Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.67 no.2 Lima abr./jun. 2021
http://dx.doi.org/10.31403/rpgo.v67i2320
Caso clínico
Diagnosis and multidisciplinary management of bladder endometriosis: A case report
1. Gynecologist Obstetrician, Clínica Internacional, Endometriosis and Pelvic Pain Advanced Diagnosis Center, Lima, Peru
2. Gynecologist Obstetrician, Clínica Santa Isabel, Lima, Peru
3. Urologist, Clínica Delgado - AUNA, Lima, Peru
Bladder endometriosis is a rare medical entity, diagnosed by clinical and imaging procedures. Transvaginal ultrasound is the first line technique for diagnosis. The treatment is laparoscopic, with good results. We present the case of a patient with this pathology, with multidisciplinary surgical approach and satisfactory evolution in the control of the disease.
Key words: Endometriosis; Ultrasonography; Laparoscopy; Cystectomy
Introducción
Deep endometriosis is defined as the presence of lesions that infiltrate more than 5 mm in depth below the surface of the peritoneum, or that compromise and distort the bowel, bladder, ureters, or vagina1-3. Blad der endometriosis (BE) consists of the presence of endometrial glands and stroma in the detrusor muscle, with the base and dome of the bladder being the most frequently affected locations4. The incidence of endometriosis of the urinary tract varies between 0.3% - 12% of patients with endometriosis, with 70% - 85% of cases corresponding to BE.
Once considered a very rare pathology, it is increasingly accepted that BE is probably underdiagnosed due to the non-specific symptoms that accompany it, such as dysuria, urgency, increased urinary frequency, suprapubic pain, bladder tenesmus, incontinence and hematuria, simulating other urological conditions such as recurrent cystitis, interstitial cystitis or chronic urethral syndrome. This non-specific presentation and insidious onset can considerably delay diagnosis, resulting in increased morbidity and erroneous treatments2,5-7.
Transvaginal ultrasound (TVU) is the first-line technique for the diagnosis of BE, due to its low cost, high availability and safety profile, as it does not use ionizing radiation5. In most cases it does not require complementation with other imaging techniques to make the diagnosis8,9. In recent years, the International Deep Endometriosis Analysis (IDEA) group has published a consensus document10 to standardize the ultrasonographic evaluation of the pelvis in women with suspected deep endometriosis. This publication is currently a guide to the systematic evaluation of the anterior and posterior compartments of the pelvis that allow the diagnosis and mapping of deep endometriosis lesions using TVU.
The treatment of BE is controversial. Being a rather rare condition, it is practically unfeasible to perform randomized studies. The type of treatment may depend on several factors, such as age, fertility expectancy, extent of the disease, severity of urinary symptoms, presence of other pelvic lesions and the degree of menstrual dysfunction. Treatment may be medical, surgical or a combination of both5. In this work we present our experience in the diagnosis and management of a case of BE using a multidisciplinary approach, with satisfactory results for disease control.
Clinical case
The 34-year-old patient was attended in a first consultation with an illness of approximately 6 months, characterized by pollakiuria, hypogastric pain, dyspareunia and mild dysmenorrhea. Physical examination revealed ill-defined pelvic pain, without palpable masses. A conventional TVU showed a 7 cm bilobated cystic formation in the right ovary, a 4 cm cyst with internal echoes in the left ovary and an intramural myoma. A urine culture was requested, the result of which was negative. Laparoscopy was performed finding severe endometriosis, obliterated posterior cul-de-sac, bilateral ovarian endometriomas and a possible endometriotic bladder lesion. Surgical wedge removal was performed on both ovaries and relea-se of adhesions. Postoperatively, treatment with GnRH analogue was indicated for 3 months.
Six months after surgery, the patient came for follow-up due to persistence of the symptoms described above. A new TVU was performed, this time using the systematic approach described by the International Deep Endometriosis Analysis (IDEA) group for ultrasonographic evaluation of the pelvis in women with suspected deep endometriosis. The examination showed the presence of hypoechogenic, heterogeneous, nodular image, located in the bladder dome, measuring 24 x 16 x 18 mm, which completely infiltrated the bladder wall, with a negative signal on color Doppler flowmetry. There was no evidence of infiltration of the vesico-uterine septum, with the presence of a positive sliding sign in the anterior compartment. In addition, ultrasound findings suggestive of adenomyosis were observed in the uterus (Figure 1-2).
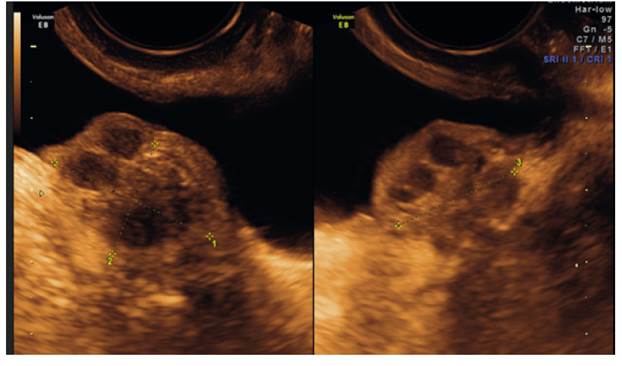
Figure 1 Sagittal and axial sections of the bladder show a hypoechogenic, heterogeneous, nodular image located in the bladder dome, measuring 24x16x18 mm, which completely infiltrates the bladder wall.
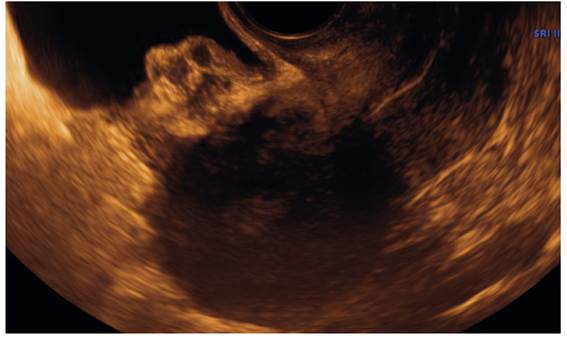
Figure 2 Sagittal section of the uterus with the bladder at half repletion showing the relationship of the endometriotic bladder implant with the uterine wall and that there is no infiltration of the vesicouterine septum. At the bimanual mobilization maneuver, the presence of the positive sliding sign was verified.
With these findings the patient was referred to the urologist for case management. An MRI was performed confirmed the presence of endometriotic implants in the fundus and anterior aspect of the bladder. In a first intervention, transurethral resection of the bladder tumor was performed, finding an exophytic tumor, mameloned with a wide base, ± 2 cm in diameter in the fundus and left lateral wall, with foci of venous hematic infiltration. The anatomopathological diagnosis was bladder mucosa with cystic glandular cystitis and presence of foci of mullerianosis (endometriosis). Subsequently, partial cystectomy was performed by laparoscopy with resection of the bladder tumor in healthy border and cystography in 2 planes. The intraoperative findings were anterior cul-de-sac occupied by a 3 cm tumor infiltrating the bladder on the left anterolateral side. The results of the pathological anatomy confirmed the presence of extensive endometriosis involving the bladder mucosa, the muscular layer and perivesical soft tissues.
The immediate postoperative period passed without intercurrences, being discharged after 24 hours with a Foley catheter, which was removed after 2 weeks. She presented urinary tract infection by Escherichia coli BLEE, which was controlled, and the patient was discharged from Urology 6 weeks after the operation.
Discussion
Endometriosis of the urinary tract is present in slightly more than 50% of cases of deep endometriosis. While the symptoms of ureteral endometriosis are nonspecific, BE symptoms help predict its location in 70% of cases5,11. It is even described that lesions at the base of the are more symptomatic than those affecting the bladder dome6. Most of the times, the clinical picture manifests as an acute urethral syndrome with increased voiding frequency, tenesmus, burning sensation, dysuria, as well as suprapubic pain and discomfort4-6,11, which coincides with the discomfort reported in the present case. The presence of hematuria and menuria has been reported only in 20%-35% of cases and are rather infrequent symptoms, due to the fact that BE rarely infiltrates the bladder mucosa producing ulcerations towards the interior of the organ5,12. Although mucosal involvement was confirmed in the anatomopathological examination, the presence of hematuria or menuria was not documented in this case.
As early as 1997, Fedele et al. stated that TVU was the ideal study for the diagnosis of BE, compared to transabdominal ultrasound and MRI13. In 2009, Savelli et al. published a series attributing a sensitivity to TVU a sensitivity of 44%, but specificity of 100%7. Similar results have been reported by different authors, finding specificity values and positive and negative predictive values very close to 100%. The sensitivity below 50% is explained by the fact that the detection rate us strongly related to the size of the lesion, with implants < 3 cm being less frequently detected by TVU5. In this case, the presence of a typical ultrasound image of heterogeneous aspect, hypoechogenic, nodular, protruding from the bladder dome towards the bladder lumen and with negative signal to color Doppler, helped to confirm the suspicion of a bladder lesion found at the first laparoscopy. The same were found on MRI. It has been pointed out that MRI could have an advantage over TVU in the detection of lesions < 2 cm, especially when an endocavitary marker is used14, so it can be considered as a second-line technique for the diagnosis of BE4,5,8. Cost is the main factor against MRI, considering that in experienced hands the diagnostic accuracy of both techniques is similar; with a great advantage for TVU in its cost-effectiveness ratio, the routine use of MRI in clinical practice for the diagnosis of BE is not recommended4,8.
Since 1999, the surgical treatment proposal for BE has been partial cystectomy by laparoscopy, with excellent clinical results15. Transurethral resection is not recommended4, unless a complementary and definitive resection is performed by laparoscopy16. In the present case, we found a patient with suggestive symptomatology, but the clinical suspicion and the first ultrasound image were insufficient, since BE was not suspected in the first instance. In the first laparoscopy the lesion was observed, but the surgical equipment was not adequate for resection. With this finding, the recurrence of the symptomatology and the second ultrasound evaluation, the patient underwent adequate multidisciplinary management with optimal results for disease control. We highlight the fact that the current recommendation is that in patients with suspected endometriosis, the study should be systematically performed to rule out bladder and urinary tract involvement10,17.
REFERENCES
1. Koninckx PR, Meuleman C, Demeyere S, Lesaffre E, Cornillie FJ. Suggestive evidence that pelvic endometriosis is a progressive disease, whereas deeply infiltrating endometriosis is associated with pelvic pain. Fertil Steril. 1991;55:759-65. [ Links ]
2. Chapron C, Fauconnier A, Vieira M, Barakat H, Dousset B, Pansini V, Vacher-Lavenu MC, Dubuisson JB. Anatomical distribution of deeply infiltrating endometriosis: surgical implications and proposition for a classification. Hum Reprod. 2003;18:157-61. [ Links ]
3. Johnson NP, Hummelshoj L, Adamson GD, Keckstein J, Taylor HS, Abrao MS, Bush D, Kiesel L, Tamimi R, Sharpe-Timms KL, Rombauts L, Giudice LC; World Endometriosis Society Sao Paulo Consortium. World Endometriosis Society consensus on the classification of endometriosis. Hum Reprod. 2017;32(2):315-24. doi: 10.1093/humrep/dew293. Epub 2016 Dec 5. PMID: 27920089 [ Links ]
4. Maggiore ULR, Ferrero S, Candiani M, Somigliana E, Viganò P, Vercellini P. Bladder endometriosis: a systematic review of pathogenesis, diagnosis, treatment, impact on fertility, and risk of malignant transformation. Eur Urol. 2017;71(5):790- 807. doi:10.1016/j.eururo.2016.12.015 [ Links ]
5. Maccagnano C, Pellucchi F, Rocchini L, Ghezzi M, Scattoni V, Montorsi F, et al. Diagnosis and treatment of bladder endometriosis: state of the art. Urol Internationalis. 2012;89(3):249-58. doi:10.1159/000339519 [ Links ]
6. Villa G, Mabrouk M, Guerrini M, Mignemi G, Montanari G, Fabbri E, Venturoli S, Seracchioli R. Relationship between site and size of bladder endometriotic nodules and severity of dysuria. J Minim Invasive Gynecol 2007;14:628-32. [ Links ]
7. Savelli L, Manuzzi L, Pollastri P, Mabrouk M, Seracchioli R, Venturoli S. Diagnostic accuracy and potential limitations of transvaginal sonography for bladder endometriosis. Ultrasound Obstet Gynecol. 2009;34:595-600. [ Links ]
8. Working group of ESGE, ESHRE, and WES, Keckstein J, Becker CM, et al. Recommendations for the surgical treatment of endometriosis. Part 2: deep endometriosis. Hum Reprod Open. 2020;2020(1):hoaa002. Published 2020 Feb 12. doi:10.1093/hropen/hoaa002 [ Links ]
9. Guerriero S, Saba L, Pascual MA, Ajossa S, Rodriguez I, Mais V, Alcazar JL. Transvaginal ultrasound vs magnetic resonance imaging for diagnosing deep infiltrating endometriosis: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2018;51:586-95. doi: 10.1002/uog.18961 [ Links ]
10. Guerriero S, Condous G, van den Bosch T, Valentin L, Leone FPG, Van Schoubroeck D, et al. Systematic approach to sonographic evaluation of the pelvis in women with suspected endometriosis, including terms, definitions and measurements: a consensus opinion from the International Deep Endometriosis Analysis (IDEA) group. Ultrasound Obstet Gynecol. 2016;48(3):318-32. doi:10.1002/uog.15955 [ Links ]
11. Knabben L, Imboden S, Fellmann B, Nirgianakis K, Kuhn A, Mueller MD. Urinary tract endometriosis in patients with deep infiltrating endometriosis: prevalence, symptoms, management, and proposal for a new clinical classification. Fertil Steril. 2015;103:147-52. DOI: 10.1016/j.fertnstert.2014.09.028 [ Links ]
12. Abrao MS, Dias JA Jr, Bellelis P, Podgaec S, Bautzer CR, Gromatsky C: Endometriosis of the ureter and bladder are not associated diseases. Fertil Steril. 2009;91:1662-7. [ Links ]
13. Fedele L, Bianchi S, Raffaelli R, Portuese A. Pre-operative assessment of bladder endometriosis. Hum Reprod. 1997;12:2519-22. [ Links ]
14. Balleyguier C, Chapron C, Dubuisson JB, Kinkel K, Fauconnier A, Vieira M, H´el´enon O, Menu Y. Comparison of magnetic resonance imaging and transvaginal ultrasonography in diagnosing bladder endometriosis. J Am Assoc Gynecol Laparosc. 2002;9:15-23. [ Links ]
15. Chapron C, Dubuisson JB. Laparoscopic management of bladder endometriosis. Acta Obstet Gynecol Scand. 1999;78:887-90. [ Links ]
16. Pang ST, Chao A, Wang CJ, Lin G, Lee CL. Transurethral partial cystectomy and laparoscopic reconstruction for the management of bladder endometriosis. Fertil Steril. 2008;90(5):2014.e1-2014.e20143. doi:10.1016/j.fertnstert.2008.04.045 [ Links ]
17. Pateman K, Holland TK, Knez J, Derdelis G, Cutner A, Saridogan E, Jurkovic D. Should a detailed ultrasound examination of the complete urinary tract be routinely performed in women with suspected pelvic endometriosis? Hum Reprod. 2015;30:2802-7. doi: 10.1093/humrep/dev246 [ Links ]
Received: January 19, 2021; Accepted: March 14, 2021











 texto en
texto en 



