aims to reduce in-person appointments and, therefore, the contact and risk of viral transmission. The prenatal care package performs essential activities to care for pregnant women of specific gestational ages with a greater impact on perinatal and maternal outcomes. This new model could be generalized nationally and be part of the solution to the disparities of healthcare in Peru, through policies for the use of telemedicine in prenatal care that facilitate its implementation, as well as its sustainability after the COVID-19 pandemic.
Key words: Telemedicine; Remote consultation; Prenatal care; Coronavirus infections; Pandemics; COVID-19
Introduction
The World Health Organization (WHO) declared COVID-19 an international public health emergency and categorized it as a pandemic in March 20201. The Peruvian government declared a national state of emergency on March 16, 2020, as a measure to prevent viral spread2. The COVID-19 pandemic and the measures put in place to control the spread of the infection, such as quarantine and social distancing3, meant the almost total interruption of outpatient prenatal care nationwide. These measures entailed a potential risk to maternal and fetal health, since prenatal care is the only means of recognizing intercurrences during pregnancy to reduce adverse outcomes4. On the other hand, in-person prenatal care requires mobilization of the patient, accompaniment of family members, and interaction with people in hospital environments5, which generates risk of exposure and contagion of COVID-19 in the pregnant women with potential occurrence of adverse perinatal outcomes6.
Telemedicine is the provision of healthcare services using information and communication technology with potential benefit in overcoming barriers to health care delivery in the context of disasters7. In the current pandemic scenario, telemedicine can complement health care delivery when in-person visits are difficult5, as reported in several international experiences and recommendations of the American College of Obstetrics and Gynecology (ACOG) and the Society for Maternal Fetal Medicine8-10. The National Maternal Perinatal Institute (INMP), a national reference center in gynecological-obstetric pathology, has incorporated teleconsultation as part of prenatal care in a new system of outpatient care for pregnant women, with the aim of reducing the number of in-person appointments and, therefore, the contact and risk of viral transmission.
The objective of this article is to describe the characteristics and organization of the new mixed model of prenatal care using telemedicine at the INMP, facilitating social distancing in the context of the COVID-19 pandemic.
The traditional prenatal care model
Prenatal care is an important public health intervention and is based on expert opinion and tradition rather than scientific evidence11-13. The specific benefits of this model have not been demonstrated in randomized clinical trials and its efficacy is not entirely clear14; however, it is widely accepted by the health system and pregnant women15. The traditional model considers differentiated schemes for pregnant women according to risk factors. In low-risk patients, evaluations are recommended to be made every 4 weeks until the 28th week, then every 2 weeks until the 36th week, and then weekly until delivery. Women with risk factors receive additional visits that can reach more than 14, whose objective is to increase fetal and maternal monitoring with clinical evaluations together with endocrinology, cardiology and laboratory, in addition to vaccination, education, and counseling16,17.
Currently, it is suggested to prioritize the essential elements of the antenatal care package and thus provide more effective care with fewer, but ‘targeted’ visits, especially focusing on those components of prenatal care that have been demonstrated an impact on maternal and perinatal outcomes18. Nicolaides suggests that improvement in perinatal outcomes could be achieved by reversing prenatal care pyramid based on prioritizing the results of comprehensive assessment between weeks 11 and 13 weeks. In this evaluation, patients would be classified according to the risk of complications; subsequent monitoring would be guided by these factors19.
Effects of the covid-19 pandemic on prenatal care
The COVID-19 pandemic presents as a barrier to the continuity of prenatal care, putting maternal health and the possibility of increased adverse fetal outcomes at risk. The quarantine and immobilization implemented by the Peruvian government in March 2020 meant that outpatient prenatal care provided by the INMP and all other health institutions was completely interrupted. Measures such as social distancing and isolation increased barriers to transportation and mobilization and the possibility of in-person medical evaluation. Health personnel with some risk factors were identified and sent home as a rapid response to protect them from spread of COVID-19 infection. Thus, health policies and practices in response to this new social reality have impacted prenatal care by limiting the scope of care in health facilities and decreasing the number of trained staff20.
Telemedicine in prenatal care
Several experiences have been published with new models of prenatal care using telemedicine as a valid option that provides flexibility to the patient, with positive maternal and fetal outcomes and great satisfaction of the pregnant woman8. Vivanti et al21 and y Peahl et al22 describe recommendations for the follow-up of pregnant women during the SARS-Cov-2 pandemic. They propose structuring it around three main ultrasounds and offering remote or in-person follow-up depending on the obstetric risk. Aziz et al5 suggested individualizing care by incorporating telemedicine into the ACOG recommendations; this would reduce the risk of acquiring SARS-Cov-2 during mobilization to an in-person visit.
Evidence suggests that telemedicine provides health outcomes comparable to traditional methods without compromising the doctor-patient relationship and improving patient satisfaction and participation23-25. ACOG considers increasing the use of telemedicine in various aspects of obstetrics and gynecology and therefore the specialist and other health care providers should become familiar with and adapt in this technological tool. However, these technology-enhanced health care delivery opportunities will not totally replace the current standard of care9.
In the scenario of the COVID-19 pandemic in Peru, virtual consultation via telephone was integrated by the INMP for the follow-up of pregnant women26. According to supreme decree DS-Nº 005-2021-SA, teleconsultation is defined as the remote consultation between a health professional and a user through the use of information and communication technologies, for the purposes of promotion, prevention, diagnosis, treatment, recovery, rehabilitation, and palliative care27.
This system was initiated in May 2020 and until December 2020, 9 007 teleconsultations and 1 230 in-person consultations were provided to obstetric patients. This included evaluations by obstetrics-gynecology, cardiology, endocrinology, internal medicine, and infectious diseases28, and allowed us to continue with counseling, identification and prevention of adverse out-comes in high-risk pregnancies.
New mixed prenatal care sceme in the covid-19 pandemic scenario
As of August 2020, mixed prenatal care began at the INMP, combining in-person visits with telephone teleconsultation. The design of this new system of care requires the coordination of various directorates and departments of the Institute, such as the executive direction of obstetrics and gynecology (DEOG), department of obstetrics and perinatology, outpatient ser vice, statistics and informatics office, and the admission office. Health care providers were trained in the use of the ministry of health MINSA-supplied electronic health records (Integrated Hospital Management System SISGA LEN PLUS). In addition, informatic technology staff is available daily to solve problems and doubts with the system, even remotely.
Logistics and administrative procedures for mixed prenatal care at the INMP
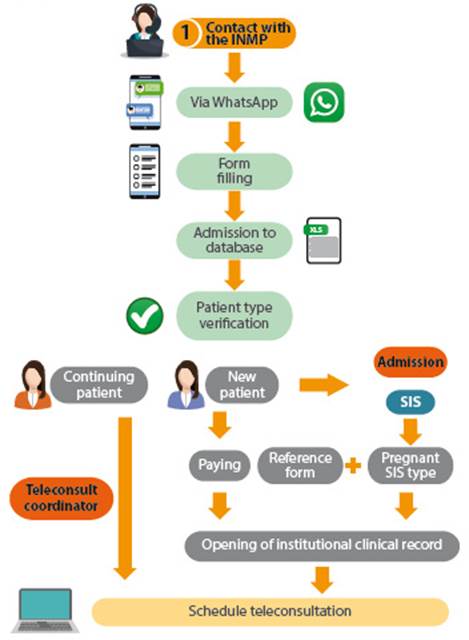
Access to prenatal care requires an administrative procedure that is carried out through telephone contact (Figure 1). The patient requests care via WhatsApp message to the telephone numbers provided on social networks and the INMP website. A form is filled out with personal data and type of health insurance, and the admission office corroborates the information sent through telephone communication with the patient. In continuing patients, the scheduling of the first virtual consultation is carried out. New patients require comprehensive health insurance (SIS) for pregnant women (80% of INMP patients have it) and a referral form from the health institution of origin. With both requirements, the medical record is opened and the first virtual consultation is scheduled. If the patient does not have SIS, she will pay for her care at Banco de la Nación agents to the INMP current account and send the payment voucher to start the care.
Mixed prenatal care flowchart
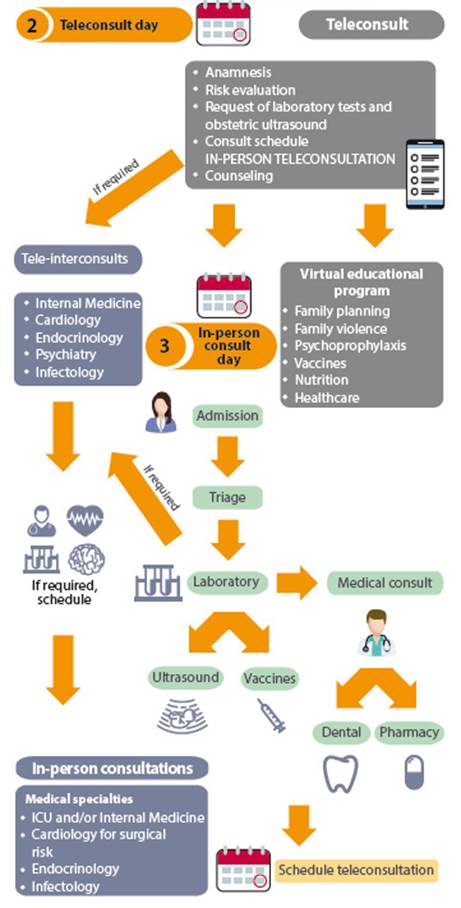
The flow of mixed prenatal care at the INMP is described in Figure 2. Prior to the virtual consultation, the prenatal care coordinators send informed consent forms to be filled out and signed by the patient26. Previous analyses and ultrasound scans are requested, which are sent to the physician in charge of the teleconsultation. Patients are scheduled and assigned. The gynecologists who perform teleconsultation are those who were sent home because they have risk factors for COVID-19 infection. Each physician working remotely has access to their patients’ electronic medical records through a link to SISGALEN PLUS.
On the day of the teleconsultation appointment, the scheduled physician makes a telephone call to the corresponding pregnant woman. According to the gestational age, a care package specified in Table 1 is applied to the patient’s first visit. The first teleconsultation service includes verifying the pregnancy diagnosis and taking the medical history in the prenatal care module of SISGALEN PLUS. According to the gestational age and risk factors, laboratory tests and the corresponding type of ultrasound are requested. An educational program is applied to all patients, including family planning, violence exclusion, immunizations, psychoprophylaxis (childbirth preparation exercises), prenatal stimulation, nutrition, health care, and alarm signs and symptoms of pregnancy and COVID-19. At the end of the teleconsultation, the physician schedules the next appointment for in-person evaluation to continue with the next teleconsultation. According to the patients’ needs, teleconsultations with specialties such as internal medicine, cardiology, endocrinology, psychiatry or infectious disease are scheduled.
Table 1 Prenatal check-up schedule according to gestational age.
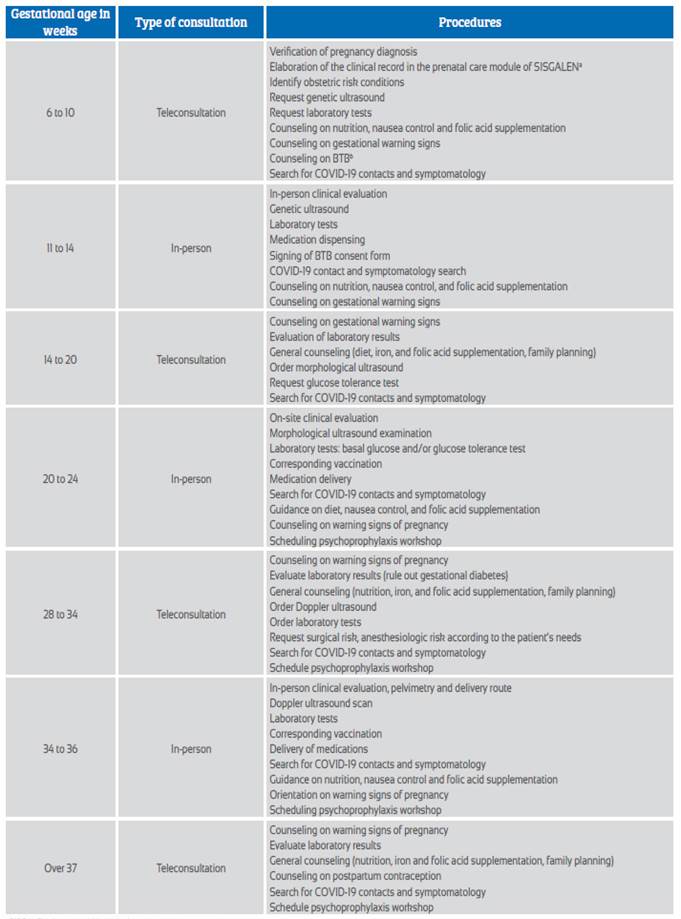
a SISGALEN: Integrated hospital management system
b BTB: bilateral tubal ligation
The in-person service at the INMP is structured to achieve the completion of scheduled activities on the same day. A maximum of 10 patients are seen per office per day and 25 minutes of consultation per patient. The appointment ticket is previously sent to the patient by email or WhatsApp, where the date and time of the appointment, that will serve as a safe-conduct for transit. The patients cited are on the list at the entrance of the institution and enter wearing masks, face shields and unaccompanied. Their temperature is taken and social distancing is maintained. After opening the manual clinical history, weight and height are assessed in the triage module. Patients are sent to a medical consultation with the obstetrician-gynecologist, clinical laboratory, fetal medicine for ultrasound, vaccination and dental evaluation, until all the activities scheduled in the teleconsultation are completed. The patient can access an in-person consultation on the same day if required. At the end of the evaluations, medications are collected from the pharmacy and the next teleconsultation appointment is scheduled according to the established scheme.
High-risk pregnant women may require an in-crease in the frequency of in-person evaluations, as well as ultrasound and laboratory tests. Risks considered include hypertensive disease of pregnancy, gestational or pre-gestational diabetes, history of prematurity or stillbirth, fetal conditions such as intrauterine growth restriction, multiple pregnancy, congenital anomalies among others.
Limitations and strengths
The major limitation in this new model of prenatal care is the accessibility of patients to the institution, due to the weaknesses of our referral system. A large number of high-risk pregnant women who request care cannot be seen because they do not have a referral from their center of origin. Additionally, it is necessary to establish a greater number of on-site clinics to cover the institutional demand that has increased in recent months (40 new patients request care per week).
The great strength in the change of the prenatal care model is the rapid adaptation of medical specialists and health care providers to the use of telemedicine in patient care, despite their lack of knowledge in the use of the technology and initial resistance to change. Currently, they are very satisfied with the system and patient loyalty. It has been possible to detect pregnancy complications early and to prepare patients for elective cesarean sections, in appropriate cases. In addition, teleconsultation has improved the quality of care due to improvements in the educational and health prevention program.
Future considerations
Peru faces multiple challenges in the field of health care. One of them is accessibility due to geographical, cultural, and socioeconomic barriers. The use of telemedicine could be part of the solution to health disparities. Thus, this mixed model of prenatal care could be generalized at the national level with individualized adaptation to each health institution. To do so, standardized policies and guidelines for telemedicine use at the national level are required to facilitate its implementation, improvement, and sustainability after the COVID-19 pandemic. And they have the potential to improve access to and use of prenatal care throughout Peru.
The unexpected situation of the COVID-19 pandemic has been the impetus for improvements and changes in the institutional health care system. The digitization of the clinical history in outpatient consultation was a necessity that was quickly implemented and allowed the connectivity of remote care by teleconsultation and in-person consultation, as well as between specialties. It is still necessary to implement the electronic medical record in all the services of the institution, in order to obtain a single, digitized system.
The INMP is currently implementing and validating the new prenatal care module that collects detailed data from the obstetric medical history. This will allow for faster patient care and use of this information for the digitization of the prenatal control card, as well as for various uses such as research. The INMP, in a joint project co-financed by the National Council for Science, Technology and Technological Innovation (CONCYTEC), is developing a mobile application for pregnant women and physicians, which will allow access to the prenatal control scheme, card and important pregnancy information, and will also serve as quality control of the care provided. This application has a traffic light system to evaluate compliance with the programmed care package according to gestational age.
Conclusions
The new mixed model of prenatal care has been implemented at the INMP to reduce the exposure of the pregnant woman and healthcare personnel to COVID-19, and uses teleconsultation with an electronic medical record system as an important tool. This model of care has a scheme based on the essential services offered in the prenatal package and has demonstrated an impact on perinatal and maternal outcomes. The use of telemedicine in Peru could contribute to solving health accessibility disparities in our country.
REFERENCES
1. World Health Organization. Cumulative COVID-19 cases reported by countries and territories in the Americas, 2020 [Internet]. USA: WHO; 2020. [citado el 21 de febrero de 2020]. Disponible en: https://who.maps.arcgis.com/apps/webappviewer/index.html?id=2203b04c3a- 5f486685a15482a0d97a87&extent=-17277700.8881%2C-104 3174.5225%2C-1770156.5897%2C6979655.9663%2C102100 [ Links ]
2. Decreto Supremo que declara Estado de Emergencia Nacional por las graves circunstancias que afectan la vida de la Nación a consecuencia del brote del COVID-19 [Internet]. Diario El Peruano. [citado el 21 de febrero de 2020]. Disponible en: https://busquedas.elperuano.pe/normaslegales/decreto-supremo-que-declara-estado-de-emergencia-nacional- po-decreto-supremo-n-044-2020-pcm-1864948-2/ [ Links ]
3. Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. 2020;27(2). DOI: 10.1093/jtm/taaa020 [ Links ]
4. Walker DS, McCully L, Vest V. Evidence-based prenatal care visits: When less is more. J Midwifery Womens Health. 2001;46(3):146-51. DOI: 10.1016/s1526-9523(01)00120-9 [ Links ]
5. Aziz A, Zork N, Aubey JJ, Baptiste CD, D'Alton ME, Emeruwa UN, et al. Telehealth for High-Risk Pregnancies in the setting of the COVID-19 pandemic. Am J Perinatol. 2020. DOI: 10.1055/s-0040-1712121 [ Links ]
6. Novoa RH, Quintana W, Llancarí P, Urbina-Quispe K, Guevara- Ríos E, Ventura W. Maternal clinical characteristics and perinatal outcomes among pregnant women with Coronavirus Disease 2019. A systematic review. Travel Med Infect Dis. 2020:101919. DOI: 10.1016/j.tmaid.2020.101919 [ Links ]
7. Lurie N, Carr BG. The role of telehealth in the medical response to disasters. JAMA Intern Med. 2018;178(6):745-6. DOI: 10.1001/jamainternmed.2018.1314 [ Links ]
8. Butler Tobah YS, LeBlanc A, Branda ME, Inselman JW, Morris MA, Ridgeway JL, et al. Randomized comparison of a reduced-visit prenatal care model enhanced with remote monitoring. Am J Obstet Gynecol. 2019;221(6):638.e1-.e8. DOI: 10.1016/j.ajog.2019.06.034 [ Links ]
9. Implementing Telehealth in Practice: ACOG Committee Opinion Summary, Number 798. Obstet Gynecol. 2020;135(2):493-4. DOI: 10.1097/AOG.0000000000003672 [ Links ]
10. Dotters-Katz S, Hughes B. Society for Maternal fetal medicine. Coronavirus (COVID-19) and pregnancy: what maternal- fetal medicine subspecialists need to know. 2020. Disponible en: https://www.fetalhealthfoundation.org/wp-content/uploads/2020/03/COVID19_PDF.pdf [ Links ]
11. Rosen MG, Merkatz IR, Hill JG. Caring for our future: a report by the expert panel on the content of prenatal care. Obstet Gynecol. [Internet]. 1991 [citado el 02 de marzo de 2021];77(5):782-7. Disponible en: https://europepmc.org/article/med/2014096 [ Links ]
12. Carter EB, Tuuli MG, Caughey AB, Odibo AO, Macones GA, Cahill AG. Number of prenatal visits and pregnancy outcomes in low-risk women. J Perinatol. 2016;36(3):178-81. DOI: 10.1038/jp.2015.183 [ Links ]
13. Okley A. The origins and development of antenatal care. En: Effectiveness and satisfaction in antenatal care. [Internet] Spastics International Medical Publications/William Heinemann Medical Books, London, 1982. p. 1-21. [citado el 02 de marzo de 2021] Disponible en: https://books. google.es/books?hl=es&lr=&id=fVH-JYbe2isC&oi=fnd&pg= PA1&dq=The+origins+and+development+of+antenatal+ care&ots=WYSvx6ANnU&sig=M6qvumboEJW8PWyee- BR9g-ybsHg#v=onepage&q=The%20origins%20and%20 development%20of%20antenatal%20care&f=false [ Links ]
14. Alexander GR, Kotelchuck M. Assessing the role and effectiveness of prenatal care: history, challenges, and directions for future research. Public Health Rep. 2001;116(4):306. DOI: 10.1016/S0033-3549(04)50052-3 [ Links ]
15. Baldwin L-M, Raine T, Jenkins LD, Hart LG, Rosenblatt R. Do providers adhere to ACOG standards? The case of prenatal care. Obstet Gynecol. [Internet]. 1994 [citado el 02 de marzo de 2021];84(4):549-56. Disponible en: https://europepmc.org/article/med/8090392 [ Links ]
16. American College of Obstetricians and Gynecologists. Guidelenes for perinatal care. American Academy of Pediatrics and the American College of Obstetricians and Gynecologists. Eighth edition. Washington, DC; ACOG: 2017. [ Links ]
17. Ministerio de Salud. Norma Técnica de Salud para la Atención Integral de Salud Materna, aprobada por Resolución Ministerial N° 827-2013/MINSA. Lima-Perú: MINSA; 2013. Disponible en: https://www.gob.pe/institucion/minsa/normas-legales/198935-2013-minsa [ Links ]
18. Dowswell T, Carroli G, Duley L, Gates S, Gülmezoglu AM, Khan-Neelofur D, et al. Alternative versus standard packages of antenatal care for low-risk pregnancy. Cochrane Database Syst Rev. 2015(7):CD000934. DOI: 10.1002/14651858.CD000934.pub2 [ Links ]
19. Nicolaides KH. A model for a new pyramid of prenatal care based on the 11 to 13 weeks' assessment. Prenat Diagn. 2011; 31(1):3-6. DOI: 10.1002/pd.2685 [ Links ]
20. Fryer K, Delgado A, Foti T, Reid CN, Marshall J. Implementation of obstetric telehealth during COVID-19 and beyond. Matern Child Health J. 2020;24(9):1104-10. DOI: 10.1007/s10995-020-02967-7 [ Links ]
21. Vivanti AJ, Deruelle P, Picone O, Guillaume S, Roze J-C, Mulin B, et al. Follow-up for pregnant women during the COVID-19 pandemic: French national authority for health recommendations. J Gynecol Obstet Hum Reprod. 2020:101804. DOI: 10.1016/j.jogoh.2020.101804 [ Links ]
22. Peahl AF, Smith RD, Moniz MH. Prenatal care redesign: Creating flexible maternity care models through virtual care. Am J Obstet Gynecol. 2020;223(3):389.e1-389.e10. DOI: 10.1016/j.ajog.2020.05.029 [ Links ]
23. Pflugeisen BM, McCarren C, Poore S, Carlile M, Schroeder R. Virtual visits: Managing prenatal care with modern technology. MCN Am J Matern Child Nurs. 2016;41(1):24-30. DOI: 10.1097/NMC.0000000000000199 [ Links ]
24. Pflugeisen BM, Mou J. Patient satisfaction with virtual obstetric care. Matern Child Health J. 2017;21(7):1544-51. DOI: 10.1007/s10995-017-2284-1 [ Links ]
25. DeNicola N, Grossman D, Marko K, Sonalkar S, Tobah YSB, Ganju N, et al. Telehealth interventions to improve obstetric and gynecologic health outcomes: a systematic review. Obstet Gynecol. 2020;135(2):371. DOI: 10.1097/AOG.0000000000003646 [ Links ]
26. Instituto Nacional Materno Perinatal. Resolución Directoral N° 099-2020-DG-INMP/MINSA. Plan de emergencia COVID-19 Telesalud, Teleorientacion para la atención de pacientes de bajo riesgo y atención presencial restringida para pacientes con riesgo de complicación, del Instituto Nacional Materno Perinatal. Lima-Perú: INMP; 2020. Disponible en: https://www.gob.pe/institucion/inmp/normaslegales/1204368-099-2020-dg-inmp-minsa [ Links ]
27. Ministerio de Salud. Decreto Supremo Nº 005-2021-SA que aprueba el Reglamento de la Ley Nº 30421, Ley Marco de Telesalud, y del Decreto Legislativo Nº 1490, Decreto Legislativo que fortalece los alcances de la Telesalud. Lima-Perú: MINSA; 2021. Disponible en: https://www.gob.pe/institucion/presidencia/normas-legales/1599291-005-2021-sa [ Links ]
28. Instituto Nacional Materno Perinatal. Oficina de Estadística e Informática del Instituto Nacional Materno Perinatal. Lima-Perú, INMP; 2020. [ Links ]
Cite as: Meza-Santibañez L, Novoa RH, Torres-Osorio J, Jáuregui-Canchari V, Rodríguez-Hilario N, Guevara-Ríos E, Huang-Yang X, Ventura Laveriano W. Implementation of a mixed model of in-person and virtual prenatal care during the COVID-19 pandemic at the National Maternal Perinatal Institute in Lima-Peru. Rev Peru Ginecol Obstet. 2021;67(2). DOI: https://doi.org/10.31403/rpgo.v67i2313
Received: March 20, 2021; Accepted: April 06, 2021











 text in
text in